Every time you pick up a prescription, there’s a good chance the pharmacist hands you a generic version instead of the brand-name drug your doctor wrote on the script. That’s legal - and common. But it’s not always automatic. You have the right to say no. And if you’re on a medication where even small changes can cause problems, you should know how to protect yourself.
Why Generic Substitution Happens
Generic drugs are cheaper copies of brand-name medications. They contain the same active ingredients and are required by the FDA to work the same way. That’s why pharmacies and insurers push them: they save money. In 2023, generics made up 92% of all prescriptions filled in the U.S. but only 24% of total drug spending. A single generic pill can cost 80-85% less than its brand-name counterpart. That’s why your insurance plan or pharmacy benefit manager (PBM) prefers them. But cost savings don’t always mean better outcomes. For some people, switching from a brand-name drug to a generic - or even between two generics - can cause side effects, reduced effectiveness, or dangerous fluctuations in how the drug works in the body. This is especially true for drugs with a narrow therapeutic index (NTI), where the difference between a safe dose and a harmful one is very small.When You Should Refuse a Generic
Not all drugs are safe to swap. The FDA lists certain medications as high-risk for substitution. These include:- Antiepileptic drugs (like phenytoin, carbamazepine)
- Thyroid medications (like levothyroxine)
- Blood thinners (like warfarin)
- Some psychiatric drugs (like lithium)
- Biosimilar insulins (like Basaglar instead of Lantus)
Your Legal Right to Say No
You don’t need to be a lawyer to refuse a generic. All you have to say is: "I decline substitution." That’s it. In 43 states, those three words are legally enough to stop the pharmacist from switching your medication. But state laws vary widely. Here’s what you need to know:- 19 states (including California, Texas, and New York) let pharmacists substitute generics automatically - but they must still notify you.
- 31 states plus D.C. require pharmacists to tell you before substituting - either verbally or in writing.
- 7 states plus D.C. (Alaska, Connecticut, Hawaii, Maine, Massachusetts, New Hampshire, Vermont) require your explicit consent before any substitution. In these places, the pharmacist cannot switch your drug unless you say yes.
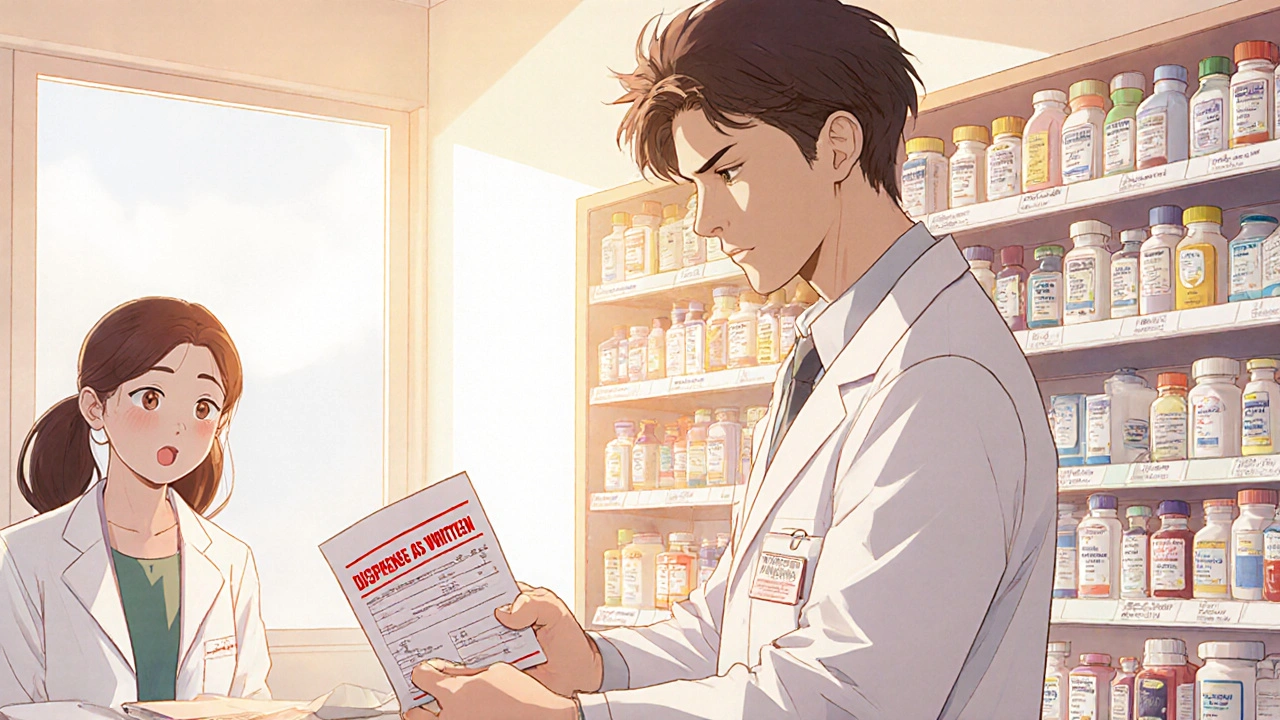
How to Get a Brand-Name Prescription Approved
If you need a brand-name drug for medical reasons, the best way to block substitution is to get your doctor to write "Dispense as Written" or "Brand Medically Necessary" on the prescription. Forty-eight states recognize this notation as a legal override. Your doctor doesn’t need to write a long explanation. Just ask them to check the box or write it clearly. Some doctors are hesitant - they don’t want to fight insurers or think generics are always fine. But if you’ve had issues before, or if you’re on a high-risk drug, insist. You’re not being difficult. You’re being smart. If your doctor refuses, ask them to document your medical history: "Patient experienced adverse effects after generic substitution in [year]. Stable on brand-name [drug]. Substitution not recommended." That’s enough for most pharmacies.What to Do If the Pharmacist Pushes Back
