It’s downright wild how a single pill can flip the script on stubborn infections. Flagyl ER—yep, the extended-release version of trusty metronidazole—has a way of swooping in when typical antibiotics wave the white flag. But it’s not some everyday go-to. Doctors pull it out of the cabinet for pretty specific reasons, and most people taking it haven’t just got the sniffles. We’re talking about things like bacterial vaginosis, certain pelvic infections, and hard-to-treat tummy troubles like amebiasis. Why toss down a slow-release version? Well, it keeps levels steady in your bloodstream so bacteria don’t get a break to regroup. That’s comfort in a capsule for people who’d rather not wake up for a dose in the middle of the night.
What Makes Flagyl ER Different from Regular Antibiotics?
Flagyl ER’s magic trick is sticking around in your body longer. It releases metronidazole slowly, so you’re not stuck timing doses four times a day. Instead, you might need just one or two. It’s especially good for infections that hang out where blood flow is funky—places like the deep pelvis or bits of the digestive tract where other drugs can’t quite reach. The FDA gave the green light for Flagyl ER specifically for bacterial vaginosis (“BV” if you’ve been on the receiving end of an awkward diagnosis), but doctors use it off-label for other nasties that regular antibiotics barely dent.
Now, not all banana instructions work for every fruit salad, and the same thing goes for antibiotics. Flagyl ER won't take out viruses, so don’t expect it to help if you’ve got the flu or a wicked cold. Misusing antibiotics—even strong ones like this—just trains bacteria to play dirty, which doctors everywhere are racing to prevent. In fact, a report by the CDC found that up to 30% of antibiotic prescriptions in the U.S. are unnecessary. That’s millions of pills going down the hatch for no good reason. When bacteria get crafty and outsmart our best antibiotics, everyone loses.
“Patients diagnosed with bacterial vaginosis and prescribed Flagyl ER typically experience relief in symptoms like discharge and odor within 2-3 days, but it’s crucial they finish the entire course to prevent recurrence,” says Dr. Rosalind Morgan, infectious disease specialist at New York Presbyterian Hospital.
“Metronidazole remains a first-line treatment, but misuse can accelerate bacterial resistance. Patients should always clarify exact dosing and potential side effects with their healthcare provider.”
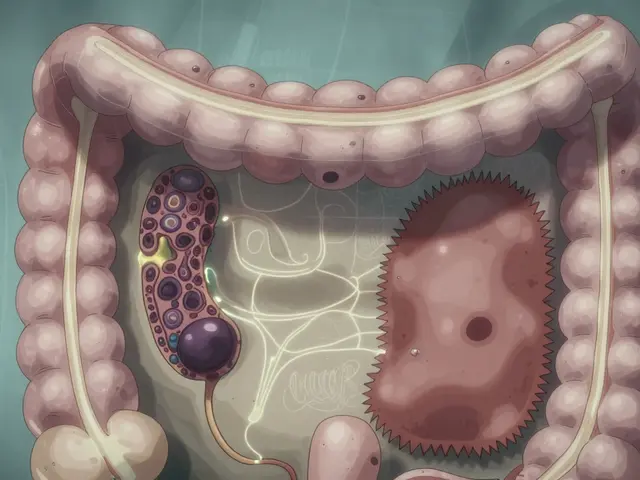
On a molecular level, metronidazole isn’t playing around. It causes knots in the DNA of troublemaker bacteria and protozoa, stopping them from multiplying. It’s especially good at tackling the tough bugs that hide out where oxygen is low—think deep in abscesses or inside the intestines. That’s something many common antibiotics can’t handle. And because Flagyl ER is extended-release, you don’t get those peaks and valleys in your blood levels, which means fewer side effects and less “crash” feeling as the drug wears off.
If you ever peek at a Flagyl ER pill, you’ll notice they’re bigger and a bit different from typical tablets. Don’t cut them in half (even if you want to save money or dose yourself creatively). Splitting destroys the built-in release trick, which can end up dosing you with way too much or way too little all at once. That’s a recipe for both side effects and treatment failure. If you have trouble swallowing big pills, flag this with your doctor. Sometimes, a regular metronidazole or even liquid formula works just as well if taken correctly.
