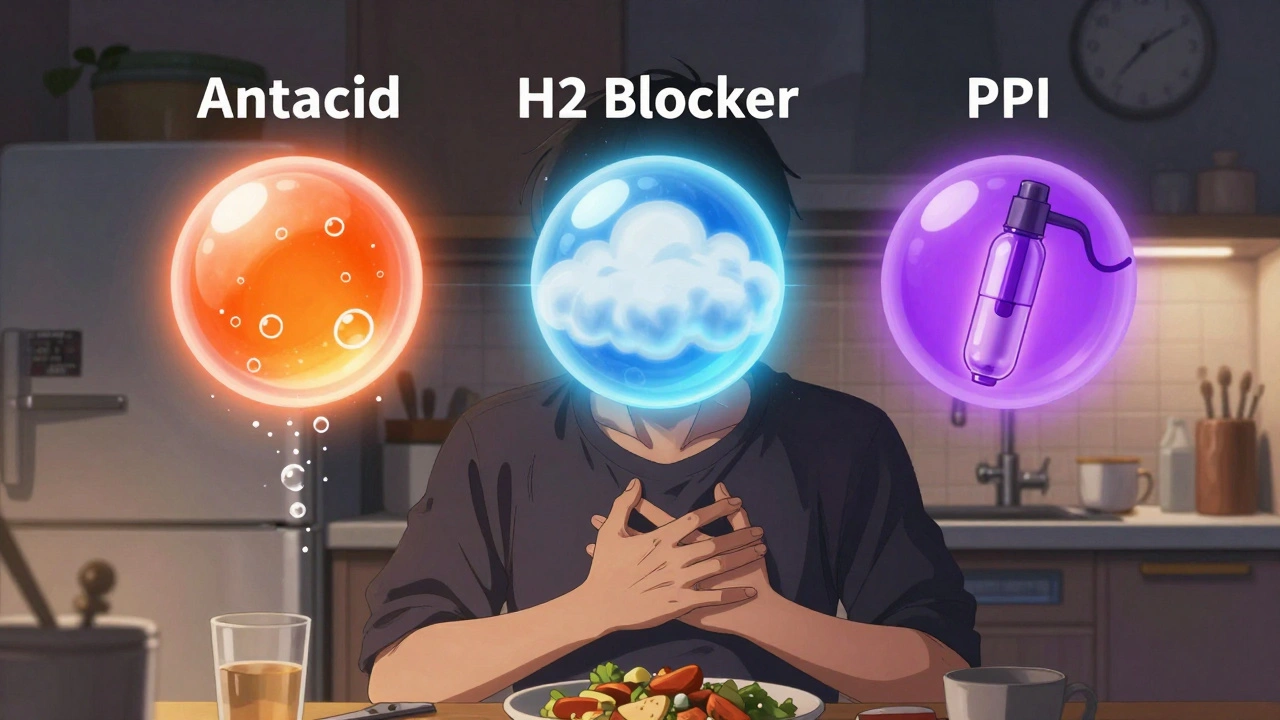
Heartburn hits hard - that burning feeling in your chest after eating, lying down, or even just bending over. It’s not just discomfort; it can wreck your sleep, your meals, and your day. And if you’re like millions of Americans, you’ve reached for an OTC pill without thinking twice. But not all heartburn meds are the same. OTC heartburn medications fall into three distinct categories: antacids, H2 blockers, and proton pump inhibitors (PPIs). Each works differently, lasts differently, and comes with different risks. Knowing which one to use - and when - can save you from side effects, wasted money, and worse, long-term health problems.
Antacids: Fast But Short-Lived Relief
Antacids are the OG of heartburn relief. They’ve been around since the 1800s, and you’ve probably seen them on the shelf: Tums, Rolaids, Maalox. These chewable tablets or liquids work by directly neutralizing stomach acid. Think of them like pouring baking soda into a fizzy drink - they cancel out the acid right where it’s causing trouble.
