Warfarin-NSAID Bleeding Risk Calculator
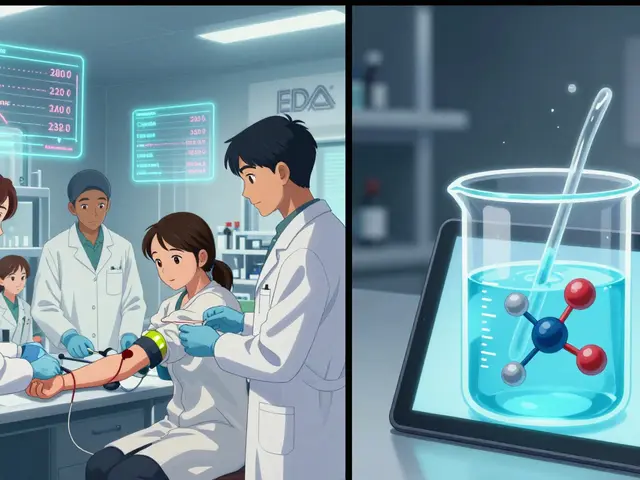
Use this tool to assess your personal bleeding risk when taking Warfarin with NSAIDs. Based on medical research from Aarhus University Hospital and the FDA, this calculator helps you understand the specific dangers based on your situation.
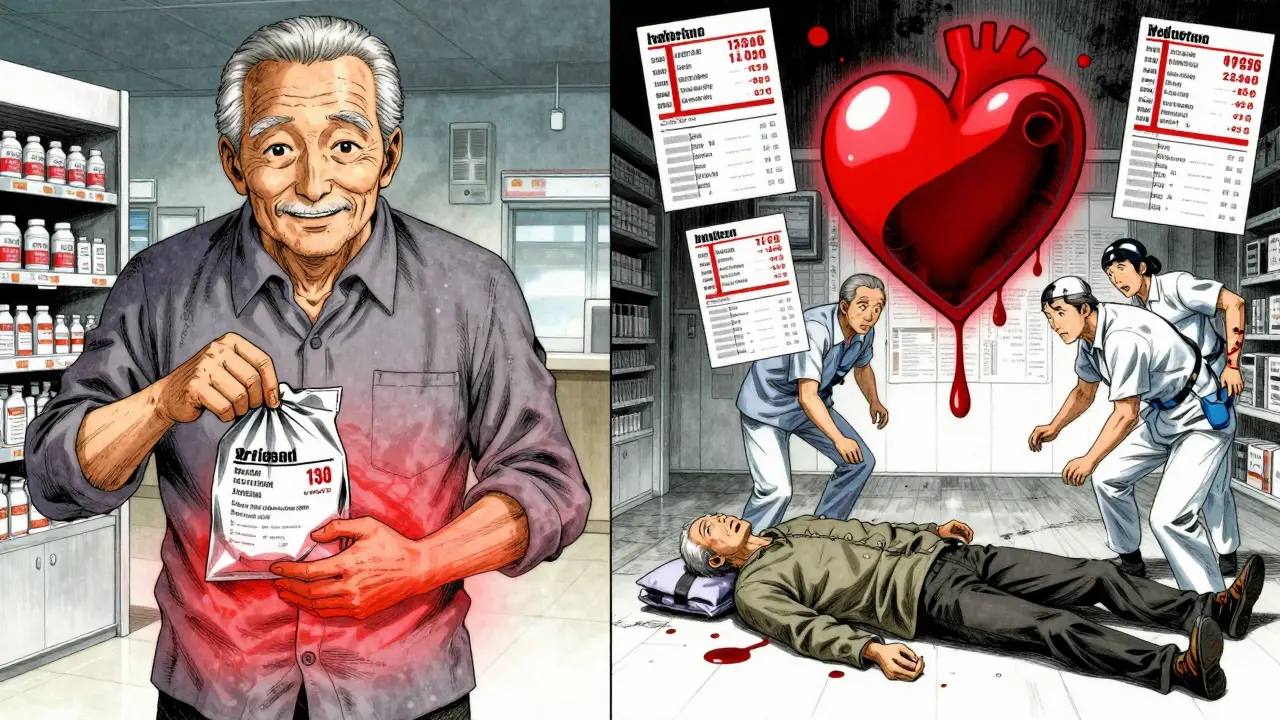
Combining Warfarin and NSAIDs isn’t just a bad idea-it’s a medical hazard that sends thousands to the emergency room every year. If you’re on Warfarin for atrial fibrillation, a replaced heart valve, or deep vein thrombosis, and you reach for ibuprofen or naproxen for a headache or sore knee, you’re playing Russian roulette with your blood. This isn’t theoretical. It’s happening right now to people you know.
