Aminoglycoside Nephrotoxicity Risk Calculator
Risk Assessment Form
When you’re fighting a serious bacterial infection-especially one caused by drug-resistant Gram-negative bacteria-doctors sometimes turn to aminoglycoside antibiotics like gentamicin, tobramycin, or amikacin. These drugs work fast and well. But there’s a hidden cost: up to 1 in 4 people who take them will develop kidney damage. It’s not rare. It’s not unusual. It’s expected.
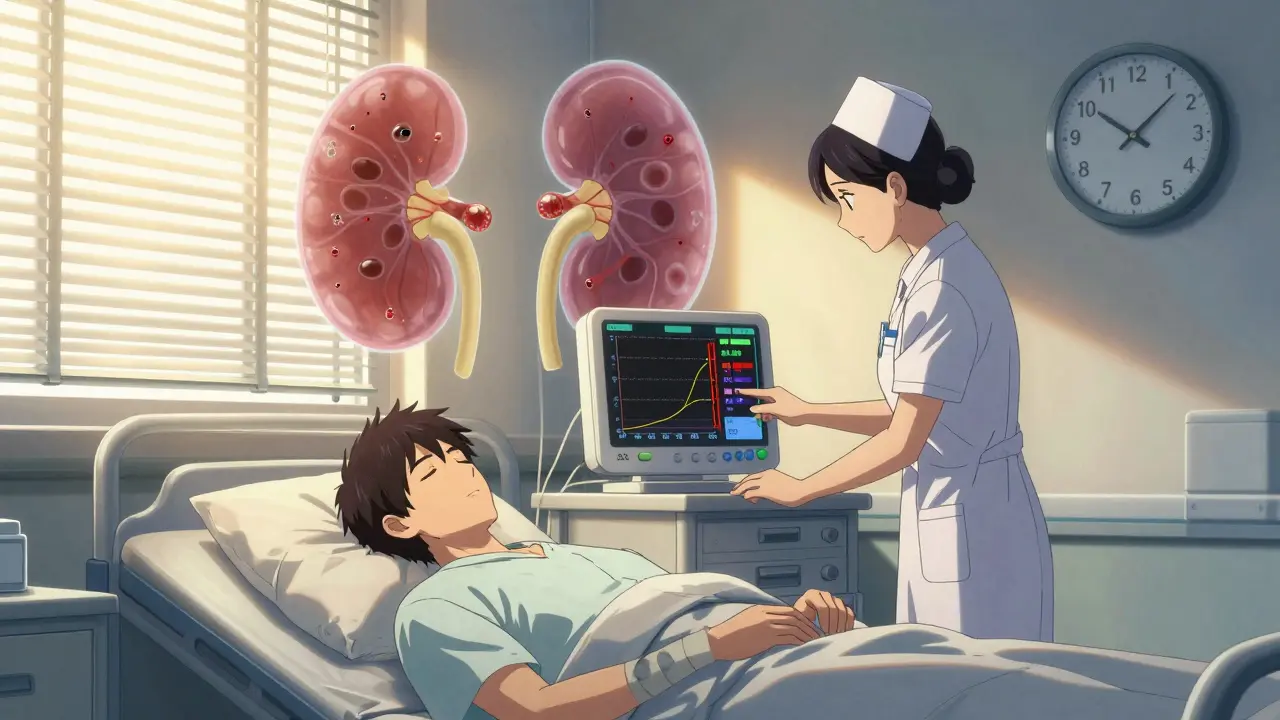
How Aminoglycosides Hurt the Kidneys
These antibiotics don’t just kill bacteria. They also stick around in your kidneys. About 5% of every dose gets trapped in the cells lining the proximal tubules-the part of the kidney that filters waste and reabsorbs nutrients. Once inside, they pile up in tiny sacs called lysosomes. Over time, these sacs swell, fill with fatty debris, and start to break down. Under a microscope, you can see them turn into myeloid bodies-dense, layered structures that shouldn’t be there.This isn’t just about clogged pipes. Aminoglycosides mess with mitochondria, the energy factories of kidney cells. They trigger oxidative stress, which leads to cell death. And it’s not just the tubules. Research from 2011 showed that these drugs also cause blood vessels in the kidney to tighten, reducing blood flow. That’s why kidney function drops even before you see obvious signs of tubule damage.
