When you're pregnant and managing high blood pressure, the last thing you want is to accidentally harm your baby. Yet, some common blood pressure medications-ACE inhibitors and ARBs-carry serious, well-documented risks that can lead to miscarriage, kidney failure in the fetus, or even stillbirth. These drugs might have kept your blood pressure under control before pregnancy, but once you’re expecting, they become dangerous. The medical community doesn’t just warn against them-they demand immediate discontinuation.
Why ACE Inhibitors and ARBs Are Dangerous in Pregnancy
ACE inhibitors like lisinopril, enalapril, and ramipril, and ARBs like losartan and candesartan, work by blocking the renin-angiotensin-aldosterone system (RAAS). That’s great for lowering blood pressure in adults. But in a developing fetus, that same system is critical for kidney formation, amniotic fluid production, and proper blood flow to the placenta. When these drugs cross the placenta, they shut down fetal RAAS activity. The result? Severe, often irreversible damage. Studies show that exposure to these medications can cause:- Fetal kidney failure
- Oligohydramnios (dangerously low amniotic fluid)
- Lung underdevelopment due to lack of fluid
- Skeletal deformities, including skull defects
- Fetal hypotension and heart problems
- Neonatal death
ARBs May Be Even Riskier Than ACE Inhibitors
While both classes are dangerous, evidence suggests ARBs pose a higher threat. The American Heart Association’s 2012 review found that babies exposed to ARBs had worse neonatal outcomes than those exposed to ACE inhibitors. This isn’t just a small difference-it’s clinically significant. ARBs like losartan bind more tightly to fetal receptors and stay active longer in the system, increasing the duration of harm. In practice, this means if you’re on an ARB and find out you’re pregnant, your doctor needs to act faster than if you were on an ACE inhibitor. The damage isn’t just more likely-it’s more severe.What Happens If You’re Already Pregnant and Taking One of These Drugs?
If you’re currently taking an ACE inhibitor or ARB and discover you’re pregnant, do not stop abruptly without medical guidance. Sudden withdrawal can cause your blood pressure to spike, which also puts you and your baby at risk. But you also can’t keep taking the drug. The standard protocol is immediate discontinuation followed by a switch to a pregnancy-safe alternative. The American College of Obstetricians and Gynecologists (ACOG) and other major bodies agree: as soon as pregnancy is confirmed, these medications must be replaced. Your doctor will likely start you on one of three proven alternatives:- Labetalol: A beta-blocker that’s become the first-line choice. It works quickly, has minimal side effects on the fetus, and has been used safely since the 1980s. Doses typically start at 100mg twice daily and can be increased up to 2,400mg per day.
- Methyldopa: The gold standard for long-term safety. Used since the 1970s, it’s the most studied antihypertensive in pregnancy. It’s gentle on the baby, doesn’t cross the placenta in large amounts, and has no known link to birth defects. Starting dose is usually 250mg twice daily, with adjustments based on response.
- Nifedipine: A calcium channel blocker used as a second-line option. It’s effective, especially for sudden spikes in blood pressure. But it’s used cautiously in women with heart conditions because it can weaken heart muscle contractions.

What About Planning a Pregnancy?
If you’re on an ACE inhibitor or ARB and thinking about getting pregnant, don’t wait until you miss a period. Talk to your doctor now. Many women with chronic hypertension are prescribed these drugs for years without realizing they’re unsafe in pregnancy. That’s why guidelines from the American Heart Association and the American College of Cardiology now require doctors to:- Ask every woman of childbearing age: “Are you planning to become pregnant?”
- Confirm pregnancy status before starting these medications
- Switch to a safer alternative before conception
- Provide clear contraception advice if pregnancy isn’t planned
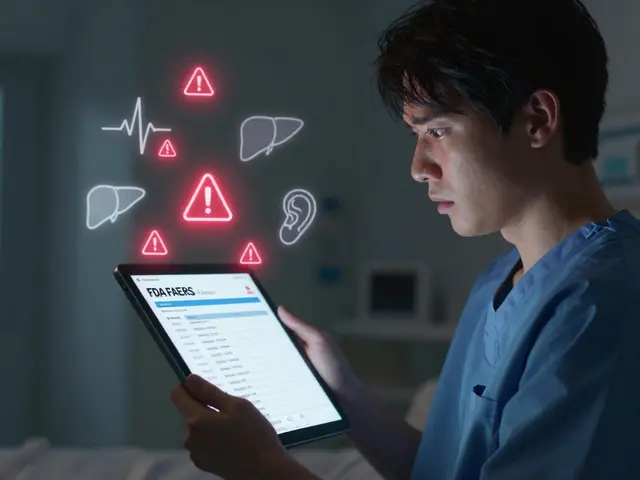
Why Do These Medications Still Get Prescribed During Pregnancy?
