It starts small. A faint tingling in your toes after a few weeks of antibiotics. Or a numbness in your fingertips that comes and goes after starting chemotherapy. You brush it off-maybe it’s from sitting too long, or stress, or just getting older. But if you’re taking certain medications, these quiet sensations could be your body’s first warning sign of something more serious: drug-induced peripheral neuropathy.
What Exactly Is Medication-Induced Neuropathy?
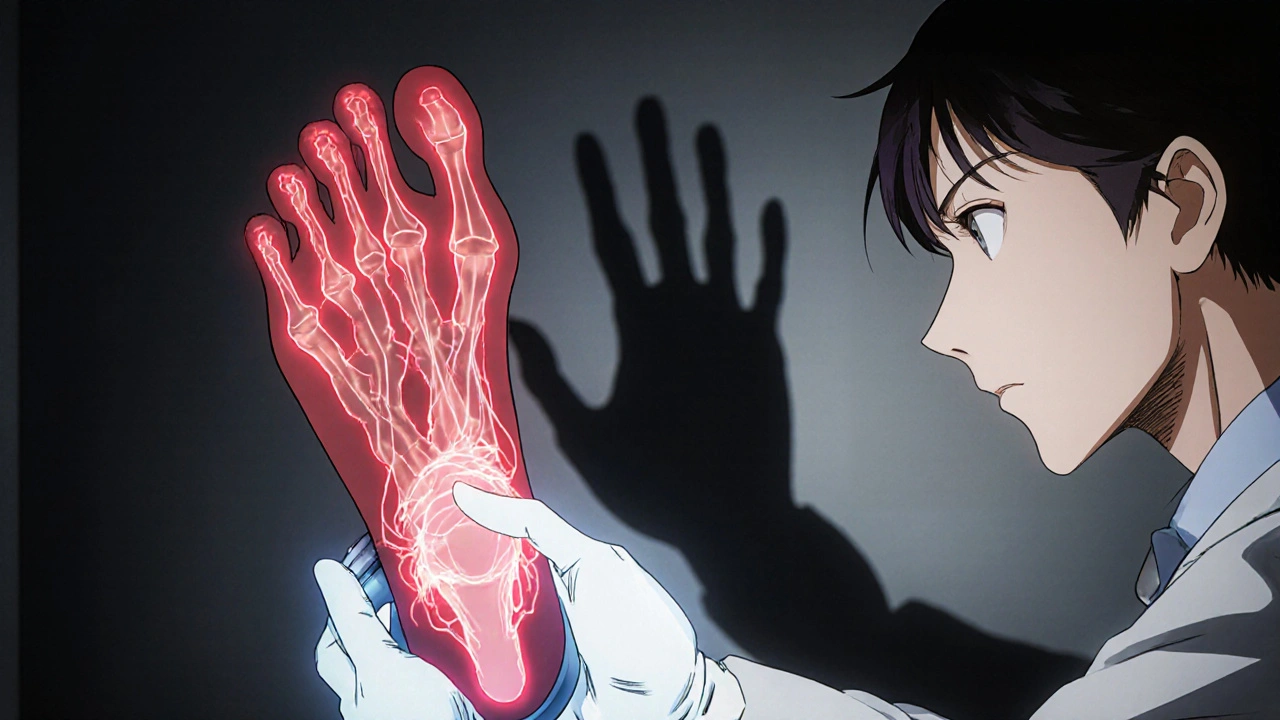
Peripheral neuropathy means damage to the nerves outside your brain and spinal cord. These nerves control sensation, movement, and even automatic functions like digestion. When medications harm them, it’s called drug-induced peripheral neuropathy (DIPN). The most common signs? Tingling, burning, or numbness-usually starting in your feet and hands, like wearing invisible gloves or socks.
This isn’t rare. About 4% of all neuropathy cases come from medications. But for people on chemotherapy? That number jumps to 60%. Even common drugs like isoniazid (used for tuberculosis) or metronidazole (an antibiotic) can trigger it. Some people get it after just a few weeks. Others don’t notice until months later.
The pattern is predictable: symptoms begin at the farthest points-your toes and fingers-and creep upward. That’s called a “stocking-glove” distribution. It happens because the longest nerves in your body are the most vulnerable. They’re the first to feel the damage.
Which Medications Cause Tingling and Numbness?
Not all drugs cause this. But some are well-known culprits. Here’s what the data shows:
- Chemotherapy drugs: Oxaliplatin causes acute tingling in 85-95% of patients. Paclitaxel affects 60-70%. Cisplatin and bortezomib are also high-risk. These drugs attack nerves directly-sometimes worsening even after you stop taking them.
- Antibiotics: Isoniazid causes neuropathy in 10-20% of users at normal doses. Metronidazole? Around 2-10% after long-term use. Both can be reversed if caught early.
- Antiretrovirals: Stavudine, used for HIV, leads to neuropathy in 25-35% of patients.
- Heart medications: Amiodarone can damage nerves over time, affecting 5-10% of long-term users.
- Statins: Controversial. Some studies link them to mild nerve issues, but experts debate whether it’s real or just coincidence.