Sometimes pharmacists say things like:- "I have to substitute - it’s the law."
- "You’ll pay more if you don’t take the generic."
- "The insurance won’t cover it otherwise."
- Ask to speak to the pharmacy manager.
- State clearly: "I am exercising my right to refuse substitution under [your state] law."
- If they still refuse, ask for a copy of the state’s generic substitution law - most pharmacies have it posted or can print it.
- If the issue continues, file a complaint with your state’s Board of Pharmacy. Every state has a process for this.
How to Protect Yourself Going Forward
Here’s what to do after every prescription:- Always ask: "Is this the brand-name drug my doctor prescribed?"
- Check the pill’s shape, color, and imprint. Generics often look different - even if they’re the same drug.
- Keep a list of every medication you take, including the brand or generic name, and when you started it.
- Use the FDA’s Orange Book (available online) to check if your drug is rated as therapeutically equivalent (AB rating). Drugs with an AB rating are considered interchangeable. Drugs with an AB1, AB2, or B rating may not be.
- Track your symptoms. If you notice new side effects, mood changes, or worsening conditions after a refill, ask: "Was this drug switched?"
What’s Changing in 2025
The FDA is moving toward stricter rules for complex generics - especially drugs like inhalers, injectables, and biosimilars. In 2023, Colorado and Nevada passed new laws requiring pharmacists to notify prescribers when they substitute a biosimilar. That’s now the norm in 47 states. Meanwhile, the Congressional Budget Office estimates that non-medical switching - changing patients from a stable brand to a generic without clinical reason - costs the system $2.1 billion a year due to increased hospital visits, lab tests, and doctor visits. The trend is clear: while generics save money, unchecked substitution creates hidden costs - and risks. More states are recognizing that patient safety should come before cost-cutting.Resources to Help You
- Your state’s Board of Pharmacy - Find contact info at www.nabp.pharmacy
- FDA’s Orange Book - Search for therapeutic equivalence ratings at www.fda.gov/drugs/drug-approvals-and-databases
- GoodRx - Compare cash prices for brand vs. generic drugs
- Consumer Reports - Reports on patient experiences with substitution
- National Organization for Rare Disorders - Support for patients on specialty medications
Can I refuse a generic drug even if my insurance says I have to take it?
