Every time you pick up a prescription, you’re holding a document that could save your life-or hurt you if you don’t understand it. Prescription labels aren’t just small slips of paper with random letters and numbers. They’re your main safety net against medication errors. And yet, prescription label misunderstandings cause over 1.3 million medication errors in the U.S. every year, according to the FDA. That’s not a small number. It’s not something you should ignore.
What’s on Your Prescription Label? (The 9 Must-Check Items)
Your prescription label has nine key pieces of information that every pharmacy is required to include. Don’t assume they’re all there or correct. Always check them yourself.
- Patient name - Is it spelled right? Is it yours? A mix-up here can lead to someone else’s medication ending up in your hands.
- Prescriber name - Does this match the doctor who wrote the script? If not, ask why.
- Drug name - Both brand and generic names should appear. If you’re used to taking lisinopril but see Zestril on the label, that’s the same thing-but you should confirm it.
- Strength - Is it 5 mg, 10 mg, or 20 mg? A wrong strength is one of the most common causes of overdose.
- Dosage form - Is it a tablet, capsule, liquid, or patch? If you expected a pill but got a liquid, double-check.
- Quantity - How many pills or mL are you getting? If your refill should be 30 pills but you got 60, ask why.
- Directions for use - This is the most important part. Does it say “take one by mouth twice daily” or “take one every 6 hours”? These are very different.
- Number of refills - How many times can you get this filled? If you need more than what’s listed, you’ll need a new prescription.
- Pharmacy contact info - Save this. You’ll need it if you have questions later.
These aren’t optional. They’re the law. If any of these are missing or wrong, the pharmacy has to fix it before you leave.
Ask About the ‘5 Rights’ - Your Personal Safety Checklist
The Institute for Safe Medication Practices created the ‘5 Rights’ system to stop medication errors. It’s simple. You can use it every time you get a new prescription.
- Right Patient - Is this label really for you? Check your full name and date of birth.
- Right Medicine - Does the drug name match what your doctor told you? Don’t trust the brand name alone.
- Right Amount - Is the dose correct? If you’re used to 10 mg and now it’s 20 mg, ask if this is intentional.
- Right Way - Should you take it with food? On an empty stomach? With water? Can you crush it? Some pills must be swallowed whole.
- Right Time - Is it once a day? Twice? Every 8 hours? Timing matters for effectiveness and safety.
Repeat these out loud to the pharmacist. If you can’t say them back clearly, they haven’t explained it well enough. Studies show patients who do this reduce medication errors by up to 58%.
What About Storage? Don’t Assume It’s Fine on the Counter
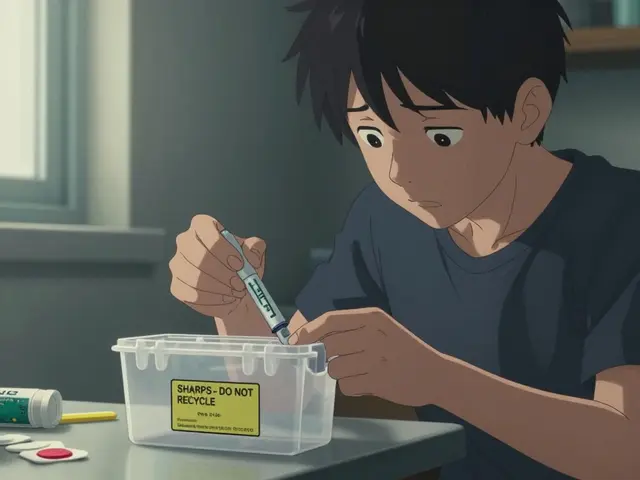
Most people think all meds can sit in a bathroom cabinet. That’s wrong. About 15% of prescription drugs need to be refrigerated. If you store insulin, certain antibiotics, or some eye drops at room temperature, they can lose effectiveness-or become dangerous.
Check the label for storage instructions. Look for phrases like:
- “Store in refrigerator between 36°F and 46°F”
- “Keep at room temperature, away from moisture and heat”
- “Protect from light”
A 2022 survey found that nearly 1 in 5 patients didn’t realize their meds needed cold storage. One woman in Alabama kept her insulin in her medicine cabinet for two weeks because the label was printed in tiny font on the back. Her blood sugar spiked. She ended up in the ER.
Ask: “Does this need to be kept cold? Where should I store it?” If you don’t ask, you might be taking a drug that doesn’t work.
Expiration Dates and Refills - Don’t Guess
Expiration dates aren’t suggestions. They’re science. The FDA requires that drugs remain effective and safe until that date-if stored properly. But many people keep pills past their expiration, thinking they’re still fine.
Ask: “Is this still good until the date on the label?”