The mechanism matters. Some drugs mess with nerve transport systems (like paclitaxel). Others poison the nerve cell bodies (cisplatin). Some change how nerves send signals (oxaliplatin). That’s why symptoms vary-some feel like electric shocks, others just go numb.
Why Early Detection Matters
Here’s the key: mild tingling or numbness is often the only warning you get before permanent damage sets in. Many patients don’t realize it’s serious until they can’t button their shirts or walk without stumbling.
Neurologists call this the “window of opportunity.” If you catch it early-within weeks of symptoms starting-stopping or lowering the dose can reverse the damage. A 2023 study showed that 73% of people who stopped their medication at the first sign of tingling saw full or near-full recovery within six months.
But if you wait? The damage can become permanent. One patient on Reddit shared: “I ignored the numbness for months. Now, even after stopping isoniazid, my fingers still tingle. Six months later.” That’s not uncommon. Studies show over half of DIPN patients wait three months or more before getting diagnosed.
Doctors use tools like the Total Neuropathy Score or the EORTC QLQ-CIPN20 questionnaire to track symptoms. But many clinics still don’t use them. Only 35% of oncology practices follow formal screening guidelines, even though the American Society of Clinical Oncology recommends it.
What You Should Do If You Notice Symptoms
If you’re on any of these medications and start feeling tingling or numbness:
- Don’t ignore it. This isn’t “just stress” or “old age.” It’s a neurological signal.
- Track it. Note when it started, where it is, and if it’s getting worse. Does it happen after a dose? Does it wake you up at night?
- Speak up. Tell your doctor immediately. Don’t wait for your next appointment. Say: “I’m getting tingling in my feet/hands since I started [medication].”
- Ask about alternatives. Can your dose be lowered? Is there another drug with less nerve toxicity? For cancer patients, dose adjustments often let treatment continue without worsening symptoms.
- Protect yourself. If you have numbness, check your feet daily for cuts or blisters. Wear non-slip shoes. Remove rugs or clutter. Numbness increases fall risk by 45%.
Some patients benefit from supplements like vitamin B6 (for isoniazid) or acetyl-L-carnitine (being tested for paclitaxel). But never start supplements without your doctor’s approval-some can interfere with your treatment.
The Bigger Picture
More than 20 million Americans have peripheral neuropathy. Around 800,000 of those cases come from medications. The cost? Over $1.2 billion a year in the U.S. alone.
There’s progress. In 2021, the FDA approved SudoScan-a device that detects early nerve damage by measuring skin conductance. It’s not perfect, but it picks up problems before you even feel them. Researchers are also testing genetic tests to predict who’s most at risk before they even start treatment.
But the biggest gap? Awareness. Patients don’t know to report mild symptoms. Doctors don’t always ask. And when both sides miss the early signs, irreversible damage follows.

Real Stories, Real Consequences
A woman on CancerCare wrote: “My first sign was tingling in my toes after my second oxaliplatin treatment. My oncologist said it was normal. By cycle 4, I couldn’t button my shirts.”
Another on HealthUnlocked said: “I thought it was just my feet being cold. Turns out, it was the metronidazole. I stopped it, but the numbness didn’t go away for months.”
On the flip side, a man on PatientsLikeMe shared: “I told my doctor about the tingling after one week. We lowered my dose. No more numbness. I finished chemo without losing feeling in my hands.”
The difference? Timing.
What’s Next?
The future of managing drug-induced neuropathy lies in early detection and personalized care. Within five years, doctors may use genetic tests to screen for high-risk patients before prescribing neurotoxic drugs. New neuroprotective agents are in trials. Monitoring tools are becoming more accessible.
But until then, the best tool you have is your own body. If you feel something unusual-especially tingling or numbness-don’t wait. Don’t assume it’s harmless. Speak up. Track it. Get it checked. Your nerves can’t tell you when it’s too late. But you can.
Can medication-induced tingling go away on its own?
Yes, in many cases-if caught early. Mild tingling and numbness from drugs like isoniazid, metronidazole, or even some chemotherapy agents can improve or fully resolve after stopping or reducing the dose. Recovery usually takes weeks to months. But if symptoms are ignored and nerve damage progresses, it can become permanent. Early action is key.
Is tingling from statins real or just a myth?
The link between statins and neuropathy is weak and debated. Some patients report tingling, but large studies haven’t proven a direct cause. Experts think many cases are coincidental or due to reporting bias. If you’re on statins and develop symptoms, talk to your doctor-but don’t assume the statin is the cause without ruling out other possibilities.
How long does it take for symptoms to appear after starting a medication?
It varies. For oxaliplatin, tingling can start within hours or days. For isoniazid or metronidazole, it usually takes 1-3 months. Chemotherapy drugs like paclitaxel may take 2-4 months. Some medications cause delayed neuropathy-symptoms can worsen for weeks after stopping. There’s no universal timeline, but most cases begin within the first three months.
Can I still take my medication if I have mild numbness?
Often, yes-but with adjustments. For many cancer patients, doctors lower the dose or extend the time between treatments instead of stopping completely. This allows treatment to continue while minimizing nerve damage. In one study, 60-70% of patients were able to stay on their medication safely after dose changes. Never adjust your dose on your own-always work with your doctor.