Yes. Insurance plans can’t force you to take a generic. You have the legal right to refuse substitution in most states. If your insurance denies coverage for the brand-name drug after you refuse, ask your pharmacist to check the cash price - it might be cheaper than your co-pay thanks to the 2018 Know the Lowest Price Act. You can also ask your doctor to write "Dispense as Written" or file an appeal with your insurer using your medical history as evidence.
Are generic drugs always safe to substitute?
No. For drugs with a narrow therapeutic index - like levothyroxine, warfarin, or seizure medications - even tiny differences in absorption can cause serious side effects. The FDA considers these drugs "not interchangeable" in practice, even if they’re rated as therapeutically equivalent. Many doctors and patients report problems after switching. Always ask if your drug is high-risk before accepting a generic.
What if my pharmacist says they "have to" substitute?
That’s not always true. In 19 states, pharmacists can substitute automatically, but they still must notify you. In 7 states plus D.C., they need your consent - so if they say "I have to," they’re lying. Ask to speak to the manager and cite your state’s law. You can find your state’s rules at your Board of Pharmacy’s website. If they still refuse, file a complaint.
Can I get my brand-name drug for free or at a lower cost?
Yes. Many drug manufacturers - like Pfizer, Merck, and Novo Nordisk - offer patient assistance programs for brand-name medications. You can also use GoodRx coupons, which often make the brand-name drug cheaper than your insurance co-pay. Some pharmacies will even match cash prices. Always ask: "What’s the lowest price I can pay?"
How do I know if my state requires consent for substitution?
Your state requires explicit consent if you live in Alaska, Connecticut, Hawaii, Maine, Massachusetts, New Hampshire, Vermont, or Washington, D.C. In all other states, pharmacists must notify you before substituting. You can verify your state’s law by visiting your state’s Board of Pharmacy website or calling them directly. If you’re unsure, always say "I decline substitution" - it’s your right everywhere.




Matthew Mahar November 22, 2025
i just got switched to a generic levothyroxine last month and my heart started doing the cha-cha at 3am. i thought i was dying. turns out my TSH went from 2.1 to 8.9. my doc didn’t even know it happened. i had to scream "I decline substitution" at the pharmacy like a lunatic. now they know my face. and my insurance? still tries to sneak it in. ugh.
John Mackaill November 23, 2025
Just wanted to add that in the UK, we don’t have this problem because the NHS mandates generics unless specified. But I’ve seen friends from the US struggle with this - it’s wild how profit-driven the system is. You’re right to fight for stability. Your body isn’t a cost center. Period.
Adrian Rios November 23, 2025
Look, I get it - generics save money. But let’s be real: if you’re on warfarin and your INR goes from 2.4 to 4.8 because the pill looks different and the fillers changed, you’re not saving money - you’re in the ER. I’ve been on the same brand of carbamazepine for 17 years. I’ve had seizures since I was 12. I don’t care if it costs $300 a month. I’m not a lab rat for PBMs. And if your pharmacist says "it’s the law," ask them to show you the statute. They can’t. Because it’s not. Not in my state. Not in most. You have rights. Use them. Write "Dispense as Written" on your script. If your doctor won’t, find a new one. Your life is worth more than a $0.50 savings.
Casper van Hoof November 24, 2025
One cannot help but observe the systemic tension between pharmaceutical economics and individual physiological integrity. The FDA’s therapeutic equivalence paradigm, while statistically robust, fails to account for bioindividuality - a concept increasingly validated by pharmacogenomic research. The substitution protocol, as currently implemented, represents a utilitarian compromise that, while efficient, risks commodifying human health. The patient’s agency, therefore, is not merely a legal formality - it is an ontological imperative.
Richard Wöhrl November 25, 2025
Important note: If you're on lithium, levothyroxine, or phenytoin - DO NOT let them switch you without testing. I’m a pharmacist. I’ve seen too many cases where patients come in with weird symptoms, and it’s because the generic they got had a different dissolution rate. Even AB-rated generics aren’t identical - the fillers change how fast the drug hits your bloodstream. Always check the pill imprint. Keep a log. And if your insurance denies the brand? Ask for a cash price on GoodRx - sometimes it’s cheaper. I’ve had patients pay $10 cash for Synthroid instead of $45 with insurance. Also: if a pharmacist says "I have to," they’re lying. Call your state board. They’ll help you.
