Putting together multiple sedating medications might seem like a simple fix for insomnia, anxiety, or chronic pain-but it’s one of the most dangerous things people do without realizing it. You’re not alone if you’ve taken a sleep pill at night, a muscle relaxer during the day, and an opioid for back pain, thinking each one is fine on its own. The problem isn’t the individual drugs. It’s what happens when they stack up. Together, they don’t just add up-they multiply. And that multiplication can stop your breathing, send you into a coma, or kill you without warning.
Why Mixing Sedatives Is Like Playing Russian Roulette
Sedating medications work by slowing down your brain. They boost a chemical called GABA, which tells your nervous system to calm down. That’s why drugs like benzodiazepines (Xanax, Valium), sleep aids (Ambien, Lunesta), opioids (oxycodone, hydrocodone), and even alcohol make you feel relaxed or drowsy. But when you take two or more of these at the same time, they don’t just work side by side. They team up. The effect becomes synergistic, meaning the whole is far worse than the sum of its parts. For example, an opioid alone can slow your breathing. A benzodiazepine alone can make you groggy. But together? A 2017 study in JAMA Internal Medicine found people taking both had more than double the risk of overdose compared to those taking opioids alone. The numbers don’t lie: in 2020, about 1 in 6 opioid-related overdose deaths in the U.S. also involved a benzodiazepine. That’s not coincidence. That’s a direct, deadly interaction. And it’s not just prescription drugs. Alcohol is the most common-and most dangerous-mixer. Just two drinks with a sleep medication like zolpidem can cut your reaction time by 70%. That’s worse than being legally drunk. People don’t realize that a glass of wine with their nighttime painkiller is just as risky as mixing vodka with Xanax.The Deadliest Combinations You Might Be Taking
Some combinations are more lethal than others. Here are the top three you need to watch out for:- Opioids + Benzodiazepines: This is the most deadly pair. It directly shuts down your brain’s breathing control center. UCLA Health estimates this combination causes nearly 30% of all prescription drug deaths. Even if you’ve taken each drug safely for years, adding the other one can be fatal.
- Alcohol + Any Sedative: Alcohol is a CNS depressant too. Mixing it with sleep aids, anti-anxiety meds, or painkillers increases overdose risk by 4 to 5 times. People don’t think of alcohol as a drug-but it’s one of the most potent ones when combined.
- SSRIs + MAOIs: These are antidepressants. When taken together, they can trigger serotonin syndrome-a rare but life-threatening condition where your body overheats, your muscles spasm, and your heart races. Symptoms can show up within hours. About 14-16% of cases end in death if not treated fast.
Warning Signs: When to Call 999 Immediately
You don’t need to wait for a full-blown overdose to act. These signs mean your body is shutting down-and you need help now:- Slowed or shallow breathing (fewer than 12 breaths per minute)
- Blue lips or fingertips (sign of low oxygen)
- Unresponsiveness-even loud shouting won’t wake you up
- Gurgling or snoring sounds while sleeping (a sign of airway blockage)
- Extreme confusion, dizziness, or inability to stand
Who’s at Highest Risk-and Why
Older adults are the most vulnerable. As we age, our bodies process drugs slower. Liver and kidney function decline. That means even normal doses can build up. The American Geriatrics Society’s Beers Criteria lists 19 sedating drug combinations that older adults should avoid. One in three seniors still takes at least one of them. But it’s not just age. People with chronic pain, anxiety, or insomnia are often prescribed multiple sedatives over time. They’re told each one is safe alone. No one warns them about the combo. A 2020 study found that electronic health records flagged only 17% of dangerous drug pairs. Doctors aren’t always alerted. Patients aren’t told. And then there’s the hidden problem: doctor shopping. Recovery Village found that 42% of people who overdosed on combined sedatives had gotten prescriptions from three or more doctors in six months. They weren’t trying to get high-they were trying to manage symptoms. But no single doctor had the full picture.
