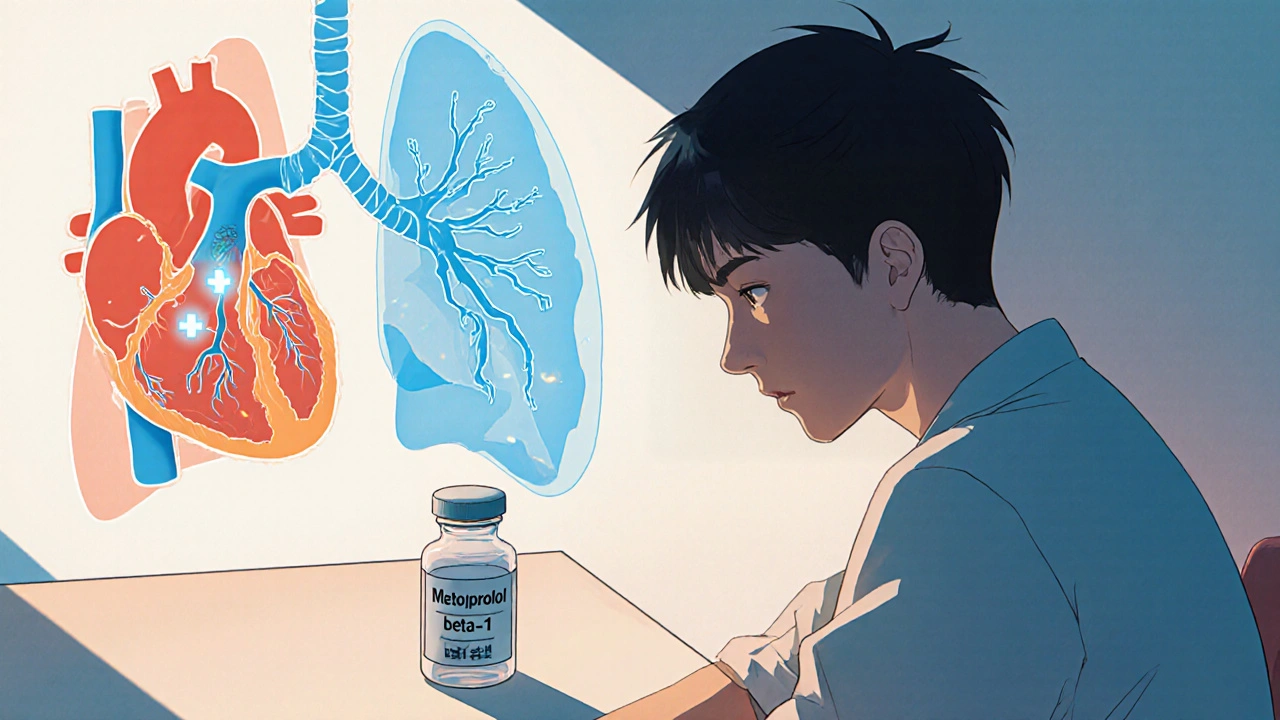
When a doctor prescribes a heart‑related drug, the last thing you want to wonder is whether it could set off your asthma. Metoprolol is a selective beta‑1 blocker used to treat high blood pressure, angina, and certain heart rhythm problems. It works by slowing the heart and reducing the force of each beat, which lowers the demand for oxygen. Asthma is a chronic inflammatory disease of the airways that makes breathing difficult, especially when the muscles around the bronchi tighten. Because both conditions involve the body’s adrenergic system, the combination raises red flags. This guide walks through how met‑oprolol interacts with the lungs, what the research says, and how you can stay safe.
How Metoprolol Works - The Good and the Caveats
Metoprolol belongs to a class called beta‑blockers. It is called “selective” because it prefers beta‑1 receptors, which are mainly in the heart. By blocking these receptors, the drug reduces heart rate (chronotropy) and contractility (inotropy). The result: lower blood pressure and less strain on a weakened heart.