Pramod Kumar November 26, 2025
Bro, this is why I love India - we don’t have this mess. If you want brand, you pay for brand. No one forces you. But here in the US, it’s like the system is trying to turn your medicine into a lottery ticket. I had a cousin who got switched to a generic insulin and ended up in the ICU. Now she carries a laminated card that says "NO GENERIC SUBSTITUTION" and shows it to every pharmacist. Smart. You gotta be your own advocate. Don’t wait for the system to wake up.
Brandy Walley November 27, 2025
Ugh. I hate how everyone acts like they’re a martyr because they got a generic. Just take the pill. Your thyroid is fine. You’re just being dramatic. I’ve been on generics for 20 years. I’m still alive. Stop being so entitled. Also, why do you think doctors write "dispense as written"? Because they’re lazy and want you to pay more. Grow up.
shreyas yashas November 27, 2025
Man, I used to think generics were just cheaper versions. Then my uncle got switched to a different generic of levothyroxine and his hands started shaking. He didn’t even know why. We found out later the new one had a different coating. Now he only takes the one with the little "S" on it. I print out the FDA orange book stuff and show it to my pharmacist. They roll their eyes, but they give me the right one. Small wins.
Suresh Ramaiyan November 27, 2025
It’s funny how we’ve normalized surrendering control over our own bodies to algorithms and cost-cutting. We don’t question the car mechanic who says "this part is interchangeable," but when it comes to medicine - the thing keeping us alive - we’re expected to trust a pill that looks different and costs less. Maybe the real issue isn’t the generic. It’s that we’ve stopped asking: "Who benefits from this?" And who pays the price?
Katy Bell November 28, 2025
I just had a pharmacist try to give me a generic for my seizure med. I said "I decline substitution." He stared at me like I asked for a unicorn. Then he handed me the brand. No argument. Just nodded. I think he’s seen this before. Don’t be shy. Say it loud. You’re not being difficult. You’re being smart.
Ragini Sharma November 29, 2025
generic? more like generic-ly bad. i got switched to some weird generic warfarin and my gums started bleeding like i was in a horror movie. turns out the fillers were different. my doc was like "oh yeah that happens." like that’s normal?? nope. i now have a note taped to my fridge: "NO GENERIC FOR ME. EVER."
Linda Rosie December 1, 2025
Patients possess a legally recognized right to refuse generic substitution in the majority of U.S. jurisdictions. This right is grounded in both statutory law and ethical principles of informed consent. The implementation of this right, however, remains inconsistent due to systemic under-education of pharmacy personnel and patient apathy. Vigilance is required.
Vivian C Martinez December 1, 2025
Hey - if you’ve ever had to fight for your brand-name med, you’re not alone. I’ve been there. I’ve cried in pharmacy parking lots. But you’re doing the right thing. Keep documenting. Keep asking. Keep saying "I decline substitution." It’s not just about you - it’s about making the system better for the next person. You’re not being difficult. You’re being brave. And you’re helping others. Thank you.
Ross Ruprecht December 1, 2025
Wow. So much drama over a pill. Can we just all take the cheaper one and stop being so sensitive? I mean, it’s the same chemical. Chill.
Adrian Rios December 2, 2025
Yeah, Ross - you’re probably the kind of guy who thinks "it’s just a pill" until your kidneys fail because your generic blood thinner didn’t dissolve right. You’re not helping. You’re part of the problem. Go read the FDA’s data on non-medical switching and hospitalizations. Or better yet - try switching your insulin and then come back and tell me it’s "just a pill." I’ve been stable on brand-name carbamazepine for 17 years. I’ve had seizures since I was 12. I don’t care if it costs $300 a month. I’m not a lab rat for PBMs. And if your pharmacist says "it’s the law," ask them to show you the statute. They can’t. Because it’s not. Not in my state. Not in most. You have rights. Use them. Write "Dispense as Written" on your script. If your doctor won’t, find a new one. Your life is worth more than a $0.50 savings.