Imagine looking at a street sign, but the letters blur and double like ripples in water. For someone with keratoconus, this isn’t a temporary glitch-it’s everyday life. The cornea, normally smooth and dome-shaped, starts to thin and bulge outward into a cone. This isn’t just blurry vision. It’s distorted, flickering, and often uncorrectable with regular glasses. By the time most people realize something’s wrong, the condition has already progressed. But there’s a solution that’s been helping millions for decades: rigid contact lenses.
What Happens When the Cornea Thins?
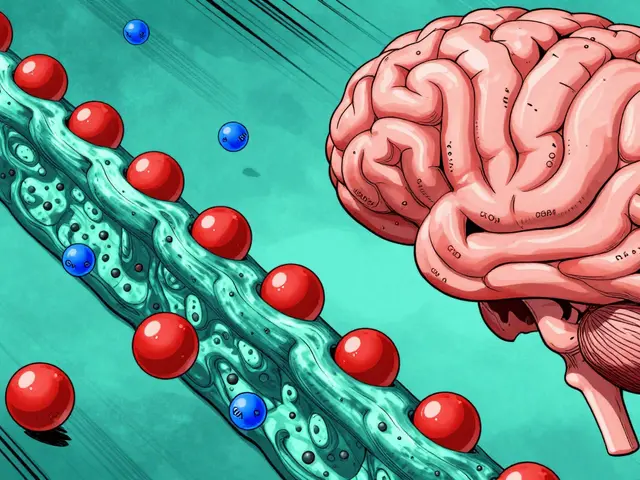
Keratoconus doesn’t strike suddenly. It creeps in during the teens or early 20s, often starting in one eye before affecting the other. The cornea’s structure weakens because enzymes break down collagen faster than the body can repair it. Think of it like a balloon slowly losing its shape-the center pushes forward, creating an irregular curve. This isn’t just a surface problem. The thinning happens in layers, and the steepest part, the cone, becomes the most distorted. Standard glasses can’t fix this. They sit too far from the eye and can’t compensate for the uneven surface. Even soft contact lenses, which conform to the shape of the eye, just mold to the irregularity instead of correcting it. The result? Vision that’s consistently 20/400 or worse-meaning you’d need to stand 20 feet away to see what someone with normal vision sees at 400 feet.Why Rigid Lenses Work When Everything Else Fails
Rigid gas permeable (RGP) lenses are the first-line defense. Unlike soft lenses, they don’t bend. They keep their shape and sit on the cornea like a tiny, clear dome. The magic? They create a new, smooth optical surface over the crooked cornea. Tears fill the tiny gap between the lens and the cornea, acting like a liquid buffer that evens out the irregularities. Studies show patients go from seeing only 20/400 to 20/200-or better-after getting properly fitted RGP lenses. That’s not a small improvement. It’s the difference between recognizing a face across the room and not being able to tell if it’s a person at all. Scleral lenses take this further. These are larger-15 to 22 millimeters wide-and vault completely over the cornea, resting on the white part of the eye (the sclera). They hold a reservoir of saline between the lens and the cornea, which not only improves vision but also soothes a damaged surface. For someone with advanced keratoconus, this can mean the difference between wearing a lens and wearing nothing at all.How Rigid Lenses Compare to Other Treatments
Corneal cross-linking (CXL) is the only treatment proven to stop keratoconus from getting worse. It uses UV light and riboflavin to strengthen the cornea’s collagen fibers. But CXL doesn’t fix blurry vision-it just stops it from getting worse. You still need lenses afterward. INTACS, tiny plastic inserts placed in the cornea, can flatten the cone a bit. But even after surgery, 35 to 40% of patients still need rigid lenses to see clearly. Corneal transplants-replacing the damaged cornea with donor tissue-are reserved for the worst cases. About 10 to 20% of patients end up needing one. But transplants come with risks: rejection (5-10%), long recovery (over a year), and lifelong steroid eye drops. Rigid lenses don’t cure keratoconus. But they’re the most effective, non-invasive way to restore functional vision. They’re not a last resort-they’re the standard.