What Nephrotoxicity Looks Like
Unlike other types of kidney injury, aminoglycoside damage usually doesn’t stop urine output. You’re still peeing-often more than 400 mL a day. But your kidneys aren’t working right. Serum creatinine creeps up. It might take 5 to 7 days of treatment before it’s noticeable. A rise of 0.5 mg/dL or more from your baseline is a red flag.Early signs show up in urine tests: more sodium, potassium, magnesium, and calcium being dumped out. Proteins like beta-2-microglobulin and enzymes like N-acetylglucosaminidase appear in higher amounts. These aren’t just lab quirks-they’re the first signals that kidney cells are under siege.
Most people don’t feel sick. No pain. No swelling. That’s why monitoring matters. If your doctor doesn’t check your creatinine every 2 to 3 days while you’re on these drugs, they’re not following best practices.
Who’s at Highest Risk?
Not everyone gets kidney damage. But some people are far more likely to. If you’re over 65, your risk doubles. If you already have kidney problems-with an eGFR below 60 mL/min/1.73m²-you’re 3.2 times more likely to get injured. Taking another kidney-damaging drug, like vancomycin, pushes the risk up by 2.7 times. Dehydration? That’s another big one. Your kidneys need good blood flow to flush out toxins. If you’re low on fluids, the drugs concentrate in your tubules and do more harm.Longer treatment = higher risk. Going beyond 7 days increases the chance of permanent damage. A 2021 study of over 1,200 patients found that 18.7% developed acute kidney injury. Most recovered, but not all. About 1 in 5 had lasting kidney function loss.
Dosing Matters More Than You Think
Here’s something most patients don’t know: how often you get the drug changes your risk. Giving aminoglycosides three times a day? That’s worse than once a day. Even if the total daily dose is the same, frequent dosing leads to faster, deeper kidney injury. Why? Because your kidneys don’t get time to clear the drug between doses. It builds up.Even the time of day matters. Studies show the lowest risk of kidney damage happens when the drug is given at 1:30 p.m. Your body’s natural rhythms affect how well your kidneys handle toxins. Giving it at night or early morning might be more dangerous.
Among the drugs themselves, gentamicin is the most toxic. Amikacin is a bit gentler on the kidneys at the same dose. But no aminoglycoside is safe. They all work the same way-and they all damage the same cells.
Can You Prevent It?
There’s no magic pill to stop it. But there are proven ways to reduce the risk.- Use once-daily dosing. It’s now the standard in Europe and the U.S.
- Keep trough levels below 1 μg/mL for gentamicin. That’s the sweet spot between killing bacteria and sparing your kidneys.
- Check creatinine every 48 to 72 hours. No exceptions.
- Avoid other nephrotoxins-especially vancomycin, NSAIDs, and contrast dyes-if you can.
- Stay hydrated. Drink water. Don’t wait until you’re thirsty.
- Limit treatment to 7 days or less, unless you absolutely can’t stop.
There’s promising research on a compound called polyaspartic acid. In animal studies, it blocked aminoglycosides from sticking to kidney cells. It prevented lysosome damage, stopped phospholipid buildup, and protected kidney function completely. But it’s not approved for humans yet. Phase II trials are ongoing, but it’ll be years before it’s available.

Recovery: Is It Permanent?
The good news? Most people bounce back. After stopping the drug, kidney function usually starts improving in 3 to 5 days. Full recovery often takes 1 to 3 weeks. A study from the Mayo Clinic showed that 82% of patients recovered fully within 30 days.But not everyone. About 1 in 5 end up with lasting kidney damage. Older patients, those with pre-existing disease, or those who got the drug for more than 10 days are at higher risk of permanent loss. That’s why it’s so important to catch it early. If you wait until your creatinine is sky-high, the damage might already be irreversible.
