Every year, millions of people in the U.S. switch from brand-name medications to generics to save money. But many still hesitate-not because of cost, but because they don’t trust them. Generic drugs are not cheaper because they’re weaker. They’re cheaper because they don’t carry the marketing costs of a big-name brand. Yet, confusion persists. Why? Because the language used to explain them is often written for doctors, not patients.
What Exactly Is a Generic Drug?
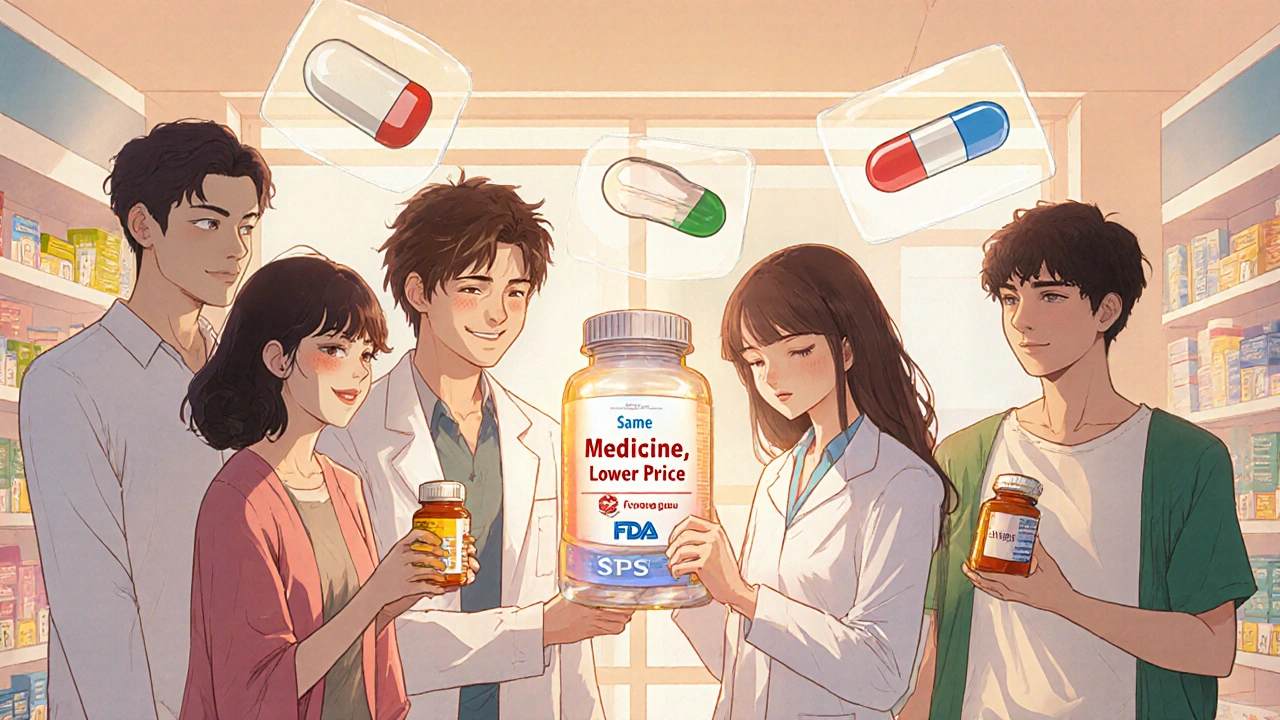
A generic drug is the exact same medicine as the brand-name version, just without the flashy packaging or trademarked name. The FDA requires that generics contain the same active ingredient, in the same strength, and work the same way in your body. If you take 20 mg of esomeprazole (the generic for Nexium), it does the same thing as 20 mg of Nexium. Same chemistry. Same effect. Same safety profile. The only differences? Color, shape, or the inactive ingredients-like fillers or dyes. These don’t affect how the drug works. Think of it like buying store-brand cereal instead of Kellogg’s. Same oats, same sugar, same nutrition. Just a different box. In 2022, 90.9% of all prescriptions filled in the U.S. were for generic drugs. That’s over 6 billion prescriptions. And yet, nearly 4 out of 10 Americans still think generics are less effective. That’s not based on science. It’s based on misunderstanding.Why Do People Doubt Generics?