What You Can Do Right Now
You don’t have to wait for a crisis. Here’s how to protect yourself:- Make a complete list of everything you take: prescriptions, over-the-counter meds (like diphenhydramine in sleep aids), supplements (like melatonin or valerian root), and alcohol. Bring this to every appointment.
- Ask your doctor: “Am I taking any drugs that could dangerously interact?” Don’t assume they know. Most don’t.
- Know your opioid dose in morphine milligram equivalents (MME). If you’re on more than 50 MME per day and also taking a benzodiazepine, your risk skyrockets. Ask for a dose review.
- Never mix alcohol with sedatives. Not even a glass of wine. Not even one night.
- Get a medication review every three months if you’re over 65 or taking three or more sedating drugs. The START criteria say this is non-negotiable.
What’s Being Done-and What’s Still Broken
There’s been progress. Since 2016, the FDA has required black box warnings on all opioid and benzodiazepine labels. All 50 states now require electronic prescribing for controlled substances, which helps track dangerous combos. The CDC now explicitly says: avoid prescribing opioids and benzodiazepines together unless absolutely necessary. But gaps remain. Only 28% of primary care doctors regularly screen for these interactions. Many patients can’t afford non-sedating alternatives-like gabapentin for nerve pain or CBT for insomnia-because they cost $450-$600 a month, while sedatives are $15-$30. Insurance doesn’t always cover safer options. New tools are emerging. The FDA-approved DETERMINE platform uses AI to predict individual risk for sedative interactions with 87% accuracy. And the NIH is investing $127 million to study genetic testing that could tell you, before you even take a drug, whether your body is likely to overreact to it. But those tools won’t help if you don’t know to ask for them.It’s Not Always About Abuse
Some people assume these deaths only happen with recreational drug use. They’re wrong. Most victims are people trying to manage real health problems. A 2022 Healthline survey found 18% of patients on carefully monitored low-dose combinations reported better quality of life. But that’s under strict medical supervision-with weekly check-ins, clear dosing rules, and no alcohol. The difference between safety and disaster isn’t intent. It’s awareness. It’s communication. It’s asking the right questions.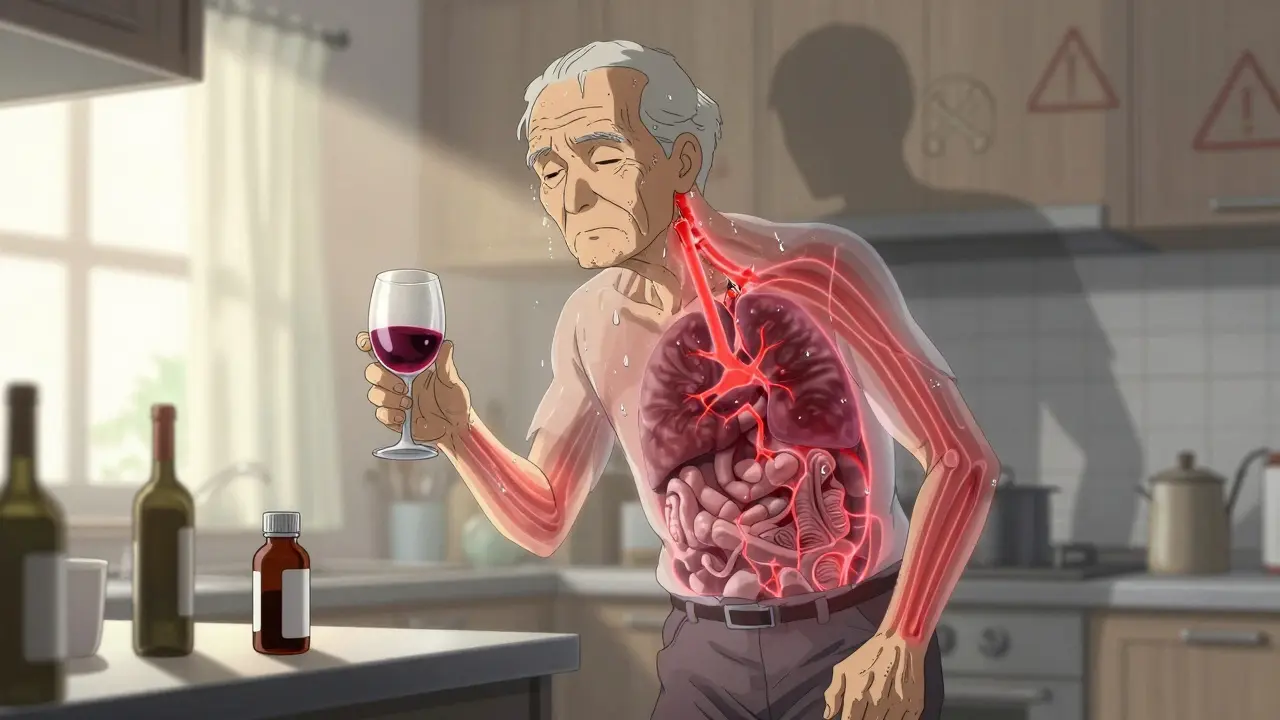
What to Do If You’ve Already Mixed Them
If you’re currently taking multiple sedatives together, don’t panic. Don’t quit cold turkey-that can be dangerous too. But do this:- Schedule an appointment with your doctor or pharmacist. Bring your full medication list.