Here’s the catch: they work fast, but they don’t last. If you take a Tums tablet, you’ll feel relief in under a minute. That’s why so many people reach for them during a sudden flare-up. But the effect fades in about 30 to 60 minutes. That’s why you might find yourself popping five tablets after dinner, then another two after dessert. It’s not just annoying - it’s expensive, and too much calcium carbonate (the main ingredient in Tums) can cause rebound acid production. Studies show up to 30% of users end up with worse heartburn a few hours later because the body overcompensates.
Antacids are best for occasional heartburn - say, once a week or less. If you’re having it more often, antacids won’t cut it. They also interfere with other meds. If you take antibiotics, iron, or thyroid pills, you need to wait at least two hours after an antacid before taking them. Otherwise, your body won’t absorb them properly. And if you’re on a low-sodium diet, watch out: some antacids are loaded with sodium bicarbonate.
H2 Blockers: The Middle Ground
H2 blockers - like Pepcid AC, Tagamet HB, and Axid AR - don’t neutralize acid. They tell your stomach to make less of it. They block histamine, a chemical that signals your stomach cells to pump out acid. This is a smarter approach than just mopping up acid after it’s spilled.
They take longer to kick in - about an hour - but they last longer. One dose can keep acid down for 8 to 12 hours. That’s why they’re perfect for people who know heartburn is coming: before a big meal, after wine and cheese, or if you’re prone to nighttime symptoms. A 2023 study in Alimentary Pharmacology & Therapeutics found that famotidine (Pepcid) reduces nighttime acid by 75%, making it one of the few OTC options that actually helps you sleep.
But H2 blockers have a flaw: they lose effectiveness over time. After 2 to 3 weeks of daily use, your body starts to adapt. The acid suppression drops from 60-70% down to maybe 30%. That’s why you might notice Pepcid working great at first, then suddenly feeling like it’s not doing anything anymore. This is called tachyphylaxis. It’s not addiction - it’s biology.
They’re also not great for immediate relief. If you’re already burning, an H2 blocker won’t help right away. You need to take it 30 to 60 minutes before eating to get the most benefit. And they can interact with other drugs - especially warfarin and phenytoin. If you’re on blood thinners or seizure meds, check with a pharmacist before using them regularly.
PPIs: The Heavy Hitters - With Heavy Risks
Proton pump inhibitors (PPIs) are the strongest OTC heartburn meds you can buy without a prescription. Brands like Prilosec OTC, Nexium 24HR, and Prevacid 24HR shut down the acid pumps in your stomach cells entirely. They don’t just reduce acid - they suppress it by 90 to 98%. That’s why they’re so effective for frequent heartburn - two or more days a week.
But they’re slow. You won’t feel better the first day. It takes 2 to 3 days of consistent use for them to reach full power. And you have to take them right - 30 to 60 minutes before breakfast. If you take them after eating, or with orange juice (which breaks down the enteric coating), they won’t work. Many users think they’re broken because they don’t feel instant relief. They’re not broken - you’re just using them wrong.