You’d think with such clear warnings, this wouldn’t happen. But according to FDA data from 2021, about 1.2% of pregnant women with chronic hypertension are still exposed to ACE inhibitors or ARBs. Why? Some doctors assume the patient isn’t planning pregnancy and don’t ask. Others think “it’s only been a few weeks”-but as we now know, even early exposure carries risk. Some patients don’t realize their blood pressure pill is dangerous because the label doesn’t scream “DANGER” in plain language. And in some places, access to alternatives is limited. The solution? Better communication. If you’re on one of these drugs, ask: “Is this safe if I get pregnant?” If you’re trying to conceive, say: “I’m planning to get pregnant-what should I switch to?”
What You Need to Do Right Now
If you’re taking an ACE inhibitor or ARB and:- Are pregnant: Call your OB-GYN or primary care provider immediately. Do not stop the medication on your own. They’ll guide you through a safe transition.
- Are trying to conceive: Schedule an appointment with your doctor to switch medications before stopping contraception.
- Are not planning pregnancy: Use reliable contraception and confirm with your doctor that your current method is effective. Don’t assume birth control is foolproof.
What About Breastfeeding?
After delivery, the risks change. ACE inhibitors and ARBs are generally considered safe during breastfeeding, though some doctors still prefer to avoid them. Labetalol and methyldopa are preferred if you’re nursing, as they pass into breast milk in very small amounts. Always discuss your plans with your doctor before restarting any blood pressure medication postpartum.Can I take ACE inhibitors or ARBs in the first trimester if I didn’t know I was pregnant?
Even if you took an ACE inhibitor or ARB in the first trimester before knowing you were pregnant, you still need to stop immediately. While earlier studies suggested first-trimester exposure might not cause major birth defects, newer research shows it still increases the risk of miscarriage, low birth weight, and premature birth. Your doctor will monitor your pregnancy closely with ultrasounds to check amniotic fluid levels and fetal growth, but the medication must be switched right away.
Are there any natural alternatives to manage blood pressure during pregnancy?
Lifestyle changes like reducing salt, eating more potassium-rich foods (bananas, spinach, sweet potatoes), staying active, and managing stress can help support blood pressure control. But they are not substitutes for medication if you have chronic hypertension. Natural methods alone won’t prevent complications like preeclampsia or fetal growth restriction in high-risk cases. Always use prescribed, pregnancy-safe drugs as directed-never replace them with supplements or diet alone.
What if my doctor says it’s okay to stay on my current medication?
If your doctor suggests continuing an ACE inhibitor or ARB during pregnancy, seek a second opinion. Every major medical organization-including ACOG, the American Heart Association, the World Health Organization, and the European Medicines Agency-agrees these drugs are unsafe. No reputable guideline makes an exception. Your health and your baby’s safety depend on following evidence-based standards, not individual opinion.
How long does it take for ACE inhibitors or ARBs to leave my system?
Most ACE inhibitors and ARBs clear from your bloodstream within 24 to 48 hours. But their effects on fetal development can linger, especially if exposure was prolonged. That’s why switching to a safer medication as soon as pregnancy is confirmed is critical-waiting even a few days can increase risk. Your doctor will monitor your blood pressure closely during the transition to ensure it stays stable.
Can I use ARBs or ACE inhibitors after giving birth?
Yes, after delivery, these medications are generally considered safe again. Many women resume them once breastfeeding is established or if they’re not nursing. However, your blood pressure may still be elevated postpartum, especially if you had preeclampsia. Your doctor will adjust your treatment plan based on your recovery, kidney function, and whether you’re breastfeeding. Always check with your provider before restarting.





Nicola George December 26, 2025
Okay, but let’s be real-how many women are even told this before they’re prescribed these meds? I’ve seen friends on lisinopril for years, told it’s ‘just for blood pressure,’ no mention of pregnancy risks until they got a positive test. That’s not medical care-that’s negligence wrapped in a white coat.