Why This Combination Is So Dangerous
Warfarin works by blocking vitamin K, which your body needs to make clotting factors. Without those factors, blood doesn’t clot as easily-good for preventing strokes, bad if you cut yourself or develop an internal bleed. NSAIDs like ibuprofen, naproxen, and diclofenac do two things that make this worse: they stop platelets from sticking together, and they eat away at the stomach lining. Together, they create a perfect storm.
When you take NSAIDs while on Warfarin, your risk of bleeding jumps by more than twice. A 2023 study from Aarhus University Hospital found that people on both drugs had a 2.09-fold higher chance of serious bleeding compared to those on Warfarin alone. That’s not a small increase. That’s a life-threatening one.
Not All NSAIDs Are Created Equal
Some NSAIDs are far riskier than others. Naproxen is the worst offender-users on Warfarin who take it have over four times the risk of bleeding. Diclofenac isn’t much better, at 3.3 times higher. Even ibuprofen, which many think is "safe," still raises the risk by nearly 80%. Meloxicam, often prescribed for arthritis, is also a red flag.
It’s tempting to assume that "selective" NSAIDs like celecoxib (a COX-2 inhibitor) are safer. They’re not. Multiple studies, including one in JAMA Internal Medicine, show they carry the same bleeding risk as traditional NSAIDs when mixed with Warfarin. The stomach lining still breaks down. Platelets still get impaired. The danger doesn’t disappear just because the drug has a different name.
Where the Bleeding Happens
It’s not just your stomach. While gastrointestinal bleeding is the most common-happening 2.24 times more often-it’s not the only concern. Brain bleeds (intracranial hemorrhage) become 3.22 times more likely. Bleeding in the lungs goes up by 36%. Urinary tract bleeding increases by 57%. These aren’t rare side effects. They’re predictable outcomes of this drug combo.
According to the FDA’s adverse event database, over 1,800 bleeding incidents tied to Warfarin and NSAIDs were reported between 2015 and 2020. Sixty-two percent of those were GI bleeds. One Reddit user wrote: "I took ibuprofen for a headache. My hemoglobin dropped from 14 to 8 in 24 hours. I ended up in the ER with a blood transfusion." That’s not an outlier. It’s a pattern.
NOACs Aren’t a Free Pass
You might think switching from Warfarin to a newer anticoagulant like apixaban, rivaroxaban, or dabigatran solves the problem. It doesn’t. While NOACs have fewer drug interactions overall, combining them with NSAIDs still increases bleeding risk.
A 2019 Circulation study found that NSAID use with any oral anticoagulant-whether Warfarin or a NOAC-led to significantly higher rates of major bleeding. The ARISTOTLE trial showed apixaban might be slightly safer than Warfarin in NSAID users, but the risk was still too high to ignore. A 2020 study even found that dabigatran with NSAIDs had less bleeding than Warfarin with NSAIDs-but that doesn’t mean it’s safe. It just means Warfarin is worse.
And here’s the scary part: doctors are prescribing NSAIDs to NOAC patients more than ever. Between 2015 and 2022, NSAID use with NOACs rose by 34.8%. Many patients and even some clinicians believe NOACs are "NSAID-friendly." They’re not.
Who’s at Highest Risk?
Not everyone on Warfarin who takes an NSAID bleeds. But some people are far more vulnerable. Research shows four key risk factors:
- High Warfarin dose (>40 mg per week)
- Taking other medications that interact with Warfarin (like antibiotics or antifungals)
- Low baseline INR (meaning your blood was clotting too well before the NSAID)
- Using meloxicam or naproxen
Age matters too. People over 75 have 3.7 times the risk of bleeding when combining these drugs. That’s not a coincidence. Older adults have thinner stomach linings, slower metabolism, and often take multiple medications. They’re the most likely to end up hospitalized.
What Doctors Should Do
Major medical groups agree: avoid NSAIDs entirely in patients on oral anticoagulants. The American College of Cardiology and American Heart Association give this a Class I recommendation-the strongest possible-saying NSAIDs "should be avoided." If there’s no alternative, here’s the protocol:
- Use the lowest possible dose of the safest NSAID (ibuprofen, if you must).
- Avoid naproxen, diclofenac, and meloxicam completely.
- Check INR before starting the NSAID.
- Check INR again 3 to 5 days after starting, then weekly while taking it.