The biggest myth? That generics aren’t held to the same standards. They are. The FDA doesn’t approve a generic unless it proves it delivers the same amount of medicine into your bloodstream as the brand. The rule? Between 80% and 125% of the brand’s blood concentration. That’s not a wide range-it’s a tight, scientifically proven window. But here’s where things get messy. Some people notice subtle differences. Maybe their headache relief feels slower. Or their thyroid medication doesn’t seem to work as well. These aren’t always imagined. For certain drugs-like warfarin, levothyroxine, or phenytoin-tiny changes in how the body absorbs the drug can matter. These are called narrow therapeutic index drugs. For these, even small variations can cause problems. That’s why experts don’t say all generics are identical. They say they’re bioequivalent. And that’s different. Bioequivalent means they work the same for most people. But for a small group, consistency matters. That’s why your doctor might recommend sticking with one brand of levothyroxine-even if it’s generic-because switching between manufacturers can sometimes cause fluctuations.How Language Guides Fix the Problem
The solution isn’t more pamphlets. It’s better language. That’s where consumer language guides come in. These aren’t legal documents or scientific papers. They’re plain-English tools designed for people who don’t have a medical degree. Take the FDA’s Generic Drug Facts page. It doesn’t say “bioequivalence.” It says: “Generics must work the same as brand-name drugs to get FDA approval.” It uses analogies: “Tylenol is to acetaminophen as Kleenex is to tissues.” It shows side-by-side images of pill bottles. It even explains why generics look different: “The shape and color don’t change how the medicine works.” A 2021 study found that patients who read these simplified guides understood generic drugs 37% better than those who got standard medication leaflets. And it wasn’t just comprehension-it changed behavior. When patients understood the science, they were 22% more likely to stick with their generic prescription. Pharmacies like CVS, Walgreens, and Walmart now train their staff to use a 90-second script: “Same active ingredient. Same effect. Same safety. Just cheaper.” That’s it. No jargon. No fluff.
What’s Missing From Most Guides?
Not all guides are created equal. Some pharmacy chains use generic templates with vague language like “generics are just as good.” That’s not enough. Patients need nuance. For example, most guides don’t mention authorized generics. These are brand-name drugs sold under a generic label-same factory, same formula, same packaging, just no brand name on the bottle. They’re often cheaper than the brand but identical in every way. And studies show patients who switch to authorized generics are 28% less likely to go back to the brand. Also missing? Clear warnings for high-risk drugs. If you’re on levothyroxine, you need to know: “Stick with one manufacturer.” If you’re on phenytoin, you need to know: “If you feel more seizures, tell your doctor right away.” These aren’t edge cases. They’re real risks that need clear, specific guidance. The FDA’s 2023 initiative is starting to fix this. They’re now creating medication-specific guides for drugs like warfarin, digoxin, and cyclosporine. These aren’t one-size-fits-all. They’re tailored. And they’re long overdue.What Patients Are Saying
On Reddit’s r/pharmacy, users shared stories. One woman switched from brand-name Lipitor to atorvastatin and saved $300 a month. She felt the same. No side effects. No difference. Another man switched his thyroid med and noticed his energy dropped. He went back to his original brand-and felt better. His doctor didn’t know why. Turns out, he’d switched manufacturers twice in six months. That’s the problem. No one told him to stay consistent. A 2021 University of Michigan study tracked 450 people on generic levothyroxine. Forty-one percent stopped taking it within six months because they thought it wasn’t working. But when researchers checked their labs, most were within normal range. The issue wasn’t the drug. It was the fear. That’s why the best guides don’t just inform-they reassure. They say: “It’s normal to feel unsure. Here’s what science says. Here’s when to call your doctor.”
What’s Changing in 2025?
By January 2025, all Medicare Part D plans must give patients generic education materials that meet NIH health literacy standards. That means no more 12-point font, no more passive voice, no more “should be taken.” It’s now: “Take this pill every morning.” Pharmacy benefit managers like CVS Caremark and OptumRx are adopting the FDA’s template. AI tools are being tested at Kaiser Permanente to personalize explanations based on your literacy level and medication history. By 2026, your electronic health record might pop up a simple message when your doctor prescribes a generic: “This is the same as the brand, but costs $40 less. Want to see how it works?” The goal isn’t to push generics. It’s to give people the truth so they can choose.What You Can Do Today
If you’re on a generic drug and you’re unsure:- Ask your pharmacist: “Is this the same as the brand?” They’ll show you the FDA-approved facts.
- Check the FDA’s Generic Drugs webpage. It’s updated quarterly and free.
- For thyroid, seizure, or blood thinner meds, ask: “Should I stick with one brand?”
- Don’t switch manufacturers unless your doctor says it’s safe.
- If you feel different after switching, write it down. Bring it to your next visit.
Are generic drugs really as effective as brand-name drugs?
Yes, for most medications. The FDA requires generics to have the same active ingredient, strength, and dosage form as the brand. They must deliver the same amount of medicine into your bloodstream-within 80% to 125% of the brand’s level. This is called bioequivalence. Over 98% of approved generics meet this standard. For most people, generics work just as well.
