Steroid-Induced Diabetes Risk Calculator
Your Steroid Information
Your Risk Factors
Your Risk Assessment
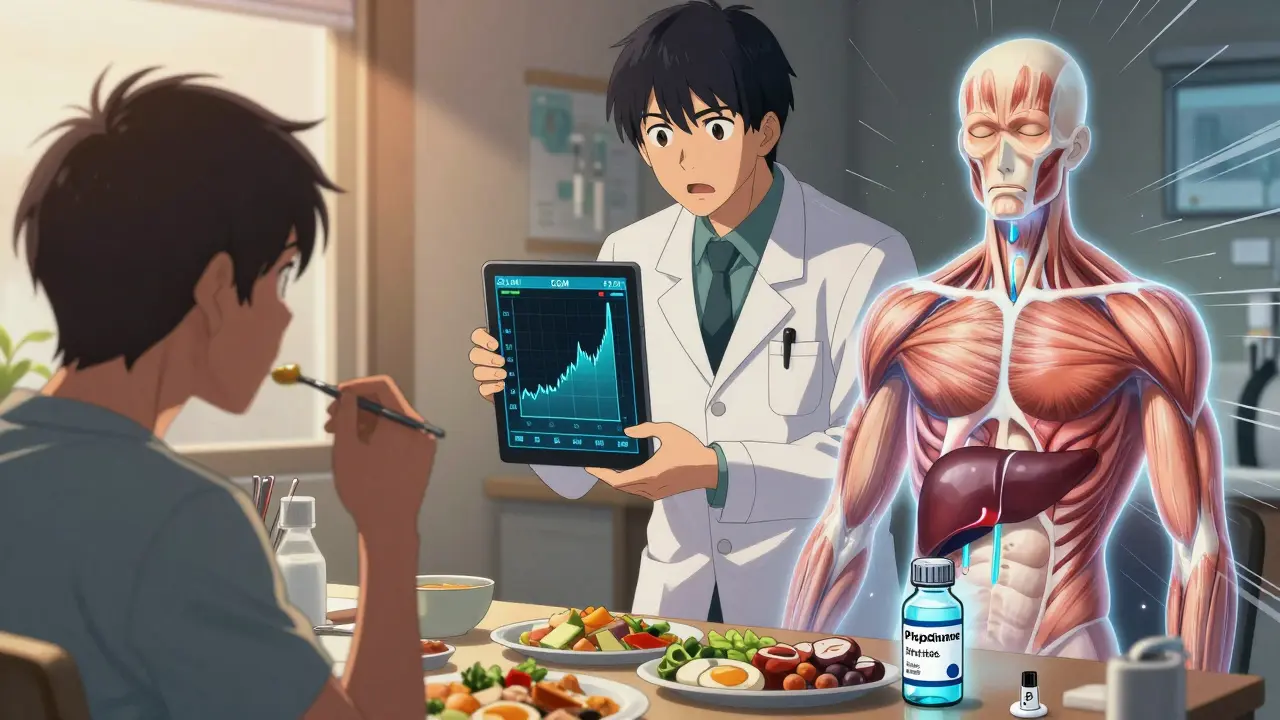
Why corticosteroids raise your blood sugar
When you take corticosteroids like prednisone or dexamethasone, your body doesn’t just fight inflammation-it also starts spiking your blood sugar. This isn’t a side effect you can ignore. Around 20-50% of people on high-dose steroids develop high blood sugar, even if they’ve never had diabetes before. It happens fast-sometimes within 24 to 48 hours of starting the medication.
The problem isn’t just that steroids make you hungrier or cause weight gain. They directly mess with how your body handles glucose. In your liver, steroids turn on the faucet for glucose production, boosting it by 35-40%. Your liver starts making more sugar than your body needs, even when you haven’t eaten. At the same time, your muscles and fat tissue stop responding to insulin like they used to. This is called insulin resistance. Your cells basically say, “We’re not taking any more glucose today,” so sugar builds up in your blood.
And it gets worse. Your pancreas, the organ that makes insulin, starts to slow down. Steroids reduce the number of glucose sensors on insulin-producing beta cells, so they don’t even know when blood sugar is high. Studies show insulin secretion drops by 20-35%. You’re left with too much sugar in your blood and not enough insulin to move it out. That’s the perfect storm for steroid-induced diabetes.
Who’s most at risk?