Also, check your refill count. If it says “0 refills,” you can’t just walk back in and ask for more. You need a new prescription. Some pharmacies will let you refill early if you’re traveling, but they’re not required to. Ask about refill policies upfront.
And if you’re on Medicare Part D, your refill eligibility might be tied to your coverage tier. Don’t assume you can refill whenever you want. Ask the pharmacist if your plan allows it.

What If the Label Is Hard to Read?
Small print, blurry ink, confusing abbreviations-these aren’t just annoyances. They’re safety risks. About 80 million American adults struggle to read medical instructions. That’s not a personal failure. It’s a system failure.
You have the right to ask for:
- Large-print labels - 92% of U.S. pharmacies offer them for free.
- Verbal explanation - Ask the pharmacist to walk you through the label again. Don’t be shy.
- Translation services - If you’re not fluent in English, the pharmacy must provide a translator under the Affordable Care Act.
- Written instructions - Request a printed summary of your dosing schedule.
One Reddit user shared how their pharmacist at a small independent pharmacy printed out a simple chart: “Monday/Wednesday/Friday: 1 pill after breakfast. Tuesday/Thursday: 1 pill after dinner.” That made all the difference.
What Are the Side Effects? Don’t Wait for the Paper
Prescription labels don’t list every possible side effect. That’s what Medication Guides are for. The FDA requires these guides for 107 high-risk drugs, including opioids, blood thinners, antidepressants, and diabetes meds.
Ask: “Do I get a Medication Guide with this?” If they say no, ask why. If they hand you a 3-page document, read it. Don’t just put it in your bag.
Also ask: “What side effects should I watch for right away?” For example, if you’re on a blood thinner, you need to know signs of internal bleeding-unusual bruising, dark stools, severe headaches. If you’re on an antibiotic, ask if it interacts with dairy or alcohol.
What About Interactions? Food, Alcohol, Other Meds
Some drugs don’t work if you take them with food. Others become toxic with alcohol. Grapefruit juice can interfere with over 85 medications, including statins and blood pressure pills.
Ask: “What should I avoid eating, drinking, or taking with this?”
Also, tell the pharmacist about everything else you take-even vitamins, supplements, or over-the-counter painkillers. Many people don’t think of Tylenol or fish oil as “meds,” but they can interact.
One man in Ohio took his cholesterol pill with grapefruit juice every morning. He didn’t know it could cause muscle damage. His pharmacist caught it when he picked up a new script. He said, “I’d have been in the hospital if you hadn’t asked.”

Are There Digital Options? QR Codes and Apps
More pharmacies are using QR codes on labels that link to video instructions. In 2022, pharmacies using this system saw a 31% drop in medication errors. Some even use AI tools that scan your label and flag risks.
Ask: “Is there a QR code on this label? Can I scan it to see a video of how to take this?”
If the pharmacy doesn’t offer it, ask if they plan to. The FDA is pushing for all high-risk meds to have scannable labels by 2026. You’re not asking for a luxury-you’re asking for better safety.
What If You’re Still Confused?
It’s okay to say, “I don’t understand.”
You can ask to speak with the pharmacist again. You can call the pharmacy later. You can ask your doctor to clarify. You can use the FDA’s free Medication Check-Up program, available at over 8,400 pharmacies nationwide.
And if you’re still unsure? Don’t take the pill. Call someone. Wait. Get help. A wrong dose can kill you. A quick question now saves a hospital trip later.
Final Thought: Your Label Is Your Lifeline
Prescription labels are designed to protect you. But they only work if you use them. Don’t be passive. Don’t assume. Don’t nod and walk away.
Ask the questions. Read the fine print. Verify the details. If the pharmacist seems rushed, ask to come back later. If they’re dismissive, go to another pharmacy. Independent pharmacies often spend more time with patients-they scored 4.3 out of 5 on Trustpilot for labeling clarity, compared to 3.1 for big chains.
Every time you pick up a prescription, you have two minutes. Use them. Ask five questions. Check the five rights. Confirm the storage. Know the side effects.
That’s not being difficult. That’s being smart. And it might just save your life.
What should I do if the pharmacy gives me the wrong medication?
If you notice the medication looks different from what you usually take, or the name doesn’t match your prescription, stop. Don’t take it. Ask the pharmacist to double-check the script and the bottle. If they confirm it’s wrong, ask them to contact your doctor for a corrected prescription. Report the error to the pharmacy manager and consider filing a report with your state’s Board of Pharmacy. Wrong medications can cause serious harm-never ignore a mismatch.
Can I ask for a printed summary of my dosing schedule?