Why do generic pills look different from brand-name pills?
By law, generic drugs can’t look exactly like the brand-name version. That’s to avoid trademark infringement. So they may be a different color, shape, or size. But those changes only affect appearance, not how the drug works. The active ingredient-and how your body absorbs it-is identical. Think of it like buying a different brand of aspirin: different logo, same pain relief.
Can switching between generic manufacturers cause problems?
For most drugs, no. But for medications with a narrow therapeutic index-like levothyroxine, warfarin, or phenytoin-even small changes in how the body absorbs the drug can matter. If you’re on one of these, it’s safest to stick with the same manufacturer. Talk to your doctor or pharmacist about whether you should avoid switching.
What’s an authorized generic?
An authorized generic is the exact same drug as the brand-name version, made by the same company, in the same factory-but sold without the brand name. It’s not a copy. It’s the real thing, just cheaper. These have the lowest switch-back rates because they’re identical in every way, including inactive ingredients.
Why do some people say their generic medication doesn’t work?
Sometimes, it’s the placebo effect-or a change in manufacturer. Other times, it’s a real issue with a narrow therapeutic index drug. If you feel different after switching, track your symptoms and talk to your doctor. Don’t assume the drug failed. But don’t ignore your body either. The key is consistency: if your medication works, stick with the same version.







Dana Dolan November 19, 2025
i switched from brand-name lisinopril to the generic last year and honestly? zero difference. saved me like $50 a month. my blood pressure’s stable, no dizziness, no weird side effects. why do people still think generics are ‘weaker’? it’s not magic, it’s chemistry.
Codie Wagers November 21, 2025
Let’s be real-this whole ‘generic equals safe’ narrative is corporate propaganda dressed up as public health. The FDA’s bioequivalence window? 80%-125%? That’s not precision-that’s a damn lottery. If your drug is supposed to be 100% effective and you get 82%, you’re getting less than what was prescribed. That’s not science. That’s negligence wrapped in a white coat.
And don’t get me started on ‘authorized generics.’ If it’s the same factory, same formula, why isn’t it branded? Because they want you to think you’re getting a bargain when you’re just paying less for the exact same thing. Sneaky.
People who say ‘it works fine’ are either lucky or delusional. I’ve seen patients crash because their thyroid med switched manufacturers. No one warned them. No one cared. The system doesn’t care about your health-it cares about margins.
Paige Lund November 22, 2025
so… generics are just as good… unless they’re not. got it. thanks for the 3000-word essay on how to feel confused about your medicine.
Michael Salmon November 22, 2025
Wow. Another feel-good article from Big Pharma’s PR department. Let me guess-next you’ll tell us that ‘generic’ means ‘same quality’ and ‘no risk.’ Please. The FDA approves generics based on averages, not individual biology. You think your body responds like a lab rat? Nah. You’re a human. And humans don’t fit into 80%-125% windows. That’s not medicine. That’s statistics pretending to be care.
And don’t even get me started on the ‘90-second script’ pharmacies use. ‘Same active ingredient. Same effect.’ Bullshit. My cousin’s heart rate went nuts after switching generics. The pharmacist didn’t even blink. Just handed her the bottle and said ‘it’s fine.’
This isn’t about education. It’s about pushing cost-cutting onto patients while pretending it’s empowerment. You’re not giving people truth-you’re giving them a sales pitch with a stethoscope.
Joe Durham November 23, 2025
I get where the skeptics are coming from-I really do. I’ve been on levothyroxine for 12 years, and I’ve switched manufacturers three times. Twice, I felt off: fatigue, brain fog, mood swings. The third time, I asked my doctor to lock me into one brand. That’s when things stabilized.
It’s not that generics are bad. It’s that the system treats them like interchangeable widgets. But for some meds, they’re not. The language guides help, but they need to be louder about the exceptions. Not every drug is like ibuprofen. Some of us are one switch away from a crisis.
Also, authorized generics? I had no idea those existed until last year. That’s the kind of info that should be front and center, not buried in a footnote. If you’re gonna save people money, at least give them the full picture.
Nick Lesieur November 24, 2025
lol so now we’re supposed to trust a pill because it’s ‘bioequivalent’? next they’ll say ‘your phone charger is bioequivalent’ so it’s fine to use a $3 knockoff. same voltage, right? sure. until your phone explodes.
also, ‘stick with one manufacturer’? yeah right. my pharmacy switches it every other refill. no warning. no consent. just a different color pill. and if i complain? they say ‘it’s the same.’ well, it’s not the same to me. my body knows.