- Ask: “Which of these can I stop first? Which is the most risky in combination?”
- Never stop an opioid or benzodiazepine suddenly. Withdrawal can cause seizures or rebound anxiety.
- Ask about a slow taper plan-usually 10-25% reduction every 1-2 weeks.
- Ask if there’s a non-sedating alternative. For sleep: cognitive behavioral therapy for insomnia (CBT-I). For anxiety: SSRIs without benzos. For pain: physical therapy or nerve blocks.
Final Thought: You’re Not Alone, But You Don’t Have to Risk It
Millions of people are taking dangerous combinations without knowing it. You’re not careless for doing it. You’re just following what you were told. But now you know better. And knowledge is the first step to safety. The goal isn’t to scare you. It’s to give you power. You have the right to ask questions. You have the right to demand a safer plan. And you have the right to live without the shadow of an accidental overdose hanging over every pill you take.Can I safely take two sedating medications if my doctor prescribed them?
Just because a doctor prescribed both doesn’t mean it’s safe. Many doctors aren’t aware of the full interaction risks, especially if the prescriptions came from different specialists. Always ask: ‘Are these two drugs known to interact dangerously?’ If you’re on opioids and benzodiazepines together, your risk of overdose is more than double. Ask for a full medication review and whether a non-sedating alternative exists.
What should I do if I accidentally mixed alcohol with my sleep medicine?
If you’ve taken alcohol with a sedative like Ambien or zolpidem, stay awake and monitor yourself closely for at least 6-8 hours. Watch for slow breathing, confusion, or dizziness. If you feel unusually drowsy or can’t stay alert, call emergency services immediately. Do not try to sleep it off. Alcohol and sleep meds together can cause your breathing to stop while you’re unconscious.
Are over-the-counter sleep aids like melatonin or diphenhydramine safe to combine with prescription sedatives?
No. Even ‘natural’ supplements like melatonin or OTC sleep aids like diphenhydramine (Benadryl) can slow your breathing and increase sedation. Melatonin itself is low-risk, but when combined with benzodiazepines or opioids, it adds to the total CNS depression. Diphenhydramine is a strong anticholinergic and sedative-it’s just as dangerous as prescription sleep pills when mixed. Always include OTC meds and supplements on your medication list.
How long should I wait between stopping one sedative and starting another?