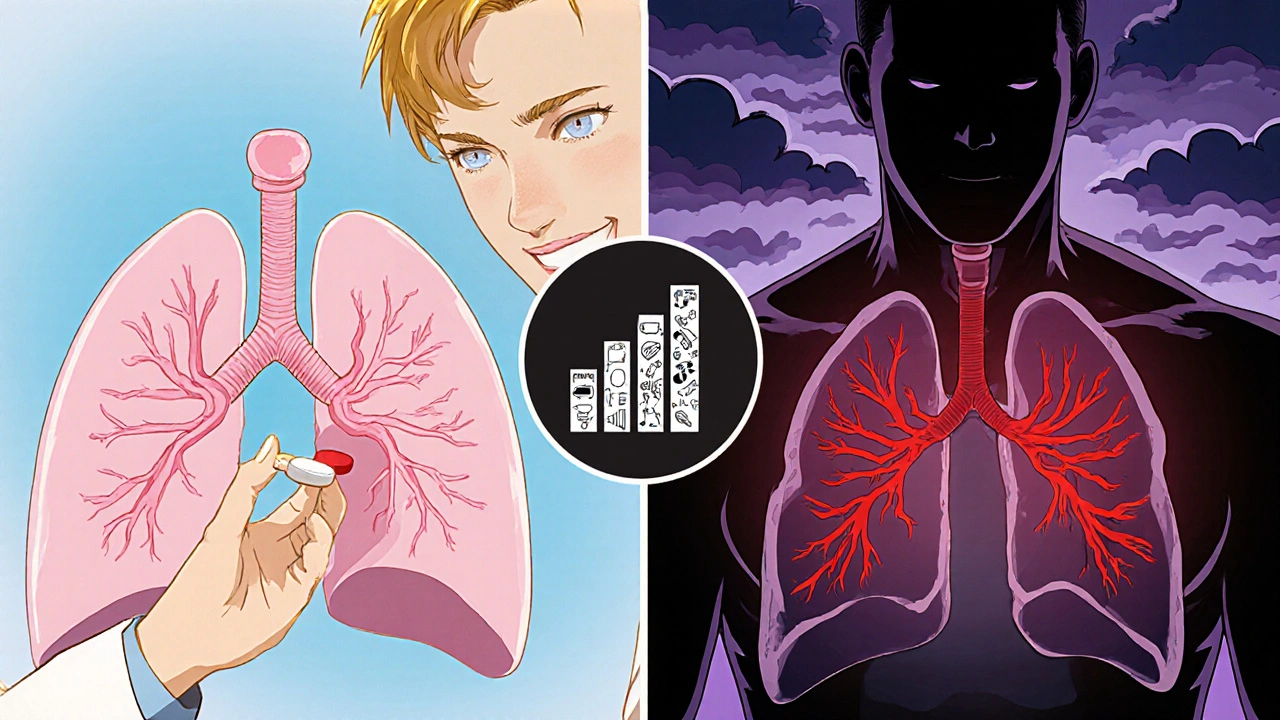
Unfortunately, no drug is 100 % selective. At higher doses, metoprolol can spill over onto beta‑2 receptors, the ones that sit in the smooth muscle of the lungs. Beta‑2 activation normally relaxes the airway muscles, so blocking them can cause bronchoconstriction - the very thing asthma patients try to avoid.
Why Asthma Patients Worry - A Quick Physiology Refresher
In asthma, the airway walls are inflamed and hyper‑responsive. When you breathe in an irritant, the body releases mediators that tighten the bronchial smooth muscle via beta‑2 receptors. Inhaled rescue inhalers (short‑acting beta‑agonists like albuterol) work by **activating** those same receptors, forcing the muscles to open.
If a medication blocks beta‑2 receptors, the rescue inhaler’s job becomes harder. The lung’s safety valve is partially shut, which can lead to:
- Worsening wheeze or cough
- Increased reliance on rescue inhalers
- Higher risk of an asthma attack that requires emergency care
For most people on low‑dose metoprolol, the spill‑over effect is minimal. The problem typically shows up when doses rise above 100 mg per day, when the drug is taken in combination with other non‑selective beta‑blockers, or when a patient already has severe airway hyper‑reactivity.