Angela Gutschwager November 26, 2025
my thyroid med switched again. i felt like a zombie for 3 weeks. pharmacist didn’t care. just said ‘it’s the same.’ nope. not for me. 😔
Andy Feltus November 28, 2025
Here’s the real question: why do we let corporations decide how we experience our own bodies? The system doesn’t care if you feel worse after a switch-it cares if the pill passes a lab test. But you’re not a lab. You’re a person who wakes up tired, who feels anxious, who wonders if the pill in your hand is really the same one that kept you alive last month.
Language guides help. But they’re still just words. What we need is a system that respects individual biology-not one that treats people like variables in a cost-benefit equation.
And honestly? The fact that we even have to argue this in 2025 is a failure. Not of science. Of ethics.
Dion Hetemi November 29, 2025
Let’s cut the crap. The FDA doesn’t test generics on real people. They test them in a flask. You think your body reacts the same as a beaker? Newsflash: your gut microbiome, your liver enzymes, your stress levels-they all affect how you absorb meds. But the system? It doesn’t care. It just wants to cut costs and check a box.
I’ve been on warfarin for 8 years. I’ve switched generics twice. Both times, my INR went wild. I ended up in the ER. The doctor said ‘it’s bioequivalent.’ I said ‘I’m not a statistic.’ He shrugged.
So yeah, 90% of people are fine. But what about the 10% who get screwed? We’re not ‘edge cases.’ We’re patients. And we deserve better than a pamphlet that says ‘it’s fine.’
Kara Binning December 1, 2025
AMERICA IS BEING POISONED BY CHEAP DRUGS AND CORPORATE GREED. THIS ISN’T HEALTHCARE-IT’S A SCAM. THE FDA IS A BRIDGE FOR PHARMA TO STEAL OUR MONEY AND OUR HEALTH. GENERICS ARE A LIE. I SAW MY NEIGHBOR DIE BECAUSE HER THYROID MED WAS SWITCHED. SHE WAS TOLD IT WAS ‘THE SAME.’ IT WASN’T. IT WAS A KILLER.
WE NEED TO BAN THIS. WE NEED TO FIGHT. WE NEED TO STOP LETTING BIG PHARMA CONTROL OUR LIVES WITH A $4 PILL AND A LAUGHABLE ‘FACTS’ PAGE.
river weiss December 3, 2025
Thank you for writing this with such clarity. The FDA’s Generic Drug Facts page is one of the few public health resources that actually gets it right: simple, factual, and human-centered. But it’s not enough. We need this level of communication embedded in every pharmacy interaction, every EHR prompt, every insurance form.
For patients on narrow therapeutic index drugs-especially levothyroxine, warfarin, or phenytoin-the stakes are life-or-death. Consistency isn’t a preference; it’s a medical necessity. And yet, most patients are never told this unless they ask.
The authorized generic point is critical. Many people don’t realize they’re already taking the brand’s exact product-just without the logo. That’s not a compromise. That’s a win. And we need to shout it from the rooftops.
Also, thank you for emphasizing: if you feel different after a switch, document it. Bring it to your provider. Your symptoms are data. They’re not ‘in your head.’ They’re your body speaking. And we need to listen.
This isn’t just about pills. It’s about dignity. About trust. About treating people like partners in their care-not passive recipients of corporate cost-saving measures.
Brian Rono December 3, 2025
Let’s be brutally honest-this whole ‘generic = good’ crusade is a smokescreen. The FDA’s 80%-125% window? That’s not science. That’s a corporate loophole dressed up as regulation. You’re not getting ‘the same drug.’ You’re getting a drug that’s statistically similar enough to pass a bureaucratic audit.
And don’t even get me started on the ‘90-second script.’ ‘Same active ingredient. Same effect.’ Yeah, right. Like saying ‘a Ferrari and a Yugo both have four wheels and an engine.’ Technically true. Practically? You’re gonna have a bad day if you think they’re the same.
People who say ‘it works fine’ are either blissfully ignorant or they’ve never had a real crisis. I’ve seen people on phenytoin have seizures after a manufacturer switch. The pharmacy didn’t even blink. Just said ‘it’s bioequivalent.’ Bioequivalent? My friend’s brain was on fire.
And authorized generics? That’s the only thing that makes sense. Same factory. Same formula. Same everything. Why isn’t that the default? Because the system wants you to think you’re saving money when you’re actually being played.
This isn’t about education. It’s about exposure. The public needs to know: this isn’t healthcare. It’s a profit-driven gamble with your life. And the people who designed this system? They’re not in the hospital. They’re in boardrooms, sipping espresso, counting the pennies they saved on your pills.