Anticholinergic Burden Calculator
Add Your Medications
Added Medications:
Your Anticholinergic Burden Assessment
0
Total ACB Score
Low risk (<3): Minimal anticholinergic burden
Medium risk (3-4): Moderate risk, monitor for symptoms
High risk (5+): Significant risk of cognitive impairment and other symptoms
Combining tricyclic antidepressants (TCAs) like amitriptyline with common over-the-counter antihistamines like diphenhydramine (Benadryl) isn’t just a minor interaction-it’s a silent danger. Millions of people take these drugs together without realizing the risk. For older adults, especially, this mix can trigger confusion, memory loss, urinary retention, and even hospitalization. The problem isn’t one drug or the other. It’s what happens when they stack up: anticholinergic overload.
What Exactly Is Anticholinergic Overload?
Your body uses acetylcholine, a key neurotransmitter, to control everything from memory and attention to digestion and bladder function. Anticholinergic drugs block this chemical. Tricyclic antidepressants were designed to affect serotonin and norepinephrine, but they also strongly block acetylcholine receptors. First-generation antihistamines like diphenhydramine do the same thing-just for different reasons. When you take both, the effect isn’t just added. It multiplies.Think of it like turning up the volume on two speakers at once. Each one alone might be loud. Together, they’re deafening. The brain and body can’t handle the sudden drop in acetylcholine activity. That’s when symptoms kick in: dry mouth, blurred vision, constipation, trouble urinating, dizziness, and worst of all-confusion that looks like dementia.
Who’s Most at Risk?
People over 65 are the most vulnerable. Their livers and kidneys don’t clear drugs as quickly. They’re also more likely to be on multiple medications. But it’s not just age. Someone taking amitriptyline for nerve pain might also take diphenhydramine for allergies or sleep. That’s a common combo. A 2022 study found that 28% of anticholinergic overload cases in clinical settings involved this exact pair.Even younger people aren’t safe. A patient on amitriptyline for chronic pain and prescribed Benadryl for seasonal allergies could end up in the ER with acute delirium. One Reddit user, a medical resident, reported seeing three elderly patients admitted for sudden confusion-all traced back to TCA plus antihistamine use. Their doctors didn’t connect the dots.
How Bad Is the Risk?
The numbers don’t lie. A 2015 study in JAMA Internal Medicine found that people who took high-anticholinergic drugs for just three years had a 54% higher risk of developing dementia. The risk climbs with each additional anticholinergic drug. Amitriptyline scores a 3 on the Anticholinergic Cognitive Burden (ACB) scale-the highest possible. Diphenhydramine scores a 2. Together? A total of 5. Research shows that a score of 4 or higher doubles dementia risk.And it’s not just long-term. Even short-term use can be dangerous. A 2023 study in the Journal of the American Geriatrics Society found that just 30 days of combined exposure increased delirium risk by 200% in patients over 65. That’s not a typo. Two months of sleeping with Benadryl on top of amitriptyline could land someone in the hospital.
Which Drugs Are the Worst Offenders?
Not all antidepressants carry the same risk. TCAs are the main concern. Amitriptyline, imipramine, and clomipramine are the strongest anticholinergics in this class. Nortriptyline and desipramine are slightly safer, but still risky when combined with antihistamines.As for antihistamines, the first-generation ones are the problem. Diphenhydramine (Benadryl), hydroxyzine (Vistaril), and chlorpheniramine (Chlor-Trimeton) all have strong anticholinergic effects. Second-generation antihistamines like loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra) have almost none. They don’t cross the blood-brain barrier as easily. That makes them far safer for people on TCAs.
Here’s a quick comparison:
| Medication | Type | ACB Score | Risk Level |
|---|---|---|---|
| Amitriptyline | TCA | 3 | Very High |
| Diphenhydramine (Benadryl) | 1st-gen antihistamine | 2 | High |
| Clomipramine | TCA | 3 | Very High |
| Hydroxyzine | 1st-gen antihistamine | 2 | High |
| Loratadine (Claritin) | 2nd-gen antihistamine | 0 | Low |
| Cetirizine (Zyrtec) | 2nd-gen antihistamine | 0 | Low |
| Fluoxetine (Prozac) | SSRI | 0 | Low |
Why Do Doctors Still Prescribe This Combo?