Yes, absolutely. You have the right to request a simple, written schedule that breaks down when and how to take each medication. Many pharmacies offer this for free, especially for patients managing multiple drugs. A clear chart like “Take 1 pill at 8 a.m. with breakfast, 1 at 8 p.m.” is far easier to follow than reading small text on a label. Ask for it when you pick up your prescription.
Why do some labels have both brand and generic names?
Federal law requires both names to appear on prescription labels so you know exactly what you’re taking. The brand name (like Lipitor) is what your doctor may have written, but the generic (atorvastatin) is the actual drug. Insurance often pushes for generics because they’re cheaper. Seeing both helps you confirm you’re getting the right drug, even if the name changed from your last refill.
What if I can’t read the label because of poor eyesight?
You’re not alone. Over 7.6 million Americans over 45 have vision problems. Pharmacies are legally required to provide large-print labels upon request-no extra cost. Just say, “I need this in large print.” Most pharmacies have special printers for this. You can also ask for a verbal explanation or a printed summary. Don’t struggle to read tiny text-your safety matters more than pride.
Do I need to ask about side effects every time I get a refill?
Yes. Even if you’ve taken the same drug before, side effects can change. Your body changes. Other meds you’re taking might change. The label might have been updated. Always ask, “Are there any new warnings or side effects I should know about?” The FDA updates safety info regularly. What was safe last year might not be this year.





Christina Bischof December 15, 2025
I used to just grab my scripts and leave. Then my grandma had a bad reaction because she didn't check the refill count. Now I ask every single time. It's not weird-it's wise. 🙏
RONALD Randolph December 15, 2025
The FDA says 1.3 million errors? That’s a national disgrace. Pharmacies are legally obligated to verify every single item on that label-no excuses. If they’re rushing you, file a complaint with your state board immediately.
Sai Nguyen December 16, 2025
Why do Americans make everything so complicated? In India, we just take what the doctor gives. No questions. No labels. Life is simpler.
Lisa Davies December 17, 2025
This is the kind of post that makes me love Reddit. 🌟 Seriously, if you're on meds, read this twice. Then show it to your parents. Or your neighbor. Or your cousin who thinks 'it's just a pill'.
Jocelyn Lachapelle December 18, 2025
I got my first big prescription last year and was terrified. I asked the pharmacist to explain the 5 rights out loud. She smiled and said, 'I wish more people did that.' It felt like a tiny victory.
Cassie Henriques December 20, 2025
QR codes on labels? That’s a game-changer. The AI flagging system in my CVS app already warned me about a potential interaction between my statin and a new OTC supplement. FDA’s pushing for this for a reason-this isn’t tech for tech’s sake, it’s harm reduction at scale.
Melissa Taylor December 21, 2025
I always ask for the large-print label. I’m 68 and I don’t need to squint to stay alive. Pharmacies should be required to offer it without being asked. It’s basic accessibility.
Raj Kumar December 23, 2025
I work at a small pharmacy in Chicago and we do this stuff automatically. We print charts, we use big fonts, we ask if they need a translator. It takes 2 extra minutes but saves lives. Why don't the big chains just do this?
Nupur Vimal December 24, 2025
You think your label is hard to read? Try being on 12 meds and having a pharmacist who thinks 'take one daily' means 'take one whenever you remember'. I've been doing this for 15 years and I still get it wrong
Mike Nordby December 26, 2025
The 5 Rights framework is evidence-based and universally applicable. It is not a suggestion-it is a clinical standard. Patients who verbalize these rights demonstrate improved medication adherence and reduced adverse events. This is not anecdotal. It is peer-reviewed.
Jake Sinatra December 28, 2025
I used to think asking questions made me annoying. Then I realized: if I don’t ask, someone else might have to bury me. I now say, 'Can you walk me through this?' every single time. It’s not a burden-it’s a right.
Benjamin Glover December 28, 2025
Americans overcomplicate everything. In the UK, we trust the pharmacist. If you can’t read the label, get glasses. Not a new policy.
Michelle M December 29, 2025
It’s funny how we treat our bodies like machines we’re too lazy to read the manual for. But we’ll spend hours reading the instructions for a toaster. Maybe we need to treat our pills like they matter-because they do.
John Samuel December 30, 2025
I’ve been a pharmacist for 22 years. I’ve seen people die because they didn’t ask if their blood thinner interacted with grapefruit juice. I’ve seen people live because they asked. Don’t be the statistic. Ask. Even if it feels silly. Even if they seem busy. Even if you’re embarrassed. Your life is not a sacrifice to politeness.
John Brown December 31, 2025
My mom’s in her 70s. I printed out the 5 Rights on a sticky note and stuck it to her pill organizer. She says it’s the only thing that makes her feel safe. Small things. Big impact.