When a new drug warning pops up, it’s not just noise-it’s a potential life-or-death signal. Every year, preventable medication errors cause tens of thousands of deaths worldwide. The good news? You don’t have to guess which updates matter. Professional societies like ISMP, ASHP, AORN, and WHO don’t just publish guidelines-they deliver real-time, evidence-based alerts that stop errors before they happen. But with so many sources, where do you even start?
Know Which Organizations Actually Move the Needle
Not all safety updates are created equal. Some are generic, some are outdated, and some are buried in PDFs no one reads. The ones that save lives come from a handful of trusted sources with proven track records.ISMP (Institute for Safe Medication Practices) is the gold standard. They don’t just report on errors-they collect them. Every week, their Medication Safety Alert! newsletter breaks down real incidents reported by hospitals and pharmacies. In 2022, they processed over 2,800 error reports. That’s not theory-it’s what actually went wrong in real clinics. Their biennial Targeted Medication Safety Best Practices are used by 87% of U.S. hospitals. If you only subscribe to one thing, make it this.
ASHP (American Society of Health-System Pharmacists) offers practical tools you can implement tomorrow. Their free Medication Safety Resource Center includes checklists, flowcharts, and self-assessments. Their premium content costs $99 a year, but if you’re in a hospital or clinic, it’s worth it. They’ve built tools to help you map out exactly where your pharmacy or unit is vulnerable.
WHO’s Medication Without Harm campaign isn’t just a slogan-it’s a global framework. Launched in 2017, it’s now active in 137 countries. Their updates focus on systemic fixes: better labeling, safer handoffs, and reducing high-risk drugs in vulnerable populations. If you work in public health or a global setting, this is your backbone.
The FDA is your regulatory alarm bell. They issue drug safety communications when something dangerous is confirmed-like a new black box warning or a recall. In 2023 alone, they issued 47 alerts. But here’s the catch: these come after harm has been detected. They’re essential, but they’re reactive. Don’t rely on them alone.
How to Subscribe Without Getting Overwhelmed
You don’t need to read every email that lands in your inbox. You need a system.Start with these three subscriptions:
- ISMP Medication Safety Alert! (Weekly, $299/year) - This is your early warning system. It’s detailed, specific, and often includes sample protocols you can copy-paste.
- FDA Drug Safety Communications (Free, email alerts) - Set this up immediately. Go to the FDA’s website, sign up for email alerts under “Drug Safety.” You’ll get notifications on label changes, recalls, and new risks.
- ASHP Medication Safety Resource Center (Free basic access) - Bookmark it. Use their self-assessment tools quarterly to see where your practice needs tightening.
For specialty areas, add these:
- AORN - If you work in surgery or perioperative care, their October 2023 update on medication safety in ORs is non-negotiable. It added new rules on labeling, tech use, and team accountability.
- ACOG - For OB/GYNs, they issue targeted alerts on high-risk drugs like oxytocin and magnesium sulfate. These aren’t just suggestions-they’re standards.
Set up filters in your email. Label ISMP alerts as “Urgent Safety,” FDA as “Regulatory,” and ASHP as “Reference.” That way, you’re not scanning everything. You’re reacting to what matters.
Turn Alerts Into Action-Not Just Reading
Reading a safety alert is useless if you don’t change how you work.Here’s how hospitals do it right:
- Assign a Medication Safety Officer - This person reads all alerts weekly, summarizes the top 2-3 actions, and shares them in a 5-minute huddle. No one has time to read 10-page PDFs. They need bullet points.
- Integrate into Training - AORN found that when updates were rolled into simulation training within 30 days, medication errors dropped by 63%. Use real cases from ISMP to train staff. Don’t just say “read this.” Say, “Here’s what happened last week. How would you have prevented it?”
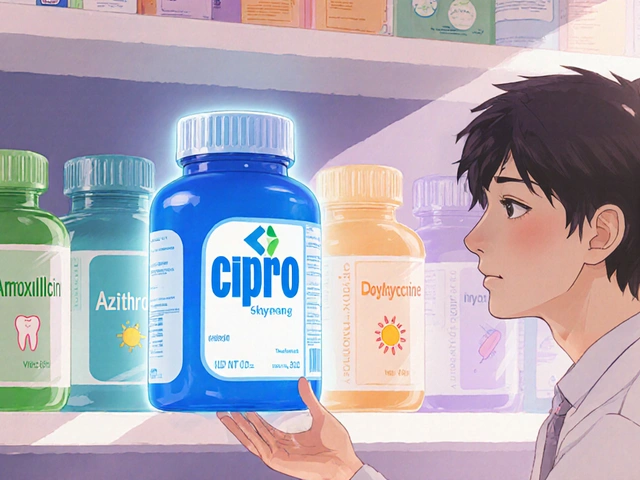
- Update Your Protocols - If ISMP says stop using “U” for units (because it looks like “0”), change your EHR templates. If the FDA warns about a new interaction with a common painkiller, update your prescribing checklist.