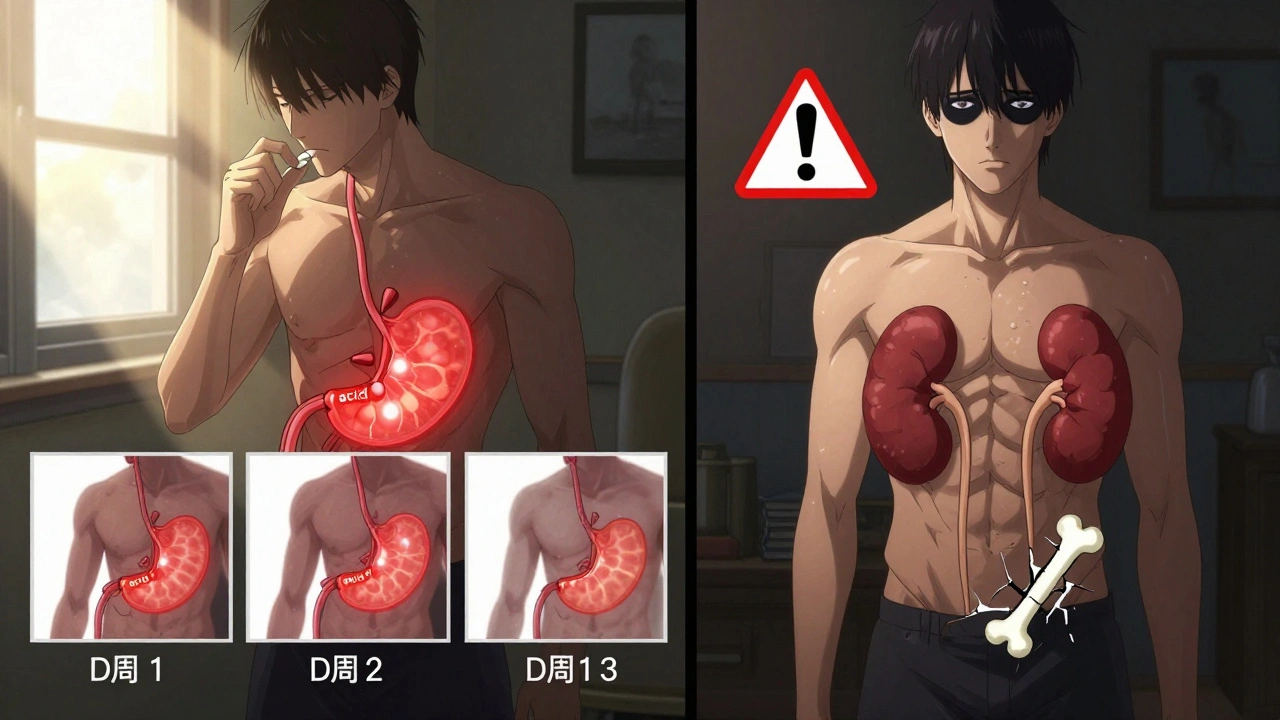
Here’s the real problem: long-term use. The FDA has issued multiple safety warnings about PPIs. Using them for more than 14 days straight without seeing a doctor increases your risk of:
- Low magnesium (can cause muscle cramps, irregular heartbeat)
- Vitamin B12 deficiency (leads to fatigue, nerve damage)
- Increased risk of C. diff infection (a dangerous gut bacteria)
- Higher chance of hip fractures (especially in older adults)
- Acute kidney injury and chronic kidney disease (newer research shows a 23% higher risk after a year of daily use)
And it’s not rare. A 2023 Johns Hopkins study found that 1 in 5 long-term PPI users developed signs of kidney damage. The FDA has issued 17 warning letters to manufacturers since 2022 for inadequate labeling about these risks. Yet, 43% of people keep taking PPIs beyond the 14-day limit, according to Columbia University research. That’s not just misuse - it’s dangerous.
PPIs aren’t meant for occasional heartburn. They’re for people who’ve tried everything else and still have symptoms. If you’re using one for more than two weeks, you need to see a doctor. It might not be heartburn at all - it could be ulcers, GERD, or even something more serious.
Which One Should You Use?
There’s no one-size-fits-all. Your choice depends on how often you get heartburn.
Less than once a week? Go with an antacid. Tums, Rolaids, or a generic calcium carbonate tablet. Chew it, wait for relief, and don’t overdo it.
Once or twice a week - and you know when it’s coming? Use an H2 blocker. Take Pepcid AC 30 minutes before your risky meal. It’s cheaper than PPIs, safer for short-term use, and works great for predictable triggers.
Two or more days a week? You need a PPI - but only for 14 days. Use Prilosec or Nexium 24HR exactly as directed: one pill, 30 minutes before breakfast. If it helps, great. But if you still feel burning after 14 days, stop. Talk to a doctor. Don’t just keep buying another bottle.