Janice Holmes December 28, 2025
THIS IS A MEDICAL EMERGENCY IN DISGUISE. 🚨 ACE INHIBITORS AND ARBS ARE FETAL POISONS. THEY DON’T JUST ‘RISK’ DAMAGE-THEY ACTIVATE A BIOLOGICAL CATASTROPHE. Oligohydramnios? Fetal renal agenesis? Skull deformities? This isn’t ‘maybe harmful’-this is ‘your baby’s kidneys are dissolving while you sleep.’ And yet, doctors still prescribe them like coffee. I’ve lost count of the OB-GYNs who shrug and say ‘it’s probably fine.’ IT’S NOT FINE. IT’S MURDER BY MISTAKE.
James Bowers December 29, 2025
While the clinical data is unequivocal, the practical implementation remains inconsistent across healthcare systems. The discontinuation protocol, though standardized in guidelines, is frequently delayed due to inadequate patient education, fragmented care pathways, and insufficient provider training in reproductive pharmacology. The 2021 FDA data indicating 1.2% exposure rates underscores systemic failure, not individual negligence. A multidisciplinary approach-integrating pharmacy alerts, preconception counseling mandates, and electronic health record flags-is not merely advisable; it is ethically obligatory.
Andrew Gurung December 29, 2025
Ugh. I can’t believe people still don’t get this. 😒 I had my OB literally tell me ‘it’s fine if you’re only 5 weeks’-like, are you kidding me? I switched to labetalol the same day. My baby’s fine now, but I’m still mad. If you’re on these meds and didn’t know? You’re not ‘lucky’-you’re just lucky you didn’t lose your kid. #PreconceptionCheck
Olivia Goolsby December 30, 2025
EVERYTHING YOU’RE TOLD IS A LIE. EVERY SINGLE WORD. ACE inhibitors? ARBs? They’re not just dangerous-they’re part of a pharmaceutical cover-up. The FDA’s ‘boxed warning’? That’s a joke. It’s printed in 6-point font on the back of the bottle. Meanwhile, the drug reps are in the doctors’ offices handing out free samples with no warning. And the ‘safe alternatives’? Methyldopa? That’s a 1970s relic. The real reason they don’t push newer drugs? Because they’re not profitable. The system doesn’t want you to know that your baby’s kidneys are being destroyed by a pill that’s been sold as ‘safe’ for decades. And don’t even get me started on how they ‘monitor’ with ultrasounds… like that fixes the damage. It’s just damage control for the corporation. Wake up.
Nikki Thames December 31, 2025
There is a profound ethical obligation here, one that transcends clinical guidelines: the duty to inform. Women are not merely patients; they are future mothers whose autonomy is violated when they are not explicitly, repeatedly, and documentedly warned of teratogenic risks. The failure to implement pre-prescription pregnancy screening-especially in populations with high rates of unplanned pregnancy-is not an oversight; it is a moral failure. The fact that this remains inconsistent across institutions reveals a systemic devaluation of reproductive agency. We must treat this not as a pharmacological issue, but as a human rights issue.
Chris Garcia January 1, 2026
In my village back in Nigeria, we say: ‘The hand that feeds you can also poison you.’ This is exactly that. A pill meant to save your life-now a silent thief of your child’s future. But here’s the beautiful thing: we have solutions. Labetalol, methyldopa-these aren’t magic. They’re medicine that remembers the mother AND the baby. The problem isn’t the science. It’s the silence. The silence of doctors who assume ‘she knows.’ The silence of pharmacies that don’t scream the warning. The silence of women who think ‘it’s just a pill.’ Let’s break that silence. Talk. Ask. Demand. Your child’s kidneys are listening.
Will Neitzer January 2, 2026
It is imperative to underscore that the transition from ACE inhibitors/ARBs to pregnancy-safe antihypertensives must be medically supervised, as abrupt cessation can precipitate hypertensive emergencies. The clinical protocols outlined by ACOG and the American Heart Association are evidence-based, pragmatic, and designed to preserve maternal-fetal homeostasis. Furthermore, the integration of pharmacogenomic screening in high-risk populations may soon enable more personalized transitions. For now, adherence to established guidelines remains the gold standard-no exceptions, no improvisations, no compromises.
Elizabeth Ganak January 3, 2026
my cousin took losartan for 3 months before she knew she was pregnant. she’s fine now but she cried for a week. just… talk to your doctor before you even try. don’t wait.