What to Expect When You Start Wearing Rigid Lenses
Fitting isn’t a one-time visit. It takes 3 to 5 appointments over 4 to 6 weeks. Your eye doctor uses a topographer to map your cornea’s shape, then tries different lens designs. One might fit well but feel uncomfortable. Another might be comfortable but blur your vision slightly. Finding the right match is like tuning a guitar-small adjustments make all the difference. Adapting takes time. Most people start with just 2 to 4 hours a day. Gradually, they add an hour or two each day. Within 2 to 4 weeks, 85% of patients are wearing them full-time. But the first week? It’s rough. Forty-five percent feel like there’s something in their eye. Thirty-eight percent are hyper-aware of the lens. Thirty-two percent struggle with putting them in or taking them out. The good news? These issues fade. Once you get used to them, most users report sharper vision, less glare, and better contrast. One patient from Bristol described it like switching from a foggy window to a clean one-suddenly, colors were brighter, faces were clearer, and driving at night didn’t feel like a gamble.Common Problems and How to Solve Them
Not every lens works perfectly. Here’s what can go wrong-and how to fix it:- Lens fogging (25% of users): Caused by protein buildup or poor cleaning. Switch to a preservative-free cleaning solution and clean daily with a recommended brush.
- Lens decentration (15%): The lens shifts off-center. This often means the curve doesn’t match your cornea. A topography-guided redesign usually fixes it.
- Solution sensitivity (10%): Redness or stinging from cleaning solutions. Try preservative-free rewetting drops or switch to a different disinfectant.
- Chronic dry eye: Makes lens wear unbearable. Artificial tears formulated for contact lens wearers help. In severe cases, scleral lenses are often the answer because they trap moisture under the lens.

Who Should Use Scleral Lenses vs. RGP Lenses?
Not all rigid lenses are the same. RGP lenses are smaller (9-10 mm), cheaper, and easier to handle. They’re great for early to moderate keratoconus. But if your cornea is severely irregular or scarred, they won’t fit well. That’s where scleral lenses come in. Scleral lenses have a 85% success rate in advanced cases (Stage III-IV), compared to 65% for RGP lenses. They’re bulkier, more expensive, and require more training to use. But for people who’ve tried everything else and still can’t see, they’re life-changing. New materials now allow oxygen permeability (Dk) values over 200-higher than ever before. This means less risk of corneal swelling, even with all-day wear. And since January 2023, the FDA has approved digital manufacturing for fully customized scleral lenses. Your lens isn’t just picked from a catalog-it’s designed from your exact corneal scan.Long-Term Outlook: Can You Avoid Surgery?
The good news? Most people with keratoconus never need a transplant. Even with progression, rigid lenses keep vision functional for decades. The American Academy of Ophthalmology reports that 60-70% of diagnosed patients rely on rigid lenses as their primary correction. That’s 6 out of 10 people. Combined treatment is becoming the norm. Around 78% of cornea specialists now pair CXL with rigid lenses. CXL stops the thinning. Lenses restore the sight. Together, they give patients the best chance at long-term vision without surgery. The market for these lenses is growing fast. It’s projected to hit $2.78 billion by 2027. More clinics now offer specialized fitting, and insurance coverage is slowly improving. What used to be a niche solution is now standard care.What Comes Next?
If you’ve been diagnosed with keratoconus, your first step isn’t panic-it’s evaluation. Get a corneal topography scan. Talk to a specialist who fits rigid lenses regularly. Don’t settle for glasses if your vision is still blurry. Don’t rush into surgery unless you’ve tried lenses first. The truth is, keratoconus doesn’t have to mean losing your sight. It means learning a new way to see. And for most people, that new way comes in the form of a small, rigid lens that sits gently on the eye-and changes everything.Can glasses correct keratoconus?
No, glasses cannot correct keratoconus effectively. Because the cornea becomes irregularly shaped, glasses sit too far from the eye to compensate for the distortion. They may help slightly in early stages, but most patients quickly outgrow their benefit. Rigid contact lenses are needed to create a smooth optical surface that glasses can’t provide.
Are rigid contact lenses uncomfortable?
Initially, yes-about 30% of patients experience discomfort during the first few weeks. Common complaints include a foreign body sensation, lens awareness, and difficulty inserting or removing them. But most adapt within 2 to 4 weeks. Once adjusted, many users report they forget they’re wearing them. Scleral lenses, which vault over the cornea, tend to be more comfortable than traditional RGP lenses, especially for advanced cases.
Do rigid lenses stop keratoconus from getting worse?
No, rigid lenses only correct vision-they don’t halt progression. To stop the cornea from thinning further, corneal cross-linking (CXL) is required. CXL is the only FDA-approved treatment that strengthens the cornea’s collagen fibers. Most eye care professionals now recommend combining CXL with rigid lenses for both vision correction and disease management.
How long do rigid lenses last?
Rigid gas permeable (RGP) lenses typically last 1 to 2 years with proper care. Scleral lenses, being larger and made of more durable materials, often last 2 to 3 years. Lifespan depends on cleaning habits, tear chemistry, and how often they’re worn. Regular check-ups ensure the fit hasn’t changed as your cornea evolves.
Can you sleep in rigid contact lenses for keratoconus?