Why We Still Use Them
You might wonder-why risk it at all? Because for some infections, there’s no better option. Drug-resistant pneumonia, sepsis from E. coli or Pseudomonas, complicated urinary tract infections in ICU patients-these are life-or-death situations. Aminoglycosides are one of the few drugs that still work.Global use? Over 12 million courses every year, according to the WHO. That’s a lot of people walking a tightrope between saving their life and damaging their kidneys. But for now, it’s the best tool we have.
Researchers are working on new versions-less toxic derivatives, targeted delivery systems, even nanoparticle carriers that skip the kidneys entirely. But those are years away. Right now, the only defense is smart prescribing, careful monitoring, and knowing the signs.
What You Should Ask Your Doctor
If you’re being prescribed an aminoglycoside, don’t wait for symptoms. Ask these questions:- Is this the best option, or is there a safer alternative?
- Will you be using once-daily dosing?
- What’s my baseline creatinine, and how often will you check it?
- What’s the target trough level for this drug?
- Am I on any other drugs that could make this worse?
- What signs should I watch for at home?
These aren’t just questions. They’re your protection. You’re not being difficult. You’re being informed.






roger dalomba December 25, 2025
So we’re just gonna keep poisoning people because ‘no better option’? Cool. Guess I’ll just sip my coffee and wait for my kidneys to turn into a lysosome graveyard. Classic medicine.
Brittany Fuhs December 26, 2025
It’s disgusting how casually doctors hand out these drugs like candy. In my country, we actually respect the human body. Here? You’re a lab rat with a Medicare card.
Sumler Luu December 28, 2025
I appreciate how thorough this breakdown is. As a nurse who’s seen this play out too many times, I’ve learned to push back when I see daily dosing ignored. It’s not just about protocols-it’s about listening to the numbers before the patient starts to suffer.
sakshi nagpal December 29, 2025
This is exactly why global health equity matters. In rural India, we often get aminoglycosides because nothing else is available or affordable. We don’t have the luxury of trough monitoring or hydration protocols. The real tragedy isn’t the toxicity-it’s the lack of alternatives.
Sandeep Jain December 31, 2025
i read this and thought of my uncle who got on gentamicin after sepsis… he was fine for a week then his creatinine shot up. doc said ‘it’s expected’ and kept going. he never fully recovered. why does ‘expected’ mean ‘acceptable’?
Sophia Daniels December 31, 2025
Oh honey, let me grab my monocle and my lab coat-because this isn’t medicine, it’s a horror show with a side of placebo hope. We’re basically doing chemical warfare on our own kidneys and calling it ‘standard of care.’ The only thing more tragic than the damage? The fact that we’ve known this for 40 years and still do it anyway.
Nikki Brown January 1, 2026
People need to stop being so careless with their health. If you’re dehydrated, you’re asking for kidney damage. No one’s forcing you to drink soda and skip water. This isn’t a conspiracy-it’s personal responsibility.
Peter sullen January 1, 2026
It is imperative to underscore, with the utmost scientific rigor, that the pharmacokinetic profile of aminoglycosides-particularly their renal tubular accumulation and mitochondrial dysfunction cascade-demands, as a non-negotiable imperative, vigilant therapeutic drug monitoring, with a mandatory emphasis on trough-level adherence, and concurrent avoidance of synergistic nephrotoxic insults.
Steven Destiny January 2, 2026
Enough with the cautionary tales. If you’re sick enough to need this drug, you don’t get to whine about side effects. You want to live? You take the hit. Period.
Fabio Raphael January 4, 2026
I wonder if polyaspartic acid could be repurposed for other nephrotoxic drugs too? Like, what if we started testing it against vancomycin or cisplatin? Maybe the mechanism is broader than we think.
Amy Lesleighter (Wales) January 5, 2026
they dont tell you this because it’s scary. but if you’re on one of these, drink water like it’s your job. and ask for the once-a-day version. it’s not magic, just common sense.
Becky Baker January 7, 2026
So basically we’re betting people’s kidneys on a roll of the dice? Thanks for the update, America.