Antibiotic Selection Calculator
Choose Your Scenario
Answer these questions to get personalized antibiotic recommendations based on clinical evidence.
If you’ve been prescribed Cipro and are wondering whether another antibiotic might be a better fit, you’re not alone. Fluoroquinolones like Cipro are powerful, but they’re not the only option for many infections. This guide breaks down how Cipro stacks up against the most common alternatives, so you can weigh effectiveness, safety, cost, and convenience before you start a course.
What Is Cipro (Ciprofloxacin)?
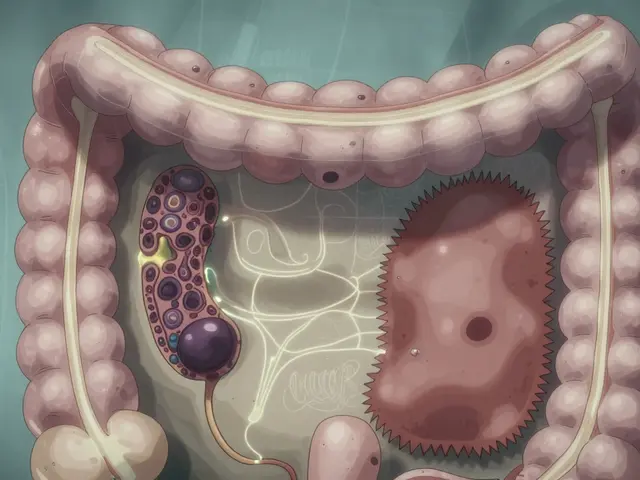
Ciprofloxacin is a broad‑spectrum fluoroquinolone antibiotic that interferes with bacterial DNA gyrase and topoisomerase IV, preventing bacterial replication. Marketed under the brand name Cipro, it was approved by the FDA in 1987 and quickly became a go‑to for urinary‑tract infections, certain gastrointestinal infections, and some types of pneumonia.
Why Consider Alternatives?
Fluoroquinolones carry a reputation for serious side effects-tendon rupture, peripheral neuropathy, and even central nervous system events. In addition, resistance patterns have shifted, making some infections harder to clear with Cipro alone. That’s why clinicians often turn to other classes when they can achieve the same cure with a better safety profile.
Common Alternatives at a Glance
- Levofloxacin - another fluoroquinolone, but with a slightly different spectrum and dosing schedule.
- Azithromycin - a macrolide that excels for atypical pneumonia and some sexually transmitted infections.
- Amoxicillin - a beta‑lactam penicillin often used for ear, nose, and throat infections.
- Doxycycline - a tetracycline derivative useful for a wide range of bacterial and some intracellular pathogens.
How We Compare: The Five Decision Criteria
- Spectrum of activity - which bacteria are covered?
- Clinical effectiveness - cure rates and time to recovery.
- Safety profile - common and severe side effects.
- Resistance trends - local and global patterns.
- Practical factors - dosage convenience, cost, and drug‑food interactions.