It depends on the drugs. For switching from an SSRI to an MAOI, you must wait at least 14 days to avoid serotonin syndrome. For opioids and benzodiazepines, there’s no fixed rule, but a 24-48 hour gap is often recommended if you’re switching or tapering. Always follow your doctor’s guidance. Never assume waiting a day is enough-some drugs stay in your system for days or weeks.
Can I use CBD oil instead of benzodiazepines to avoid dangerous interactions?
CBD oil is not a proven replacement for benzodiazepines. While some people report reduced anxiety with CBD, it’s not regulated, and studies on its effectiveness for anxiety are mixed. More importantly, CBD can interact with liver enzymes that break down many sedatives, potentially increasing their levels in your blood. That means even if you stop the benzodiazepine, adding CBD could still make other drugs more potent. Don’t assume it’s safer without medical advice.
What are the long-term effects of combining sedating medications?
Long-term use of multiple sedatives leads to tolerance, meaning you need higher doses for the same effect. This increases overdose risk. It also causes cognitive decline-memory loss, confusion, slower thinking. In older adults, it raises fall risk by 50%, leading to broken hips and long-term disability. There’s also evidence linking chronic polypharmacy to higher dementia rates. The damage isn’t always immediate, but it’s real and cumulative.






john Mccoskey January 18, 2026
Let’s be real-this isn’t about education, it’s about systemic failure. Doctors prescribe like they’re playing Tetris with your nervous system. They don’t care about synergy, they care about ticking boxes. You get anxiety? Here’s Xanax. Can’t sleep? Here’s Ambien. Back hurting? Take oxycodone. No one connects the dots because the system rewards volume, not vigilance. And when you die? It’s labeled an ‘accident.’ Not negligence. Not malpractice. Just bad luck. We’ve turned medicine into a vending machine and people into coins. The real crisis isn’t the drugs-it’s the indifference that lets this keep happening.
vivek kumar January 18, 2026
The data is unequivocal: synergistic CNS depression is a leading cause of preventable death. Yet, medical education still treats polypharmacy as an edge case rather than an epidemic. The FDA black box warnings are a start, but without mandatory EHR alerts for high-risk combinations, we’re rearranging deck chairs on the Titanic. Furthermore, the assumption that ‘prescribed = safe’ is dangerously naive. Pharmacists must be empowered to intervene-not just flag, but halt. This isn’t theoretical. I’ve seen three patients in my clinic alone die from this exact scenario. Knowledge without action is complicity.
Riya Katyal January 19, 2026
Oh wow, so taking two things that make you sleepy is bad? Who knew? Next you’ll tell me drinking gasoline is bad for your kidneys. I mean, I get it, you’re trying to sound smart-but this post reads like a textbook that got lost in a support group. Maybe stop writing like you’re giving a TED Talk and start writing like someone who’s actually lived through this?
Henry Ip January 19, 2026
Thank you for this. I’ve been scared to say anything because everyone says ‘just take what your doctor gives you’ but I’ve been on three sedatives and alcohol on weekends and I didn’t realize how close I was to not waking up. I just cut out the wine and made an appointment. Small steps. You’re not alone. We’re all just trying to survive.
waneta rozwan January 20, 2026
MY BROTHER DIED FROM THIS. He was 42. Took Xanax for anxiety, oxycodone for a work injury, and had a glass of wine every night ‘to relax.’ He didn’t even know it was a problem. His doctor never asked. His pharmacist never warned. He just… stopped breathing one night. And now I’m here screaming into the void because no one listens until it’s too late. This isn’t a ‘warning.’ It’s a funeral notice written in prescription bottles.
Nicholas Gabriel January 20, 2026
Can we talk about the fact that this entire post is written in perfect, clinically accurate language-but the people who need to read it the most? They’re the ones scrolling past it because it’s ‘too long’ or ‘too scary’? We need infographics. We need TikTok videos. We need memes that say ‘Your wine + Ambien = your funeral’ in Comic Sans. People don’t read 2000-word essays. They react to visuals. We’re in 2024. Why are we still relying on PDFs and doctor’s office pamphlets?