- Prescribe a proton pump inhibitor (like omeprazole) to protect the stomach.
- Teach the patient exactly what bleeding signs to watch for.
Yet, only 40% of U.S. hospitals have electronic systems that flag this dangerous combo. And 68% of bleeding cases involve patients who never told their doctor they were taking over-the-counter NSAIDs.
What You Should Do
If you’re on Warfarin, stop taking NSAIDs unless your anticoagulation specialist says otherwise. That includes aspirin, even low-dose aspirin-yes, even if your cardiologist prescribed it. Ask them if it’s still necessary.
Use acetaminophen (Tylenol) instead. It doesn’t affect platelets or the stomach lining. It’s not perfect-too much can damage your liver-but it’s the safest pain reliever for people on blood thinners. Topical creams with menthol or capsaicin work well for joint pain. Ice packs. Physical therapy. These are better options.
If you absolutely must take an NSAID, get your INR checked within 72 hours. Don’t wait. Don’t assume it’s fine. Bleeding can happen fast. Hemoglobin can drop 6 points in a day. You won’t feel it until you’re collapsing.
The Bigger Picture
This isn’t just about one drug interaction. It’s about how medicine fails patients. Millions of people take NSAIDs daily. Doctors prescribe them without thinking. Patients don’t realize they’re dangerous. Pharmacists don’t always warn them. Electronic health records don’t flag them.
The cost? $1.87 billion a year in the U.S. alone. Thousands of hospitalizations. Hundreds of deaths. And yet, 42.6% of Warfarin users still get NSAID prescriptions every year.
The good news? Co-prescribing has dropped 27% since 2015, thanks to more people switching to NOACs. But the bad news? That drop is being offset by more NSAID use with NOACs. We’re just moving the problem around.
The solution isn’t more drugs. It’s better awareness. Better communication. Better systems. And most of all-patients asking questions. If your doctor says "it’s fine," ask: "What’s the bleeding risk? What’s the evidence? Is there a safer option?""
Because the truth is simple: if you’re on Warfarin, NSAIDs are not a minor risk. They’re a major threat. And you don’t need them.
Can I take ibuprofen while on Warfarin?
No, it’s not safe. Ibuprofen increases your bleeding risk by nearly 80% when taken with Warfarin. It affects platelets and can cause stomach ulcers. Even occasional use can trigger a serious bleed. Use acetaminophen (Tylenol) instead for pain relief.
Is aspirin safe with Warfarin?
Aspirin is an NSAID and also interferes with platelet function. Taking it with Warfarin significantly raises bleeding risk, especially in the stomach and brain. Unless your doctor specifically recommends it for heart protection, avoid it completely. Never start aspirin on your own while on Warfarin.
What’s the safest painkiller for someone on Warfarin?
Acetaminophen (Tylenol) is the safest choice for pain or fever. It doesn’t affect platelets or the stomach lining. Stick to the recommended dose-no more than 3,000 mg per day-to avoid liver damage. For joint pain, try topical creams, ice packs, or physical therapy.
How often should INR be checked when taking NSAIDs with Warfarin?
If NSAID use is unavoidable, check INR before starting, then again 3 to 5 days after. Continue weekly monitoring while taking the NSAID. INR can spike quickly-sometimes within 48 hours. Don’t wait for symptoms. Bleeding can happen silently.
Do COX-2 inhibitors like celecoxib have less bleeding risk with Warfarin?
No. Studies show celecoxib and other COX-2 inhibitors carry the same bleeding risk as traditional NSAIDs when combined with Warfarin. They don’t protect the stomach lining enough to prevent bleeding. The idea that they’re safer is a myth.
What should I do if I accidentally took an NSAID while on Warfarin?
Stop taking the NSAID immediately. Contact your anticoagulation clinic or doctor right away. Get your INR checked within 24 to 48 hours. Watch for signs of bleeding: unusual bruising, blood in stool or urine, severe headaches, dizziness, or vomiting blood. Don’t wait for symptoms to get worse.
Can I take NSAIDs occasionally if my INR is stable?
Even if your INR is stable, NSAIDs can cause sudden spikes. The risk isn’t just about numbers-it’s about how the drugs interact physically in your body. Platelet function and stomach lining damage happen regardless of INR. Most experts say no safe occasional use exists. Avoid NSAIDs completely.
Are there any NSAIDs that are safe with Warfarin?
No. All NSAIDs-whether prescription or over-the-counter-carry increased bleeding risk with Warfarin. Naproxen and diclofenac are the worst, but even low-dose ibuprofen or aspirin can trigger a bleed. There is no safe NSAID for someone on Warfarin.