Not everyone on steroids gets high blood sugar. But some people are much more likely to. If you’re over 50, your risk jumps by more than three times. If you’re overweight (BMI 25 or higher), your risk goes up by 2.5 times. A family history of diabetes? That adds another 2.7 times the risk. And if you’ve had gestational diabetes before, your chance of developing steroid-induced diabetes is more than four times higher.
Dose matters. Taking just 7.5 mg of prednisone daily triples your risk. Dexamethasone is even stronger-0.75 mg daily increases risk nearly threefold. The longer you’re on steroids, the worse it gets. Each week past the first two weeks raises your risk by 12%. And if you’re on more than 20 mg of prednisone a day, your chances of needing treatment for high blood sugar jump dramatically.
People with kidney problems are also at higher risk. If your eGFR is below 60, your risk increases by 3.8 times. That’s because your kidneys can’t help clear excess glucose as well, and insulin clearance slows down too. Even if you feel fine, if you fall into one of these categories, you need to be monitored closely.
What symptoms should you watch for?
Some people feel it right away. Sixty-five percent report extreme thirst. Seventy-two percent are peeing more often than usual. Eighty-one percent say they’re constantly tired, even after sleeping. Forty-three percent get headaches. But here’s the catch: 40% of people show no symptoms at all. That’s why routine blood sugar checks are critical.
Other signs can be tricky because they overlap with steroid side effects. You might feel hungrier than normal-85% of steroid users do. You might gain weight-2.5 to 4 kg in the first month is common. Blurred vision? That happens in 32% of cases. Mood swings? That’s 67%. These aren’t just “side effects.” They could be signs of high blood sugar.
Many patients on Reddit and other forums say they weren’t warned. Sixty-eight percent reported their doctor never mentioned the risk. That’s a gap in care. If you’re prescribed steroids for more than a few days, ask for a blood glucose test before you start and again after a few days. Don’t wait for symptoms.
How doctors test and monitor for steroid-induced diabetes
Monitoring isn’t optional-it’s standard. The NIH recommends checking blood sugar at least twice a day if you’re on prednisone 20 mg or higher daily. Some hospitals check it before breakfast and before dinner. Others check it 4-8 hours after your morning steroid dose, because that’s when blood sugar usually peaks.
The thresholds for action are clear: if your fasting glucose is above 140 mg/dL (7.8 mmol/L) or your random glucose is above 180 mg/dL (10.0 mmol/L), you need treatment. For people who already have type 2 diabetes, insulin needs often jump by 50-100% during steroid therapy.
Doctors use different tools. Some rely on finger-prick tests. Others use continuous glucose monitors (CGMs), especially in hospitals. A CGM can show you how your sugar moves throughout the day, which is especially useful because steroid-induced highs don’t follow meal patterns. They follow the steroid dose. If you take prednisone at 8 a.m., your sugar might not peak until 2 p.m. That’s why timing matters.
How it’s treated: insulin is often the best choice
Oral diabetes pills? They’re not always the answer. Sulfonylureas (like glipizide) force your pancreas to make more insulin, but that’s risky when steroids are tapering off. Your insulin production might not bounce back fast enough, and you could crash into low blood sugar. In fact, 37% of hypoglycemia cases linked to steroid use happen when the steroid dose is lowered too quickly.
That’s why insulin is the go-to treatment. Basal insulin (long-acting) helps control the liver’s sugar output. Rapid-acting insulin covers meals. The University of California San Francisco recommends increasing basal insulin by 20% for every 10 mg increase in prednisone above 20 mg/day. For meals, one unit of rapid-acting insulin for every 5-10 grams of carbs usually works.
Some newer options are being tested. GLP-1 receptor agonists (like semaglutide) are showing promise in early trials. They help your body make insulin only when blood sugar is high, reduce appetite, and lower the risk of low blood sugar. In the GLUCO-STER trial, patients on GLP-1 drugs had 28% fewer episodes of hypoglycemia than those on insulin.
But insulin remains the most reliable. It’s fast-acting, adjustable, and doesn’t rely on your pancreas working properly-which, remember, is already suppressed by the steroids.

What happens when you stop the steroids?
Here’s the good news: steroid-induced diabetes usually goes away. Once you stop taking the steroids, your blood sugar levels typically return to normal within 3 to 5 days. Your liver stops overproducing glucose. Your muscles start responding to insulin again. Your pancreas wakes up.
But here’s the catch: many patients don’t know this. Sixty-three percent keep taking diabetes meds long after they’ve stopped steroids. That’s dangerous. Continuing sulfonylureas or even insulin without need can cause dangerous low blood sugar. That’s why your doctor should review your meds every time you reduce your steroid dose.