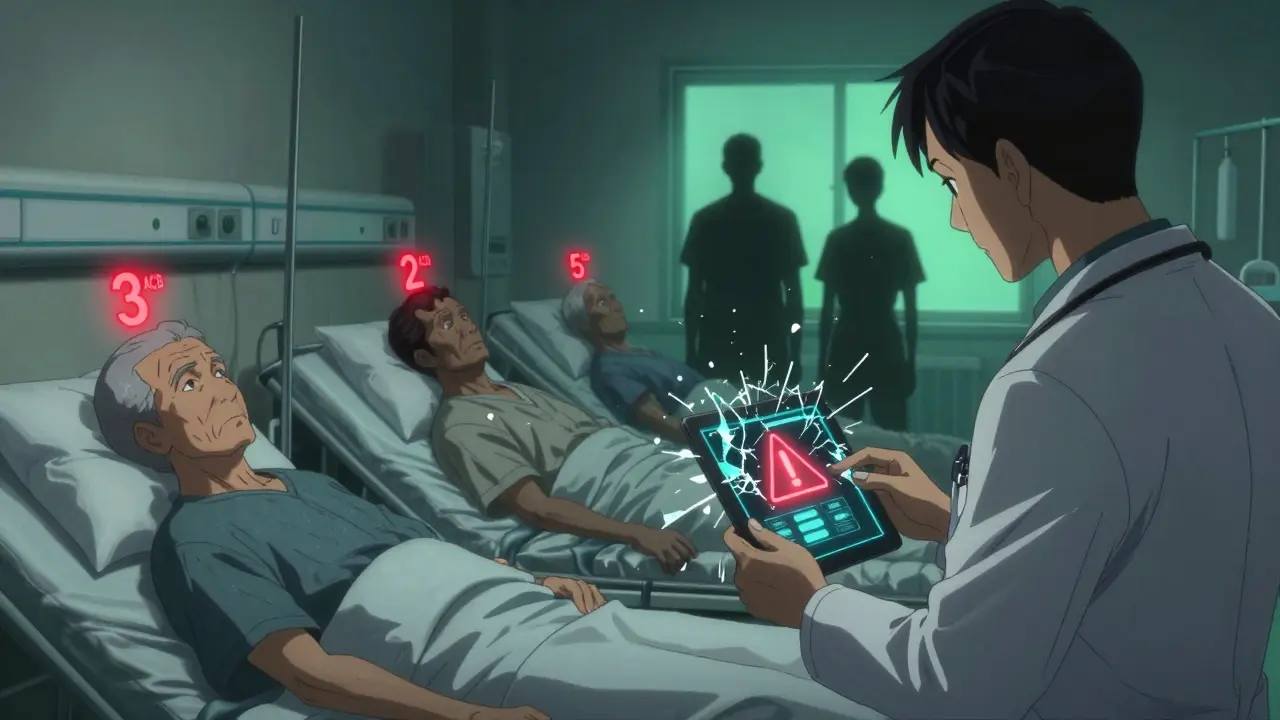
It’s not always negligence. Many patients are told to take Benadryl for sleep because it’s cheap, available, and feels like a quick fix. Doctors might not realize how strong the anticholinergic effect is-or they assume the patient isn’t taking anything else. But the data is clear: over 6,800 high-risk interaction alerts were flagged in just 3,365 patients in one 2020 study. That’s not rare. It’s routine.Electronic health records now block many of these combinations. Epic and other major systems trigger hard stops when a prescriber tries to order amitriptyline and diphenhydramine together. But not all systems are updated. And some prescribers override the alerts without realizing the long-term consequences.