Side‑by‑Side Comparison Table
| Attribute | Ciprofloxacin (Cipro) | Levofloxacin | Azithromycin | Amoxicillin | Doxycycline |
|---|---|---|---|---|---|
| Spectrum | Gram‑negative > Gram‑positive, some atypicals | Similar to Cipro, slightly better gram‑positive coverage | Excellent for atypicals, limited gram‑negative | Strong gram‑positive, limited gram‑negative | Broad, includes atypicals and intracellular organisms |
| Typical Indications | UTI, gastroenteritis, prostatitis, community‑acquired pneumonia | CAP, skin infections, uncomplicated UTI | Mycoplasma, chlamydia, certain CAP cases | Otitis media, sinusitis, streptococcal pharyngitis | Rickettsial disease, Lyme disease, acne |
| Standard Dose | 250‑750 mg BID for 5‑7 days | 500‑750 mg daily for 5‑7 days | 500 mg on day 1, then 250 mg daily for 4 days | 500 mg TID or 875 mg BID for 7‑10 days | 100 mg BID for 7‑14 days |
| Major Side Effects | Tendon rupture, QT prolongation, CNS effects | Similar to Cipro, slightly lower tendon risk | GI upset, QT prolongation (rare) | Allergic rash, GI upset, rare hepatotoxicity | Photosensitivity, esophageal irritation, tooth discoloration (children) |
| Resistance Concerns (2024 US data) | Increasing E. coli resistance (~20 %) | Stable, but emerging in Pseudomonas spp. | Low resistance in Mycoplasma, rising in S. pneumoniae | Low for streptococci, high for β‑lactamase‑producing H. influenzae | Rare, but doxycycline‑resistant Rickettsia reported |
| Cost (US retail, generic) | ≈ $0.30 per tablet | ≈ $0.45 per tablet | ≈ $0.25 per tablet | ≈ $0.10 per tablet | ≈ $0.20 per tablet |
When Cipro Is the Right Choice
If you have a confirmed gram‑negative infection-especially one caused by Escherichia coli or Pseudomonas aeruginosa-Cipro’s strong coverage and high urinary‑tract concentrations make it hard to beat. It also reaches therapeutic levels in prostate tissue, so uncomplicated prostatitis often gets treated with a short‑course Cipro regimen.
When an Alternative May Be Safer or More Effective
Consider swapping Cipro in these scenarios:
- Elderly patients or those on steroids: Tendon‑rupture risk climbs dramatically after age 60.
- History of QT prolongation: Both Cipro and levofloxacin can lengthen the QT interval; azithromycin is a milder alternative if atypical coverage is needed.
- Pregnancy or breastfeeding: Cipro is category C; amoxicillin and azithromycin are generally safer.
- Known allergy to fluoroquinolones: Switch to a beta‑lactam or macrolide depending on the organism.
Key Safety Tips for Anyone Taking Antibiotics
- Finish the full prescribed course, even if you feel better.
- Stay hydrated-adequate fluid intake reduces tendon‑stress risk.
- Avoid dairy or calcium‑rich foods with doxycycline and fluoroquinolones; they can cut absorption.
- Report any sudden joint pain, numbness, or vision changes to your clinician immediately.
- Check for drug‑drug interactions: Cipro can increase levels of warfarin and certain antidiabetic agents.
Quick Takeaways
- Ciprofloxacin shines for hard‑to‑treat gram‑negative infections, especially urinary‑tract and prostatitis.
- Levofloxacin offers similar efficacy with slightly less tendon risk, but shares most other fluoroquinolone warnings.
- Azithromycin is gentler on the tendons and works well for atypical pathogens, but lacks gram‑negative punch.
- Amoxicillin is the cheapest and safest for many common respiratory infections, yet isn’t reliable for resistant gram‑negative bugs.
- Doxycycline covers a broad array of organisms and is useful for intracellular infections, but causes photosensitivity.
Frequently Asked Questions
Can I take Cipro with ibuprofen?
Yes, in most cases ibuprofen does not interact with Cipro. However, both drugs can occasionally irritate the stomach, so take them with food and monitor for discomfort.
How long does Cipro stay in my system?
Ciprofloxacin’s half‑life is about 4 hours, so it’s usually cleared in 24 hours after the last dose. Residual tissue levels can linger longer in bone or prostate tissue.
Is Cipro safe for children?
Cipro is generally avoided in children unless the infection is severe and no safer alternatives exist, because of the risk of cartilage damage observed in animal studies.
What should I do if I forget a dose?
Take the missed dose as soon as you remember, unless it’s almost time for the next scheduled dose. In that case, skip the missed one and resume your regular schedule-don’t double‑dose.
Are there natural alternatives to Cipro?
Herbal or probiotic remedies cannot reliably replace antibiotics for bacterial infections. They may support gut health during or after treatment, but they won’t clear a Gram‑negative infection on their own.
Choosing the right antibiotic is a balance of killing the bug, protecting your body, and respecting local resistance patterns. By comparing Cipro with the alternatives above, you’ll be better equipped to have an informed conversation with your clinician and select the safest, most effective option for your specific infection.