Flagyl ER is usually prescribed for 7 days for BV, but for harder-to-treat infections, the course can be longer. Timing matters, too. Take it with food—unless your doctor says otherwise—to avoid the dreaded upset stomach. A glass of water helps get it all down, and a little planning makes a big difference for folks juggling other meds or meals.

Possible Side Effects and How to Deal With Them
Most people get through a week on Flagyl ER with little more than a weird taste in their mouth and maybe a bit of nausea. Others—especially folks who don’t eat before taking it or gulp it down with just a sip of water—notice a metallic aftertaste that’s hard to shake. Chewing gum or sucking on hard candy sometimes helps. More rarely, there’s serious stuff to watch for. Dizziness, headaches, tummy cramps, and diarrhea can sneak up, especially if you miss doses or mix Flagyl with booze. Study after study (and plenty of nurse warnings) agree: keep alcohol off the guest list while you’re on metronidazole. There’s a reason—the combo can kick off violent vomiting and racing heart, way beyond your average hangover.
Here’s a quirky tidbit: guided by science, the alcohol warning is more than old folklore. Mixing metronidazole and alcohol interferes with how your body breaks down booze, letting a compound called acetaldehyde pile up. This makes you feel sick fast—flushing, pounding head, nausea—sometimes within minutes. One 2020 toxicology review found that about ⅓ of people who ignored this warning had dramatic reactions. No glass of wine is worth that drama! Even foods with hidden booze, like certain sauces or extracts, should be avoided until the last dose has cleared your system, usually after 48 hours.
If you’re the type who reads medication leaflets word-for-word, you’ll spot some extra possible Flagyl ER side effects: rashes, weird changes in your pee color (sometimes darker), and rarely, tingling or numbness in fingers and toes. This last one—called “peripheral neuropathy”—shows up mostly in people taking the drug long-term, like those with chronic gut infections. If you get this symptom, call your doc right away. Sometimes Flagyl needs to be stopped and changed out for something else. Kids and seniors can be more sensitive to these issues, so it’s wise to keep an extra eye out if they’re prescribed this med.
Flagyl ER can also mess with your taste buds during treatment. Some folks complain that every bite of food tastes off, or they get a lingering bitter twinge, especially if they don’t drink enough water. Having a glass of something cold—plain water, seltzer, or a sports drink—on hand can tame that metallic funk, at least for a few minutes. If you have to keep up your appetite, try eating bland or cool foods like yogurt or applesauce to keep nausea at bay. Avoid spicy or greasy meals until you’ve finished your medication.
While most people’s side effects go away a few days after stopping Flagyl ER, very rare reactions like seizures or severe allergic rashes demand emergency care. If you ever have trouble breathing, swelling of your face, or a sudden rash that spreads fast, don’t mess around—head straight to urgent care or call for help.
Pregnant and breastfeeding folks need a special mention. Flagyl can pass into breast milk and across the placenta, but studies say that short courses like those used for BV usually don’t hurt the baby. Still, always talk this through with your OB-GYN before starting, and if you’re breastfeeding, find out whether you need to pump and dump for a while.
It’s helpful to write down your symptoms, both the original infection and anything new that pops up. Your doctor will want to know how you’re feeling from the first dose until the prescription runs out. With busy schedules, it’s easy to forget whether something started before or after a new med. Notes, even if just on your phone, make a huge difference in getting the right care.

Flagyl ER Tips for Real Life and When to Call Your Doctor
Staying organized is half the battle when you’re on a strict medication schedule. Set phone reminders, use a pillbox, or even stick Post-it notes on your fridge. If you miss a dose, don’t double up—just take the next scheduled pill. Doubling up can double the side effects without double the benefit. If you throw up soon after taking a pill and can still see it in the vomit, you probably need another. If not, check with a pharmacist or your doctor before repeating the dose.