Don’t wait for a big audit or accreditation visit. Make safety updates part of your monthly workflow. Treat them like a checklist item-same as hand hygiene or patient ID verification.
What to Avoid-The Pitfalls That Cost Lives
Many providers think they’re staying safe because they “follow guidelines.” But here’s the truth: confusion kills.Pitfall 1: Relying on One Source - Dr. Michael Cohen, former ISMP president, said it plainly: “Relying on a single source is as dangerous as using a single verification step.” If you only watch the FDA, you’ll miss critical system-level fixes from ISMP. If you only read AORN, you won’t know about a new interaction with a drug used in primary care.
Pitfall 2: Waiting for the “Perfect” Update - Some providers delay action because they think they need the full policy, the official training module, the signed approval. You don’t. ISMP’s alerts often say, “Stop doing X.” That’s enough. Do it now. Document it later.
Pitfall 3: Ignoring the Human Factor - The biggest errors aren’t from bad drugs. They’re from tired nurses, rushed prescribers, unclear labels, and poor communication. ISMP’s best practices focus on these. Ask yourself: Are we using the same abbreviations? Are we double-checking high-alert meds? Is the barcode scanner working? Fix the system, not just the drug.
What’s Changing in 2025
The landscape is shifting fast.ISMP launched its 2024-2025 Best Practices in March, adding two new sections: one on AI-assisted prescribing and another on compounding pharmacy risks. That’s not theoretical-it’s already happening in clinics. If you’re using AI tools to generate prescriptions, you need to know how to verify them.
AORN is ditching its biennial updates. Starting in 2025, they’ll release micro-updates quarterly. That means you can’t just “review guidelines once a year.” You need to check them every three months.
WHO is rolling out new handoff tools for transitions of care-when patients move from ER to floor, or hospital to home. These are critical moments where errors spike. If you’re involved in discharge planning, pay attention.
And in late 2024, Epic and Cerner will start integrating ISMP’s best practices directly into their EHR systems. That means alerts could pop up right when you’re prescribing. It’s a game-changer. But until then, you still need to stay ahead.
Real Stories From the Front Lines
A nurse in Ohio read an ISMP alert about a mix-up between hydromorphone and morphine. She noticed her hospital was using similar-looking vials. She pushed for color-coded labels. Within two months, they had zero errors with those drugs.A pharmacist in Texas saw an FDA alert about a new interaction between a common antidepressant and a blood pressure med. He checked his pharmacy logs. Five patients were on both. He called their doctors. All five were switched safely.
On Reddit, a pharmacy tech wrote: “I implemented three changes from last month’s ISMP. One of them stopped a potential overdose before it happened. That’s why I pay for this.”
These aren’t outliers. They’re what happens when someone pays attention-and acts.
Final Checklist: Your Action Plan
Here’s what you need to do right now:- Sign up for ISMP Medication Safety Alert! (even if you have to pay for it yourself).
- Subscribe to FDA Drug Safety Communications via email.
- Bookmark ASHP’s Medication Safety Resource Center and use their self-assessment tool this quarter.
- Share one new safety tip with your team this week-even if it’s small.
- Review your facility’s medication labeling, abbreviations, and high-alert drug protocols. Are they aligned with ISMP’s latest list?
Medication safety isn’t about perfection. It’s about consistency. It’s about showing up, every week, and asking: “What could go wrong-and how do I stop it?”
The updates are out there. The tools exist. The only thing missing is your next move.
What’s the most important safety update source for a hospital pharmacist?
For hospital pharmacists, ISMP’s Medication Safety Alert! and Targeted Medication Safety Best Practices are the most critical. ISMP collects real error reports from thousands of institutions and turns them into actionable, step-by-step fixes. Their updates are used by 87% of U.S. hospitals and directly influence EHR alerts, labeling standards, and protocol changes. While FDA alerts are important for regulatory compliance, ISMP tells you how to prevent errors before they happen.
Are free safety resources reliable?
Yes-some are. The FDA’s Drug Safety Communications and ASHP’s free Medication Safety Resource Center are both authoritative and evidence-based. But free doesn’t mean comprehensive. ISMP’s paid newsletter and AORN’s updated guidelines offer deeper, more frequent, and more practical insights that free sources often lack. Think of it like this: free resources tell you what’s wrong. Paid ones tell you exactly how to fix it.
How often should I check for updates?
Check ISMP’s newsletter weekly-it’s published every Tuesday. Review FDA alerts daily if you handle high-risk medications. Check ASHP’s resource center monthly for new tools. For specialty groups like AORN or ACOG, check quarterly. Don’t wait for annual reviews. Safety moves faster than that. Treat updates like vital signs: check them regularly, record them, and act.