Cheryl Griffith January 21, 2026
I’ve been on a low dose of gabapentin and trazodone for years. My doctor said they were fine together. But I started feeling foggy, like my brain was wrapped in cotton. I didn’t realize it was the combo until I read this. I cut out the trazodone cold turkey-big mistake. Had panic attacks for a week. Now I’m tapering slowly, under supervision. The scariest part? No one ever told me to monitor my own symptoms. We’re taught to trust, not to observe. This post saved my life. Thank you.
swarnima singh January 22, 2026
so like... if i take melatonin and klonopin and a glass of wine... is that like... bad? or is it just me being dramatic? like i know its not good but i feel so much better at night and i dont wanna stop... also my mom says i'm addicted but shes just mad i dont go to church
Isabella Reid January 23, 2026
As someone who grew up in a culture where ‘medication = weakness,’ I didn’t even tell my doctor I was taking valerian root and sleeping pills together. I thought if I just ‘tried harder’ to sleep, I wouldn’t need the meds. Turns out, my body was screaming. Now I’m in therapy, on a slow taper, and I finally feel like I’m not just surviving. This isn’t about being strong. It’s about being smart. And yeah, asking for help is the bravest thing you can do.
Kasey Summerer January 23, 2026
lol at the FDA black box warning like that’s gonna stop anyone. I’ve seen people take 4 benzos, 3 opioids, and a bottle of whiskey and still say ‘I’m fine.’ It’s not ignorance. It’s denial. And the people who need this info? They’re too busy scrolling cat videos to read a 10-page essay. We need a ‘Sedative Overdose Simulator’ app. Like a game where you pick your combo and see how fast you die. Maybe then they’d listen.
kanchan tiwari January 24, 2026
THIS IS A GOVERNMENT PLOT. They want you addicted so they can control you. The ‘dangerous combinations’? Made up. The real danger is the pharmaceutical industry. They profit from your fear. They pump out these drugs knowing you’ll stack them. Then they sell you the antidotes. They’re not trying to save you-they’re trying to monetize your collapse. Wake up. They’re watching. They’re listening. They’re in your pills.
Bobbi-Marie Nova January 25, 2026
Okay but honestly? I took a melatonin and a muscle relaxer once and woke up in a puddle of drool on the floor. Felt like I’d been hit by a truck made of fog. I didn’t tell anyone. But now I know why. I’m done. No more ‘just one’ anything. My brain deserves better than being a party for chemicals.
Allen Davidson January 26, 2026
I’m a nurse. I’ve seen this too many times. The saddest part? The patients who survive usually say ‘I didn’t think it would happen to me.’ But it happens to everyone who does it. I wish I could hand every patient a printed version of this post. No jargon. No fluff. Just: ‘This combo kills. Period.’ You don’t need to be an expert to understand that.
Samyak Shertok January 27, 2026
So… what’s the alternative? You’re telling people to stop their meds, but you don’t offer real solutions. CBT-I costs $600? Physical therapy? Not covered. Gabapentin? Still sedating. So what’s left? Suffer? Starve? Sleep in a chair? This isn’t advice-it’s guilt-tripping with footnotes. You want people to change? Fix the system first. Stop blaming the broken for not being perfect.
Stephen Tulloch January 27, 2026
Wow. Just… wow. This is the most articulate, data-rich, emotionally intelligent piece I’ve read on this topic. Honestly, I’m impressed. You didn’t just list risks-you framed it as a moral imperative. And the part about doctor shopping? 100% accurate. I’ve seen it firsthand. This isn’t just a medical post. It’s a manifesto. I’m sharing this with my entire family. And yes, I’ve been taking Ambien + hydrocodone for 8 months. Time to talk to my pharmacist. Thanks for not sugarcoating it.