Flagyl ER can interact with all kinds of other medicines—blood thinners like warfarin, seizure meds, and certain antidepressants, just to name a few. Always hand over an updated list of what you take, including vitamins and herbal stuff. St. John’s Wort and a few other supplements can mess with how Flagyl works, sometimes making it less effective or increasing side effects. Even simple antacids can slow down absorption if taken too close together. A pharmacist can help with spacing things out if the schedule gets crowded.
If you’re planning to travel while on Flagyl ER, bring extra pills (plus a copy of your prescription, just in case you need to prove what’s in your bag). Extreme heat and humidity—like stashing your meds in the glove box or a steamy bathroom—can make the drug break down faster. Keep it in a cool, dry spot, ideally in its original container with the label slapped on. Never share leftover antibiotics with friends or family, even if their symptoms sound just like yours. The right dose and duration are crucial, and sharing leftover meds is a big reason resistance rates keep ticking up.
Some infections might clear up before the prescription runs out, but don’t get cocky and quit Flagyl ER early. Cutting the course short is like sending your army home one battle too soon—the enemy might regroup and come back even nastier. One patient study showed that people who stopped after just a few days of feeling better had their infections return nearly twice as often as those who stuck it out the whole week.
Certain folks should call their doctor right away if anything feels wrong while taking this drug. Watch for side effects like severe headache, blurry vision, confusion, persistent vomiting, or allergic reactions (hives, breathing trouble, swelling). Don’t wait for things to get worse—flag these symptoms early to avoid bigger problems.
Finally, don’t hesitate to ask a friendly pharmacist any nagging questions. Whether you’re dealing with the aftertaste, worried about missed doses, or curious about what foods go best with your meds, they’ve heard it all. “I tell folks to keep it simple: water, regular meals, and lots of communication if anything changes,” says Karen Lam, lead pharmacist at a Houston urgent care.
“Flagyl ER is a powerful tool, but it works best when patients really partner with their care team and don’t go it alone.”
Flagyl ER might not be famous or trendy, but in its own quiet way, it’s a real lifesaver when standard treatments just can’t cut it. Use it right, listen to your body, and never be shy about reaching out for help. Little victories—a clear mind, a quiet gut, or a healed infection—can add up in a hurry if you keep your eyes open and stay on track.







AJIT SHARMA August 13, 2025
Nice write-up but people always act like pills are magic fix-alls.
Take the med if doc says so, finish the course, and stop whining about a weird taste.
Karen Nirupa August 16, 2025
Thanks for the clear breakdown — this is really helpful for people who get anxious when they see a prescription for something labeled “ER.”
I appreciate the practical tips about food, alcohol, and storing the medication. It might also comfort readers to know that pharmacists are a great, underused resource for dose timing and interactions, especially if someone is on multiple medications.
If anyone here is pregnant or breastfeeding and feeling uncertain, please consult your OB-GYN before starting anything; that shared decision-making really matters.
Thomas Ruzzano August 18, 2025
Good article but I wish it called out overprescribing more bluntly. The line about CDC stats is barely a slap on the wrist — antibiotic misuse is a public-health dumpster fire.
Also, people need to stop self-dosing with leftovers from who-knows-when. That’s how you get resistance and a mess for the rest of us.
Dan Tenaguillo Gil August 20, 2025
I’ll add a longer clinical perspective because this topic comes up a lot in outpatient and hospital settings and there are nuances people often miss.
First, the ER formulation is not just a convenience for dosing; it changes some pharmacokinetics in ways that matter for tissue penetration. For infections that are deep or have limited vascular supply, maintaining a steady plasma concentration can improve the drug’s ability to reach effective levels at the site of infection. That’s why clinicians favor extended-release formulations for certain pelvic or intestinal infections where intermittent peaks and troughs could allow bacteria to persist.
Second, while metronidazole is often discussed in the context of bacterial vaginosis, its activity against anaerobes and protozoa is broader, and that biologic activity explains both its strengths and side effects. The DNA-damaging mechanism that makes it effective also means rapidly dividing human cells in some tissues can transiently feel the impact — hence nausea, metallic taste, and the rare neurotoxic effects.
Third, peripheral neuropathy is rare but real, and clinicians should ask about baseline neuropathic symptoms before prescribing longer courses. If a patient develops paresthesia, taking prompt action to stop the drug can prevent progression. Long-term courses aren’t common for routine BV but do occur for certain refractory or complex infections; those require careful monitoring.