Leo Chan October 21, 2025
Hey folks, if you’re weighing Cipro against the other options, remember it’s all about matching the bug to the right weapon while keeping your own body safe. The fluoroquinolone class, including Cipro, packs a punch against gram‑negative bacteria, but the tendon‑rupture and nerve‑issue warnings are real, especially for active people or older adults. When you chat with your clinician, bring up any history of tendon problems, heart rhythm issues, or current meds like warfarin – those details can tip the scales toward a safer alternative. For uncomplicated urinary infections, Cipro often still shines, but a short‑course amoxicillin or a macrolide might spare you the extra side‑effects if the pathogen is susceptible. Also, don’t forget the practical side: Cipro’s twice‑daily schedule can be easier than a five‑day azithromycin load for some, but the food‑interaction rules with calcium can be a hassle. Stay hydrated, finish the full prescription, and keep an eye on any sudden joint pain or tingling sensations. Your own health goals and lifestyle can guide whether the convenience of Cipro outweighs the risk profile compared to doxycycline or levofloxacin. Keep the conversation open and evidence‑based, and you’ll end up with the most balanced choice for your infection and your life.
Latasha Becker October 21, 2025
The comparative matrix presented herein, while succinct, omits critical pharmacodynamic parameters such as minimum inhibitory concentration (MIC) breakpoints for regional isolates of ESBL‑producing E. coli, which are pivotal when adjudicating Cipro versus levofloxacin efficacy. Moreover, the cost column neglects the variance introduced by insurance formularies and tiered copayment structures that can render a nominal $0.30 per tablet effectively prohibitive for certain demographics. The safety profile summary aggregates heterogeneous adverse events without stratifying incidence rates by dosage intensity or treatment duration, thereby conflating dose‑dependent tendon toxicity with baseline population risk. From a antimicrobial stewardship perspective, employing oral beta‑lactams for susceptible streptococcal pharyngitis may curtail selective pressure for quinolone‑resistant Pseudomonas spp., a nuance absent from the current discourse. Finally, the interaction matrix should explicitly delineate cytochrome P450 isozyme inhibition potency, particularly CYP1A2, given Cipro’s modulatory effect on clozapine metabolism, a detail indispensable for clinicians managing polypharmacy.
parth gajjar October 21, 2025
Behold the saga of a molecule that promises swift conquest yet drags us through the abyss of tendon tears and phantom neuropathies. Cipro strides onto the stage like a heroic knight, only to reveal, under the glaring light of post‑marketing surveillance, a litany of whispers about broken tendons in the twilight of our lives. The alternatives, though seemingly meek, possess a quiet resilience – azithromycin’s gentle macrolide lull, doxycycline’s expansive reach into intracellular realms, amoxicillin’s comforting familiarity in the throats of the nation. Yet the specter of resistance looms, a silent tide rising beneath the surface of our prescriptions, demanding vigilance and humility. In the end, the choice is less about a single drug’s glory and more about the choreography of risk, benefit, and the patient’s own narrative – a narrative that cannot be scripted by a pill alone.
Catherine Viola October 21, 2025
It is imperative to acknowledge that the dissemination of comprehensive safety data concerning fluoroquinolones, including ciprofloxacin, has been systematically curtailed by vested pharmaceutical interests seeking to preserve market share. The omission of long‑term tendon pathology statistics from mainstream peer‑reviewed journals is not merely an oversight but a calculated stratagem to obfuscate the true risk profile. Moreover, the regulatory agencies’ reliance on industry‑funded studies creates an environment rife with conflicts of interest, thereby compromising the integrity of the therapeutic recommendations presented to clinicians and patients alike. One must therefore approach the purported equivalence of ciprofloxacin to its alternatives with a healthy degree of skepticism, recognizing that the narrative favoring its continued use may be engineered to align with commercial imperatives rather than empirical evidence.