And if you’re mixing them? That’s common. Nearly 70% of frequent heartburn sufferers use antacids on top of PPIs for breakthrough pain. That’s fine - as long as you’re not using the antacid as a crutch for long-term PPI use.
What No One Tells You
Most people don’t realize that heartburn isn’t always about acid. Stress, obesity, smoking, alcohol, and certain foods (coffee, chocolate, spicy meals) can trigger it. Medications only treat the symptom - not the cause. If you’re popping pills every day, ask yourself: What’s really going on?
Also, generic PPIs are just as good as brand names. Curist’s generic versions cost $4.99 instead of $25. Same active ingredient. Same FDA approval. You’re not getting more power by paying more.
And don’t ignore lifestyle. Losing 10 pounds can cut heartburn by half. Eating smaller meals. Not lying down for 3 hours after eating. Elevating your head while sleeping. These changes work better than any pill - and they don’t come with a warning label.
When to See a Doctor
OTC meds are great for occasional heartburn. But if you need them more than twice a week for more than two weeks, it’s time to talk to a professional. Other red flags:
- Difficulty swallowing
- Unexplained weight loss
- Vomiting blood or black, tarry stools
- Chest pain that spreads to your arm or jaw
That last one? Could be a heart attack. Don’t assume it’s heartburn. When in doubt, get checked.
Heartburn is common. But treating it like a minor annoyance - with endless bottles of pills - is a mistake. The right OTC med can help. But the right plan - including lifestyle changes and knowing when to stop - is what keeps you healthy long-term.
Can I take antacids every day?
You shouldn’t. Antacids are meant for occasional use - once or twice a week. Taking them daily, especially calcium carbonate-based ones like Tums, can cause rebound acid production, kidney stones, or high calcium levels. If you need daily relief, you likely need a different type of medication or to see a doctor.
Do H2 blockers stop working over time?
Yes. After 2 to 3 weeks of daily use, your body can become less responsive to H2 blockers like Pepcid. This is called tachyphylaxis. The acid suppression drops significantly, making them ineffective for long-term control. They’re best for short-term, predictable triggers - not daily management.
Why do PPIs take days to work?
PPIs don’t neutralize acid - they turn off the acid pumps in your stomach cells. These pumps are constantly being replaced. It takes 2 to 3 days of daily dosing to shut down enough pumps to significantly reduce acid. That’s why you need to take them before breakfast, every day, for at least 3 days to feel the full effect.
Is it safe to take PPIs for more than 14 days?
The FDA says no. OTC PPIs are labeled for 14-day use only. Taking them longer increases your risk of kidney damage, low magnesium, vitamin B12 deficiency, and bone fractures. If you still need relief after 14 days, see a doctor. You might have GERD or another condition that needs diagnosis and prescription treatment.
Can I take antacids with PPIs?
Yes - but only for breakthrough symptoms. Many people take Tums while on a PPI for sudden flare-ups. Just make sure to wait at least 2 hours between taking the antacid and any other medication, including the PPI. Don’t use antacids as a reason to keep taking PPIs longer than recommended.
Are generic PPIs as good as brand names?
Yes. Generic omeprazole, esomeprazole, and lansoprazole are bioequivalent to Prilosec, Nexium, and Prevacid. They contain the same active ingredient, meet the same FDA standards, and work the same way. The only difference is price - generics can cost 80% less. There’s no medical reason to pay more.
Next Steps
If you’re using OTC heartburn meds regularly, start here:
- Track your symptoms for a week. When does it happen? After what meals? At night?
- Stop taking PPIs if you’ve used them longer than 14 days. Switch to an H2 blocker or antacid temporarily.
- Try lifestyle changes: lose 5-10 pounds if overweight, avoid late-night eating, cut back on caffeine and alcohol.
- If symptoms persist after 2 weeks of lifestyle changes and proper OTC use, see a doctor. Don’t just keep buying pills.