Fourth, interactions matter. Metronidazole inhibits CYP pathways and can potentiate warfarin’s effect, increasing INR — so anyone on anticoagulants needs closer lab follow-up. It also affects the metabolism of some anticonvulsants and can interact with alcohol, producing a disulfiram-like effect; that’s not just folklore but a predictable biochemical interaction with acetaldehyde accumulation.
Fifth, patient adherence is critical. The ER option helps with adherence by reducing dosing frequency, but if a patient is splitting pills or taking them inconsistently, the pharmacologic advantage is lost. Counsel patients explicitly not to crush or halve ER tablets and to report swallowing issues — alternatives do exist, including immediate-release forms or liquid formulations in some settings.
Finally, for anyone managing recurrent BV or chronic anaerobic infections, consider diagnostic follow-up. Microbiologic confirmation, when possible, and re-evaluation of predisposing factors (IUDs, sexual practices, local hygiene products, or underlying conditions) can reduce recurrence rates more than repeated short antibiotic courses alone.
In short: ER formulation is a useful tool, not a panacea. Use it thoughtfully, monitor for neurotoxicity on prolonged courses, beware interactions, and focus on adherence and prevention strategies to avoid repeat prescriptions.
Tiffany Owen-Ray August 23, 2025
Really appreciate that detailed breakdown — you covered the clinical pieces most people miss.
One thing I’d add from a patient-support angle is that side effects like metallic taste and nausea often feel disproportionately upsetting because they affect daily joys like food. Tell patients it’s temporary and offer small coping strategies: cold smoothies, plain yogurt, or short walks after meals can help keep appetite up and nausea down.
Also, encourage folks to voice even mild neuropathic symptoms early instead of waiting. Early recognition usually means a quick medication change and full recovery.
Jill Brock August 25, 2025
I took metronidazole once and nearly died from the taste, it was brutal and I refused to finish the course, worst decision ever but still dramatic.
Ellie Chung August 27, 2025
Yikes, that sounds awful — taste aversion can be surprisingly traumatic.
Maybe next time try cold foods, strong mints before eating, and sipping something fizzy; it helps some people reset their palate fast.
Sophia Simone August 30, 2025
Not convinced the ER formulation is always superior; in many cases immediate-release metronidazole, dosed correctly, provides the same microbial kill with a more predictable safety profile, especially in patients with complex comorbidities who metabolize drugs unpredictably.
High-level marketing for extended-release pills often overlooks individualized pharmacotherapy, and clinicians should weigh age, liver function, polypharmacy, and adherence before reflexively choosing ER.
sourabh kumar September 1, 2025
Sounds okay.
Christian Miller September 3, 2025
Anybody else notice how quickly big pharma pivots a drug into a new formulation and then shoves it down everyone’s throat? There’s always a financial motive lurking behind “convenience” labels.
I’d be curious about the patent timelines on Flagyl ER and whether prescribing rates spiked after the label change. Medicine and market incentives rarely operate independently.
AJIT SHARMA September 5, 2025
Exactly — follow the money. Doctors should be skeptical and patients too.
You don’t need ER just because it’s shiny; if the standard pill works and you can take it, do that.
Thomas Ruzzano September 8, 2025
I hear the skepticism, but the choice between ER and immediate release isn't just marketing theater — it’s a pharmacology question tied to patient behavior.
For folks who are terrible at remembering midday doses, ER can be the difference between cured and chronic. For others, the cost and access issues make immediate-release the better practical pick. It’s not one-size-fits-all, and blanket distrust of pharma won't solve the logistics patients face.
Karen Nirupa September 10, 2025
Agree with the last point — nuance matters.
It’s entirely reasonable to examine incentives, ask about cost, and request immediate-release if that’s more affordable or accessible. Pharmacists often know cheaper generics and equivalent alternatives and can help navigate insurance formularies.
At the end of the day, choosing the right formulation should be a shared decision between patient and clinician that accounts for adherence, side effects, interactions, and cost.