No, you should never sleep in rigid gas permeable or scleral lenses. These lenses are not designed for overnight wear. Sleeping in them increases the risk of corneal hypoxia (oxygen deprivation), infection, and ulcers. Always remove, clean, and store them in fresh solution before bed. Some patients use overnight CXL treatments, but that’s a medical procedure, not lens wear.
Is keratoconus treatment covered by insurance?
Coverage varies. Medical insurance often covers corneal cross-linking (CXL) as a medically necessary procedure. Specialty contact lenses like scleral or RGP lenses are sometimes covered under vision plans, but often require prior authorization. Many insurers classify them as medical devices, not cosmetic, so documentation from your eye doctor can help. Always check with your provider and ask for a letter of medical necessity.
What’s the success rate of scleral lenses for advanced keratoconus?
Scleral lenses have an 85% success rate in advanced keratoconus cases (Stage III-IV), compared to 65% for traditional RGP lenses. Their larger size and fluid reservoir make them ideal for irregular, scarred, or sensitive corneas. Many patients who couldn’t tolerate other lenses find they can wear sclerals comfortably for 12+ hours a day, with visual acuity improving from 20/80 to 20/25 on average.
Do I need to get a corneal transplant if I have keratoconus?
Only about 10-20% of people with keratoconus eventually need a corneal transplant. Most cases are managed successfully with rigid lenses and cross-linking. Transplants are reserved for those who can’t tolerate lenses, have severe scarring, or have failed other treatments. Even after transplant, many patients still need contact lenses to achieve optimal vision.
If you’re living with keratoconus, you’re not alone-and you’re not out of options. Rigid lenses aren’t a perfect fix, but they’re the most reliable, non-surgical tool we have to restore clear vision. With better materials, smarter fitting, and combined therapies, most people can live full, active lives without ever needing a transplant.





Joe Lam December 5, 2025
Rigid lenses? Please. I’ve been wearing custom sclerals for 8 years and let me tell you - this article reads like a pharmaceutical brochure written by a sales rep who’s never held a lens in their hand. The real magic isn’t the lens - it’s the $3,000 topographer that maps your cornea like a damn satellite survey. And don’t even get me started on how most optometrists still treat this like a one-size-fits-all problem. You need a specialist. Not some guy who fits contacts on weekends.
Also - ‘non-invasive’? Please. You’re literally gluing a plastic dome to your eyeball. That’s not medicine, that’s bioengineering with a side of existential dread.
Jenny Rogers December 5, 2025
It is, indeed, a profound tragedy of modern medicine that we have reduced the human ocular system - a marvel of evolutionary architecture - to a mere engineering problem solvable by synthetic polymers and saline reservoirs. One cannot help but wonder: in our haste to correct the symptom, have we forgotten to honor the sanctity of the cornea’s natural design? The body, when left undisturbed by artificial intervention, possesses an innate wisdom that our technological arrogance too often dismisses. Is it not humility, rather than rigid lenses, that should be our first recourse?
Benjamin Sedler December 7, 2025
Wait - so you’re telling me the solution to a cornea that’s melting like a candle in a sauna… is to slap a tiny plastic saucer on it and call it a day? Brilliant. Next they’ll invent a helmet for your brain so you don’t think too hard.
Also - ‘tears act as a liquid buffer’? That’s not science, that’s a poet’s fantasy. My tears are salty, emotional, and occasionally contain regret. They don’t fix optics. They just make the lens stick to your eyelid like a sad little sticker.
Carolyn Ford December 8, 2025
Let me be crystal clear: if you’re still using soft contacts for keratoconus, you’re not just misinformed - you’re endangering your vision!!
And yes, CXL is mandatory!!
And no, you don’t get to skip the topography scan!!
And yes, insurance will fight you - but you fight harder!!
This isn’t a lifestyle choice - it’s a medical imperative!!
And if you think glasses are ‘fine for now’ - you’re one blurry bus ride away from a corneal transplant!!
Heidi Thomas December 9, 2025
Everyone’s overcomplicating this. Rigid lenses work. Sclerals work better. CXL stops it from getting worse. Done. Stop writing novels about it. Just get fitted. Stop scrolling. Your vision won’t fix itself.
Also stop saying ‘non-invasive’ - it’s a lens. You put it in your eye. That’s invasive. Stop marketing spin.
Gillian Watson December 11, 2025
Interesting piece. I’ve got a mate in Bristol who’s been on sclerals since 2019 - says it’s like going from watching TV through a foggy window to 4K HDR. Took him six months to get used to inserting them, but now he forgets they’re there. He even does yoga with them in. Wild.
Still, I reckon the real win here is how the tech’s evolved. Digital scans, custom designs - feels like we’re finally treating the person, not just the condition.