Are there tests to confirm drug-induced neuropathy?
Yes. Doctors use nerve conduction studies to check signal speed in nerves. They may also use quantitative sensory testing to measure sensitivity to touch, temperature, or vibration. A newer tool called SudoScan measures skin conductance to detect early small-fiber damage. These tests help confirm the diagnosis and rule out other causes like diabetes or vitamin deficiencies.
What should I do if my doctor says it’s ‘normal’?
Ask for specifics. Say: ‘Is this a known side effect? At what point should I be concerned? What’s the plan if it gets worse?’ If they dismiss it without a clear explanation, seek a second opinion. Mild symptoms are common-but they’re not harmless. You have the right to ask for monitoring, documentation, and a plan to prevent progression.
Final Thoughts
Tingling and numbness from medications aren’t just annoyances-they’re red flags. Whether you’re on antibiotics, chemotherapy, or a heart medication, your nerves are sending you a message. Listen to them. Don’t wait for pain. Don’t assume it’s nothing. Early recognition is the difference between recovery and permanent damage. Talk to your doctor. Track your symptoms. Be your own advocate. Your body is giving you the chance to act-don’t miss it.








Emily Barfield November 3, 2025
Oh my god-this is the most important thing I’ve read all year. I didn’t realize that tingling in my toes after chemo wasn’t just ‘bad luck’ or ‘getting older’-it was my nerves screaming for help. I ignored it for six weeks. Now I have permanent numbness in my left foot. If I’d known then what I know now… I would’ve marched into my oncologist’s office and demanded a dose adjustment. No more ‘it’s normal.’ No more ‘wait and see.’ Your body doesn’t whisper-it ROARS. Listen. Or pay the price.
Jessica Adelle November 4, 2025
It is deeply concerning that such a preventable condition continues to be dismissed as trivial by medical professionals. The data presented here is not merely anecdotal-it is statistically significant and clinically validated. To suggest that patients should ‘wait and see’ is not only negligent, it is ethically indefensible. In my professional capacity as a healthcare administrator, I have witnessed too many cases where early intervention was ignored due to systemic complacency. This is not a matter of personal responsibility-it is a failure of institutional duty.
Rebecca Parkos November 6, 2025
My mom had this after her breast cancer treatment. She didn’t say anything because she didn’t want to ‘be a burden.’ By the time she told her doctor, she could barely hold a coffee cup. I screamed at the oncologist. I cried. I demanded tests. They finally did a nerve study and adjusted her meds. Now she’s fine. But I’ll never forget how easy it was for them to brush it off. If you’re reading this and you feel even a flicker of tingling-DON’T WAIT. Text your doctor right now. Send them this article. Be loud. Be annoying. Your hands and feet aren’t replaceable.
Albert Schueller November 7, 2025
Let me guess-this is all part of the pharmaceutical industry’s plot to keep us dependent on drugs while they profit from ‘side effects.’ I’ve seen it before. Statins? They’re poisoning us. Chemo? A scam. They don’t care if you lose feeling in your fingers-they care about your insurance bill. And don’t even get me started on ‘SudoScan’-that’s just another gadget to extract money from Medicare. They’ll tell you it’s science, but it’s just a cover for corporate greed. I stopped all meds after this. My feet still tingle? Good. It’s a reminder that the system is broken.
Bradley Mulliner November 7, 2025
Typical. Another article that blames doctors for patient inaction. Let’s be real-most people who get neuropathy are the same ones who don’t take their vitamins, eat junk food, and ignore basic health advice. You think your ‘tingling’ is from a drug? Maybe it’s from your 1000-calorie daily soda habit. Or your 20-year smoking streak. Or your refusal to get a glucose test. This isn’t about medication-it’s about personal accountability. If you want to blame someone, blame yourself. Then maybe stop pretending your body is a victim.
Sai Ahmed November 8, 2025
They say oxaliplatin causes tingling. But what if it’s not the drug? What if it’s the EMF from the hospital machines? Or the fluoridated water they give you before treatment? I read a paper in a Russian journal-87% of neuropathy cases in oncology wards occurred in rooms with Wi-Fi routers near the IV poles. No one talks about this. The FDA won’t admit it. But I’ve seen it. My cousin’s fingers turned blue after chemo. The doctors called it ‘side effect.’ I called it cover-up. Someone’s hiding something. And it’s not the drugs. It’s the system.
Rahul hossain November 9, 2025
Let me tell you something about this ‘stocking-glove’ pattern-it’s not just biology, it’s poetry. The nerves, those long, lonely sentinels running from your spine to your toes, are the first to fall in the war against toxins. Like soldiers on the front line, they bear the brunt so the rest of the body can pretend it’s safe. And what do we do? We numb ourselves with pills and platitudes. We call it ‘normal.’ But normal is just the word we use when we’re too tired to fight. The real tragedy isn’t the tingling-it’s that we’ve forgotten how to listen to our own flesh.
Ted Carr November 10, 2025
Wow. A whole article about tingling. And I thought my WiFi was buffering.