Don’t assume your sugar will drop on its own. Keep checking. If your fasting glucose stays below 100 mg/dL for two days after stopping steroids, you can probably stop treatment. But always confirm with your doctor. Some people, especially those with risk factors, may develop permanent type 2 diabetes after a steroid course. That’s why follow-up testing at 3 months is recommended.
What’s new in managing this condition?
There’s progress. The European Association for the Study of Diabetes launched a mobile app called STEROID-Glucose in 2023. It lets you enter your steroid dose and blood sugar readings, then recommends insulin adjustments in real time. In pilot studies, users had 32% fewer high blood sugar episodes.
Researchers are also working on new steroids that don’t wreck your metabolism. Compound XG-201, a tissue-selective glucocorticoid, showed a 65% reduction in hyperglycemia compared to prednisone in phase II trials-while still fighting inflammation just as well.
And the problem is growing. Steroids are now used in 75-85% of CAR-T cell cancer therapies, a fast-growing treatment. That means more patients than ever are at risk. By 2030, experts predict steroid-induced diabetes will become the third most common cause of secondary diabetes, after Cushing’s syndrome and pancreatic disease.
What you can do now
If you’re starting steroids:
- Ask for a baseline blood sugar test before you begin.
- Request a monitoring plan-how often, when, and what numbers matter.
- Know your steroid dose and how long you’ll be on it.
- Track your thirst, urination, and energy levels. Don’t brush off fatigue as “just the meds.”
- Don’t skip follow-ups. Even if you feel fine, sugar can rise quietly.
If you’re already on steroids and your sugar is high:
- Insulin is safe and effective. Don’t be afraid of it.
- Work with your doctor to adjust doses as your steroid dose changes.
- Don’t stop insulin or pills on your own when you stop steroids. Get professional guidance.
This isn’t just about controlling sugar. It’s about preventing emergencies. Steroid-induced hyperglycemia can lead to hyperosmolar hyperglycemic state (HHS), which kills 15-20% of people who get it. Or diabetic ketoacidosis. Both are life-threatening. But they’re preventable-with awareness, monitoring, and the right treatment.
Can corticosteroids cause diabetes in people who’ve never had it before?
Yes. Corticosteroids like prednisone and dexamethasone can cause steroid-induced diabetes in people with no prior history. This happens in 10-50% of patients depending on dose and duration. It’s not a permanent condition in most cases, but it requires immediate management to avoid serious complications.
How long does steroid-induced high blood sugar last?
Once you stop taking corticosteroids, blood sugar levels usually return to normal within 3 to 5 days. The liver stops overproducing glucose, insulin sensitivity improves, and the pancreas resumes normal function. However, some people with risk factors may develop lasting type 2 diabetes, so follow-up testing at 3 months is recommended.
Is insulin safe to use while on steroids?
Yes, insulin is the preferred treatment for steroid-induced hyperglycemia. It works directly on blood sugar without relying on your pancreas, which is suppressed by steroids. Basal insulin controls liver glucose output, and rapid-acting insulin covers meals. Insulin doses can be adjusted as steroid doses change, making it flexible and safe.
Should I stop taking my steroids if my blood sugar goes up?
No. Never stop steroids on your own. They’re often prescribed for life-threatening conditions like severe asthma, autoimmune disease, or cancer treatment. Stopping suddenly can cause adrenal crisis. Instead, contact your doctor. They can adjust your diabetes treatment while you continue your steroid therapy safely.
Do all corticosteroids raise blood sugar the same way?
No. Dexamethasone is about 6-8 times more potent than prednisone at causing hyperglycemia at equivalent anti-inflammatory doses. Longer-acting steroids like dexamethasone (36-72 hours) cause prolonged high blood sugar, while prednisone (12-36 hours) has a shorter window. The duration and potency affect how you monitor and treat it.
Can I manage steroid-induced diabetes with diet and exercise alone?
For mild cases, diet and movement help-but they’re rarely enough. Steroids override normal metabolic control. Even strict low-carb diets can’t fully counteract the liver’s increased glucose production or the insulin resistance caused by steroids. Most people need medication, usually insulin, to keep blood sugar in a safe range.
What should I do if I’m on long-term steroids?
If you’re on steroids for months or years, you need ongoing blood sugar monitoring-every 1-3 months. Ask for an HbA1c test every 3 months to track long-term control. Work with your doctor to adjust your diabetes treatment as your steroid dose changes. Some people on long-term steroids develop permanent type 2 diabetes and will need lifelong management.