Heartburn is manageable. But it’s not a problem you fix with a bottle. It’s a signal - and ignoring it can cost you more than money.







Ariel Nichole December 11, 2025
Love this breakdown. I used to pop Tums like candy until I realized I was making it worse. Switched to Pepcid before pizza night and my sleep actually improved. Who knew?
matthew dendle December 12, 2025
so ppi’s are just fancy acid blockers with a side of kidney damage? cool cool. guess i’ll keep chuggin’ omeprazole like it’s gatorade. 🤡
Jean Claude de La Ronde December 13, 2025
It’s funny how we treat our stomachs like broken faucets that need constant turning off. We don’t fix the pipe, we just keep mopping the floor. Maybe the real problem isn’t acid… it’s our entire relationship with food, stress, and time. Or maybe I just ate too much chili last night.
Mia Kingsley December 15, 2025
OMG I’ve been on PPIs for 3 years and you’re telling me I’m gonna get kidney failure?? I just turned 28 and already feel like an old man. This is a scam. I demand a refund from Big Pharma.
Aman deep December 16, 2025
Man, this hit different. I used to think heartburn was just ‘part of being a student who eats ramen at 2am.’ But after my cousin got diagnosed with Barrett’s esophagus, I started tracking my meals and sleeping upright. No pills. Just less coffee, no midnight snacks, and a pillow wedge. It’s not glamorous, but my chest doesn’t feel like it’s on fire anymore. You don’t need a pharmacy to heal - just awareness.
And yeah, generics are legit. I buy Curist like it’s my job. Same pill, $5 instead of $25. Save your cash for better things - like tacos.
To anyone still popping antacids daily: please stop. Your bones will thank you. Your kidneys will whisper sweet nothings. And your wallet? It’ll throw a party.
Also, losing 10 pounds didn’t just help my heartburn - it made me feel like I could breathe again. Not a miracle cure, but a quiet revolution.
Thanks for writing this. It’s rare to see someone actually care about helping people understand, not just sell them something.
Sylvia Frenzel December 16, 2025
Why are we even talking about OTC meds when the real issue is that Americans are too lazy to change their diets? We eat like garbage, then expect a pill to fix it. This isn’t medicine - it’s enabling.
Aileen Ferris December 18, 2025
hahah so ppi’s take days to work? wow i thought they were magic. guess i’ve been taking them wrong all this time. whoops.
Sarah Clifford December 19, 2025
so basically if you eat anything fun you’re doomed? why even live?
Regan Mears December 20, 2025
Great post - and I really appreciate how you highlighted the difference between symptom management and root-cause healing. So many people don’t realize that heartburn is often a signal, not the disease itself. I’ve seen patients on PPIs for years who never got a proper endoscopy. The real tragedy isn’t the side effects - it’s the missed diagnoses.
Also, the 14-day rule is non-negotiable. If you need it longer, you’re not treating heartburn - you’re treating an undiagnosed condition. Please, if you’re reading this and you’ve been on PPIs for months: make an appointment. Not next week. Now.
And yes - lifestyle changes work better than pills. I’ve had patients reverse their GERD with weight loss, sleep posture, and cutting out soda. No drugs. Just discipline. It’s not sexy, but it’s real.
Also - generics are absolutely fine. I prescribe them every day. Save your money. Spend it on a personal trainer instead.
Ben Greening December 22, 2025
Interesting. I’ve been using famotidine for two weeks and noticed it’s less effective now. I assumed I was building tolerance. This explains why. Will switch to antacids for flare-ups and reevaluate.
Vivian Amadi December 22, 2025
You’re all wrong. Heartburn is caused by low stomach acid. Acid blockers make it worse. Take apple cider vinegar. Done.
Ariel Nichole December 24, 2025
Wait… apple cider vinegar? I tried that once and nearly cried. My esophagus felt like it was on fire. Also, low acid doesn’t explain why I feel better when I stop eating pizza at midnight.