Amber Lane January 20, 2026
My grandma took ibuprofen for her arthritis and ended up in the ER with a GI bleed. She didn’t even know it was dangerous. This post saved her life.
Ben McKibbin January 21, 2026
Let’s be real-this isn’t just about drug interactions, it’s about systemic medical negligence. Doctors treat NSAIDs like candy, patients treat them like water, and nobody checks the fine print until someone’s hemoglobin drops into the toilet. The fact that 68% of cases involve patients who never told their doctor they were popping Advil? That’s not ignorance. That’s institutional failure wrapped in a white coat.
And don’t even get me started on the pharmaceutical marketing machine that convinced millions that celecoxib was the ‘safe’ NSAID. It’s not. It’s just a prettier poison. The data doesn’t lie. Platelets don’t care about your COX-2 selectivity. Your stomach lining doesn’t read clinical trial abstracts. It just bleeds.
We’ve got a generation of seniors on blood thinners who think Tylenol is ‘too weak’ and reach for the blue bottle because ‘it works faster.’ Meanwhile, ERs are filling up with people who didn’t know their headache medicine could kill them. This isn’t a cautionary tale. It’s a public health emergency dressed up as a Reddit post.
And yet, the system keeps chugging along. EHRs don’t flag it. Pharmacists don’t scream. Medical schools barely mention it. The only thing keeping people alive is word-of-mouth like this. So thank you. Keep writing. Someone’s life depends on it.
Stephen Rock January 22, 2026
so like… ibuprofen is literally a death sentence if you’re on warfarin? wow. who knew. also why is everyone acting like this is news. i’ve been telling people this for years. nobody listens. also my cousin died from this. just saying.
Kevin Narvaes January 23, 2026
they say tylenol is safe but what if you got liver issues? what then? everything is a tradeoff bro. life is just a series of bad choices with different levels of suffering.
Andrew Rinaldi January 24, 2026
I’ve sat in too many clinic waiting rooms watching elderly patients nod along while their doctor scribbles a prescription for naproxen like it’s aspirin. There’s a quiet tragedy here-not in the drugs, but in the silence between the questions people are too afraid to ask. ‘Is this really safe?’ ‘Could this kill me?’ ‘Why didn’t anyone tell me?’
We treat anticoagulation like a technical problem, when it’s really a human one. People don’t need more data. They need someone to look them in the eye and say, ‘I know you’re in pain, but this isn’t worth the risk.’ And then offer something better.
Acetaminophen isn’t glamorous. Ice packs don’t come in fancy packaging. Physical therapy requires effort. But those are the real solutions. Not the next pill. Just… less pills.
Philip Williams January 26, 2026
The data here is impeccable-2.09-fold increase in bleeding risk, FDA adverse event reports, JAMA and Circulation studies cited. This isn’t opinion; it’s evidence-based medicine at its most urgent. But what’s missing is the human layer: how do we change behavior? How do we make this stick?
Patients don’t forget Warfarin. They remember it because they get weekly INR checks. But NSAIDs? They’re OTC. They’re in the cabinet. They’re ‘just for a headache.’ That’s the gap. We need mandatory pharmacy counseling for anyone picking up anticoagulants, paired with a simple, bold sticker on every NSAID bottle: ‘DANGER: MAY CAUSE INTERNAL BLEEDING IF TAKEN WITH WARFARIN OR NOACS.’
And we need doctors to stop being passive. If you prescribe warfarin, you have a duty to ask: ‘Are you taking any painkillers?’ Not ‘do you take NSAIDs?’-because most patients don’t even know what NSAID means. Ask: ‘Are you taking ibuprofen, naproxen, aspirin, or anything for pain?’
Also, why are we still prescribing aspirin to people on anticoagulants? That’s not preventative-it’s reckless. The data shows no net benefit in most cases. It’s time to retire this outdated practice.
This post should be required reading for every medical student, pharmacist, and ER nurse. And every patient on warfarin should get a printed one-pager. No excuses. Lives are literally on the line.
Ashok Sakra January 27, 2026
i think this is all a big lie by big pharma to sell more tylenol and make doctors look smart. my uncle took naproxen for 10 years with warfarin and he’s fine. also i think the government is hiding the truth about blood thinners. maybe they want us to be weak.
shubham rathee January 29, 2026
they say no safe nsaid but what about cbd oil? i heard that works for pain and doesnt thin blood. maybe this whole thing is just to keep people buying pills