Gareth Storer December 12, 2025
So let me get this straight. The cure for a cornea that’s turning into a cone… is to put a tiny plastic dome on it and pretend it’s not a medical emergency?
Next up: we’ll replace your spine with a pencil and call it ergonomic.
Also, who approved this article? A marketing intern who just got their first pair of contacts?
Pavan Kankala December 13, 2025
They don’t want you to know this - but rigid lenses are just a distraction. The real cause? 5G radiation frying your corneal nerves. That’s why it hits teens - they’re on their phones 12 hours a day. The FDA? Owned by lens manufacturers. CXL? A placebo with UV light. Sclerals? A profit engine. They’re selling you comfort so you forget you’re being manipulated.
Go outside. Look at the sun. Let your eyes heal naturally. No plastic. No chemicals. No lies.
Jessica Baydowicz December 14, 2025
Okay I just got fitted for my first RGP lenses last week and I’m crying - not from pain, from relief. I’ve been squinting at my kid’s school play for two years thinking I was just getting old. Turns out my cornea’s been slowly turning into a potato. These lenses? They’re like putting on glasses for the first time - but way better. I can see the eyelashes on my cat now. I’m not joking.
To anyone scared to try: you’re not broken. You’re just waiting for the right tool. And that tool? It’s out there.
Yasmine Hajar December 14, 2025
I’m a mom of a 16-year-old with keratoconus - and I can’t tell you how many times I’ve wanted to scream at doctors who said ‘just wait and see.’
This article? It’s the first one that didn’t make me feel like I was failing my kid.
Yes, the fitting process is a nightmare. Yes, the lenses feel like alien objects. But the first time she saw her own face clearly in the mirror after two weeks? She didn’t say a word. Just hugged me so hard I thought I’d break.
You’re not alone. We’re all just trying to see - literally and figuratively.
George Graham December 15, 2025
My brother’s been on sclerals for 10 years. He’s a mechanic - works with grease, dust, sweat. Still wears them 14 hours a day. Never had an infection. Never needed a transplant.
What this article doesn’t say enough is: the real hero isn’t the lens. It’s the optometrist who actually listens. The one who spends 90 minutes tweaking a curve because you said ‘it feels like a rock.’ That’s the magic. Not the tech. The person behind it.
John Filby December 16, 2025
Just got my first pair of RGPs last month 😅
Day 1: felt like I had a bug in my eye
Day 7: could read the license plate on a car 3 blocks away
Day 14: forgot I was wearing them
Also - the cleaning solution? Don’t use the cheap stuff. Got a rash. Switched to preservative-free and boom - no more stinging. Just a heads up for anyone new to this.
Elizabeth Crutchfield December 17, 2025
i got my first scleral lenses last year and omg they changed my life like i could finally read the clock without squinting and now i drive at night and dont feel like im gonna crash
the fitting was a mess tho like 5 appointments and i cried twice but worth it
also pls use the right solution dont be like me and use tap water
Chad Handy December 19, 2025
Let me tell you about the time I spent six months trying to get these lenses right. I was so desperate I tried wearing them while sleeping. I woke up with my eye glued shut, swollen, and screaming. The ER doctor looked at me like I’d tried to microwave my face.
Turns out, the ‘non-invasive’ solution is actually a slow-motion assault on your cornea. They don’t tell you that the lenses cause chronic dryness that feels like sandpaper over your optic nerve. They don’t tell you that your tears stop working because your eye thinks it’s under siege.
And now? I’ve got permanent corneal neovascularization. Blood vessels crawling across my eye like tiny spiders. Because I trusted the ‘standard care.’
I’m not saying don’t use them. I’m saying: if you’re going to do this, go full research mode. Read the journals. Talk to patients who’ve had transplants. Don’t let a 10-minute YouTube ad convince you this is harmless.
I’m 32. I’ve lost 60% of my vision. And I still have to wear them. Every. Single. Day.
So yeah. ‘Restores vision.’ Maybe. But at what cost?
Rebecca Braatz December 19, 2025
Hey everyone - if you’re new to this, I’ve been helping folks through keratoconus for 7 years now. You’re not broken. You’re not behind. You’re just early in the journey.
That first week with rigid lenses? It’s brutal. You’ll feel like you’re wearing a helmet made of glass. But here’s the secret: the discomfort fades faster than you think.
And if you’re scared to ask for a second fitting? Do it. Your doctor wants you to succeed. This isn’t a ‘one-size-fits-all’ game. It’s a custom build.
And if you’re wondering whether you’re ‘bad’ at wearing them? No. You’re just learning. I’ve seen people go from crying to driving at night in 3 weeks.
You’ve got this. And you’re not alone.