What Should You Do If You’re on Both?
If you’re taking a TCA and a first-generation antihistamine, don’t stop suddenly. Talk to your doctor. Ask these questions:- Is this antihistamine necessary? Can I switch to loratadine or cetirizine?
- Is there a non-anticholinergic sleep aid I can try instead? Melatonin (0.5-5 mg) is often effective.
- Can we check my anticholinergic burden score?
- Should I get my cognitive function tested with a simple tool like the MMSE?
One patient, who called herself “ChronicPainWarrior” on a support forum, described being rushed to the ER after adding Benadryl to her amitriptyline. She had urinary retention and couldn’t think clearly. Her doctors confirmed anticholinergic toxicity. She switched to loratadine for allergies and melatonin for sleep. Within weeks, her brain fog lifted.

What Are the Alternatives?
For allergies: Stick with second-generation antihistamines. They work just as well for runny nose and sneezing without affecting your brain.For sleep: Melatonin is the safest bet. It doesn’t block acetylcholine. Trazodone (a low-dose antidepressant) is sometimes used off-label for sleep in patients on TCAs-but only under supervision. Avoid benzodiazepines like lorazepam or alprazolam. They add another layer of CNS depression and increase fall risk.
For depression: If your TCA isn’t working or causing side effects, ask about SSRIs like sertraline or escitalopram. They have far less anticholinergic activity. For nerve pain, TCAs are still first-line-but only if you’re not adding other anticholinergics.
What’s Changing in 2026?
The FDA now requires stronger warnings on all TCA and first-gen antihistamine labels. The American Geriatrics Society’s Beers Criteria explicitly says: “Avoid first-gen antihistamines in older adults taking TCAs.”More hospitals are running “anticholinergic burden audits.” In one pilot program, 41% of inappropriate TCA-antihistamine combinations were stopped within six months. Research is also moving toward genetic testing. If you’re a CYP2D6 poor metabolizer, your body can’t break down amitriptyline properly. That makes you 3.2 times more likely to overdose on it-even at normal doses.
The National Institute on Aging is funding a $2.4 million study to track long-term cognitive damage from anticholinergic accumulation. Early results suggest that even a few months of combined use can leave lasting effects.
Deprescribing-safely stopping unnecessary anticholinergics-has been shown to improve cognition by 34% in 18 months. That’s not a small gain. That’s life-changing.
Can I take Benadryl with amitriptyline if I only use it once in a while?
No. Even occasional use adds to your cumulative anticholinergic burden. The damage isn’t always immediate-it builds over time. One dose might not cause symptoms, but it contributes to long-term risk. If you need allergy relief, switch to Claritin or Zyrtec.
Are SSRIs safer than TCAs when combined with antihistamines?
Yes. SSRIs like sertraline or escitalopram have almost no anticholinergic effect. You can safely combine them with second-gen antihistamines like loratadine. But never combine SSRIs with first-gen antihistamines without checking with your doctor-some SSRIs can still interact with other drugs you’re taking.
How do I know if I’m experiencing anticholinergic overload?
Watch for sudden confusion, memory lapses, trouble speaking, urinary retention, constipation, dry mouth, blurred vision, or dizziness. If you’re on a TCA and notice any of these, especially after starting a new antihistamine, contact your doctor immediately. These aren’t normal side effects-they’re warning signs.
Is there a test to measure my anticholinergic burden?
Yes. The Anticholinergic Cognitive Burden (ACB) scale is used by clinicians to add up scores from all your medications. Amitriptyline = 3, diphenhydramine = 2. A score of 3 or higher is considered high risk. Ask your pharmacist or doctor to calculate your total score. Many now use it routinely.
Can anticholinergic damage be reversed?
In many cases, yes. Stopping the drugs can lead to noticeable improvement in cognition within weeks to months. The 2023 study in the Journal of the American Geriatrics Society showed a 34% improvement in cognitive function after deprescribing. But the longer you’ve been exposed, the slower the recovery. Early action matters.