What if my workplace won’t pay for ISMP or ASHP subscriptions?
Many professionals pay for ISMP out of pocket because the value is clear. If your employer won’t cover it, present the ROI: one prevented error can save tens of thousands in liability and patient harm costs. Share a single ISMP alert with your manager-show how it led to a change in your unit. Use ASHP’s free tools to build your case. If you’re in a small clinic, join ISMP’s community forum (free for individuals) to access peer advice and summaries.
Do I need to follow WHO updates if I work in the U.S.?
Not daily-but yes, you should be aware. WHO’s Medication Without Harm initiative shapes global standards that eventually influence U.S. policy. Their focus on handoffs, labeling, and high-risk drug use aligns with U.S. goals. If you’re involved in policy, training, or international work, WHO’s frameworks are essential. For day-to-day practice, prioritize ISMP and FDA. But keep WHO in your awareness-it’s where the future of safety is being designed.
If you’re reading this, you’re already ahead of most providers. The next step isn’t more information-it’s action. Pick one thing from this list and do it today.





Herman Rousseau December 21, 2025
Just signed up for ISMP this week after reading this-best $299 I’ve ever spent. Got an alert about morphine/hydromorphone mix-ups and caught our pharmacy’s vial labels before anyone got hurt. 🙌
Sam Black December 22, 2025
Man, I’ve been lurking on ISMP’s forum for months-silent reader, but their stuff is pure gold. The way they break down real incidents? It’s like watching a crime scene reconstruction… except instead of blood, it’s wrong dosages and misplaced decimals. Still, I’d rather read about near-misses than live one.
Jamison Kissh December 23, 2025
I keep wondering why we treat medication safety like a checklist instead of a culture. We audit hand hygiene, we track PPE compliance-but when was the last time your team discussed how a poorly labeled syringe almost killed someone last month? The tools exist. The data’s out there. But without psychological safety to speak up, no alert matters.
Johnnie R. Bailey December 24, 2025
As someone who’s worked in rural clinics and urban hospitals, I can tell you-ISMP’s alerts are the only thing that survived the transition. FDA? Too slow. AORN? Too surgical. But ISMP? They get how messy real life is. One alert told us to stop using ‘q.d.’-we did. Two weeks later, a nurse caught a duplicate order because she remembered the ‘U’ for units thing. That’s not policy. That’s practice.
And yeah, paying for it? Worth it. My clinic didn’t have a budget, so I paid out of pocket. One prevented error covered it tenfold. Don’t wait for permission to do the right thing.
Tony Du bled December 26, 2025
Honestly? I just skim the ISMP emails and forward the ones that look scary to the pharmacist. She’s the one who actually does the work. I’m just here for the coffee and the occasional ‘oh crap’ moment.
Art Van Gelder December 27, 2025
Let’s be real-this whole system is a band-aid on a bullet wound. We’re treating symptoms while ignoring the disease: healthcare is broken. We have AI prescribing tools that hallucinate doses, EHRs that force you to click through 17 screens to change a single medication, and nurses working 16-hour shifts because staffing’s a joke. ISMP gives you a checklist to avoid drowning-but we’re still in the ocean. And the boat? Still leaking.
Don’t get me wrong-I love ISMP. But if we keep pretending that a newsletter can fix systemic collapse, we’re kidding ourselves. The real update? We need to stop treating providers like cogs and start treating them like humans with limits.
Kathryn Weymouth December 28, 2025
There’s a grammatical inconsistency in the post: ‘They don’t just report on errors-they collect them.’ The em dash is correctly used, but later, ‘They’re essential, but they’re reactive.’-the repeated contraction feels redundant. Also, ‘U’ for units should be italicized consistently. Small things, but in safety, precision matters.
Nader Bsyouni December 29, 2025
ISMP? Please. Another corporate nonprofit with a newsletter and a price tag. The FDA is the only real authority. Everything else is noise. You think a nurse in Nebraska needs to pay $300 a year to avoid a typo? Grow up.
Julie Chavassieux December 30, 2025
I’m so tired of people acting like they’re heroes for reading an email. I’ve been doing this for 20 years-and I never paid for anything. You think you’re saving lives? You’re just checking a box. Real safety? It’s in the quiet moments. The pause before you press ‘send.’ The second glance. The gut feeling. Not a newsletter.
Vikrant Sura December 31, 2025
Why are we even talking about this? Most of these alerts are obvious. Hydromorphone and morphine look different. Duh. This whole post feels like someone trying to monetize common sense.
Candy Cotton January 2, 2026
As an American citizen and licensed pharmacist, I must emphasize that only FDA-approved protocols should be followed. Any foreign or private organization promoting paid subscriptions is a threat to national healthcare integrity. This is not a matter of safety-it is a matter of sovereignty.