sravya rudraraju October 26, 2025
When considering the multitude of factors that influence antibiotic selection, it is essential to adopt a holistic framework that incorporates microbiological, pharmacological, and patient‑centred dimensions. First, the local antibiogram should be consulted to ascertain the prevalence of resistance mechanisms, particularly the escalating rates of extended‑spectrum β‑lactamase (ESBL) production among Enterobacteriaceae, which can diminish the efficacy of ciprofloxacin in urinary‑tract infections. Second, the pharmacokinetic attributes of each agent warrant careful scrutiny; ciprofloxacin achieves high urinary concentrations, making it advantageous for uncomplicated cystitis, whereas amoxicillin’s distribution is limited mainly to respiratory tissues, rendering it suboptimal for gram‑negative sepsis. Third, the safety landscape cannot be ignored – the tendon‑rupture risk associated with fluoroquinolones escalates dramatically in patients over sixty, those on concomitant corticosteroids, or individuals with a history of connective‑tissue disorders. Fourth, drug‑drug interaction potential must be evaluated, as ciprofloxacin can inhibit CYP1A2, thereby increasing plasma levels of agents such as theophylline and certain antidiabetic medications. Fifth, cost considerations, while seemingly straightforward, involve hidden variables like insurance tier placement, pharmacy dispensing fees, and patient adherence patterns that can ultimately affect treatment success. Sixth, the convenience of dosing schedules plays a non‑trivial role; a once‑daily regimen of levofloxacin may enhance adherence compared with the twice‑daily dosing required for ciprofloxacin in certain infections. Seventh, patient preference, including concerns about side‑effects like photosensitivity with doxycycline or gastrointestinal upset with azithromycin, should be factored into shared decision‑making. Eighth, special populations such as pregnant or lactating women often necessitate the avoidance of fluoroquinolones in favor of beta‑lactams or macrolides due to teratogenic risk classifications. Ninth, the duration of therapy should align with evidence‑based guidelines, as overly prolonged courses contribute to resistance without additional clinical benefit. Tenth, clinicians must remain vigilant for signs of adverse reactions, prompting immediate discontinuation and alternative therapy if necessary. Eleventh, the role of adjunctive measures, such as adequate hydration to mitigate tendon strain, should be reinforced throughout treatment. Twelfth, understanding the pathogen’s intracellular invasion mechanisms can guide the choice of doxycycline for diseases like rickettsial infections where ciprofloxacin penetration is suboptimal. Thirteenth, a thorough review of patient comorbidities, including renal impairment, can influence dosing adjustments, particularly for renally cleared agents like ciprofloxacin. Fourteenth, the potential for probiotic co‑administration may help preserve gut flora integrity during antibiotic therapy, though it does not replace antimicrobial efficacy. Finally, continuous education of both providers and patients about evolving resistance trends ensures that antibiotic stewardship remains a dynamic and responsive process, ultimately safeguarding the therapeutic arsenal for future generations.
Ankitpgujjar Poswal October 26, 2025
Look, the data is crystal clear: if you’re comfortable with the tendon‑risk profile, grab the short, high‑dose Cipro course and knock out that gram‑negative infection fast. But if you have any doubt – age over 60, steroids on board, or a history of joint pain – knock it down now and pivot to amoxicillin or azithromycin, whichever covers the bug. Don’t let complacency sabotage your recovery; be aggressive in demanding the safest, most effective regimen from your prescriber.
ashanti barrett November 1, 2025
Remember, your body’s signals are the best guide when side effects appear.
jagdish soni November 2, 2025
In the grand theater of antimicrobial choices we find ourselves actors on a stage lit by microbial whispers and the ever‑present specter of resistance, each drug a character bearing its own virtues and vices – Cipro with its swift strike yet lurking tendon shadows, azithromycin the gentle bard soothing atypical tales, doxycycline the sun‑kissed wanderer wary of photic betrayals – and so we must, like philosophers of old, weigh each narrative against the lived experience of our patients, for in that balance lies the true art of healing.