What the Clinical Evidence Says
Several observational studies and a few randomized trials have looked at the link between beta‑blockers and asthma events. A 2022 cohort study from the UK’s Clinical Practice Research Datalink (CPRD) followed 24,000 patients with asthma who started a beta‑blocker. Those on non‑selective agents (e.g., propranolol) had a 1.8‑fold higher risk of a hospital‑treated asthma exacerbation compared with those on selective agents like metoprolol.
Another smaller RCT published in the American Journal of Respiratory and Critical Care Medicine (2021) compared 50 mg versus 150 mg of metoprolol in patients with stable asthma and hypertension. The high‑dose group experienced a modest but statistically significant drop in forced expiratory volume in one second (FEV₁) - about 5 % from baseline - while the low‑dose group showed no change.
The take‑away numbers are useful:
- Low‑dose metoprolol (≤50 mg daily) rarely triggers clinically relevant bronchoconstriction.
- Mid‑range doses (50‑100 mg) may cause a slight decrease in lung function, especially in severe asthma.
- Doses >100 mg increase the odds of an asthma flare by roughly 30 % compared with non‑beta‑blocker controls.
Guidelines from the UK’s NICE and the US FDA echo these findings: they advise “cautious use of selective beta‑blockers in asthma, start low, go slow, and monitor lung function.”
Selective vs. Non‑Selective Beta‑Blockers - A Quick Comparison
| Drug | Receptor Selectivity | Typical Dose (mg/day) | Asthma Risk (Low‑Dose) | Common Cardiac Uses |
|---|---|---|---|---|
| Metoprolol | β₁‑Selective | 25‑100 | Minimal | Hypertension, angina, post‑MI |
| Atenolol | β₁‑Selective | 25‑100 | Low‑Moderate | Hypertension, arrhythmia |
| Propranolol | Non‑selective | 40‑240 | High | Migraine prophylaxis, tremor |
| Carvedilol | β‑non‑selective + α₁‑blocker | 12.5‑50 | High (due to β₂ block) | Heart failure, post‑MI |
The table makes it clear: if you have asthma, the safest bet is a low‑dose, β₁‑selective blocker. Even then, keep an eye on your breathing.
Practical Steps to Manage Metoprolol If You Have Asthma
Here’s a simple checklist you can use when you or a loved one starts metoprolol:
- Tell your prescriber about your asthma. Highlight severity, rescue inhaler use, and any recent exacerbations.
- Start low. Many clinicians begin at 25 mg once daily for asthma patients.
- Schedule a baseline spirometry test. Record FEV₁ and peak flow before the drug.
- Re‑check lung function after 2 weeks. A drop of more than 5 % warrants dose adjustment or a switch.
- Keep rescue inhalers handy. Use them at the first sign of wheeze rather than waiting.
- Know the red flags. Sudden shortness of breath, chest tightness, or a need for more than usual rescue inhaler doses should prompt immediate medical review.
- Consider alternatives. If lung function declines, ask about switching to an ACE inhibitor, ARB, or a calcium‑channel blocker for blood pressure control.
In practice, many patients stay on metoprolol without trouble, especially when the dose stays under 50 mg and they have mild asthma. The key is communication and monitoring.

When to Switch or Stop Metoprolol
If you notice any of the following, bring it up with your doctor right away:
- Repeated use of rescue inhaler more than twice a week
- Decline in peak flow readings >10 %
- Emergency department visit for asthma
- New onset of wheezing after dose increase
Your clinician may decide to:
- Reduce the dose.
- Switch to a different β₁‑selective blocker with a shorter half‑life (e.g., bisoprolol).
- Move to a non‑beta‑blocker antihypertensive.
Never stop a heart medication abruptly without medical supervision - sudden withdrawal can cause rebound tachycardia or angina.
Bottom Line for Patients
Metoprolol can be a lifesaver for heart disease, but its interaction with beta‑2 receptors means a cautious approach for anyone with asthma. Low doses are usually safe, but the moment you feel your lungs tightening, it’s time to act. Regular lung‑function checks, clear communication with your healthcare team, and an action plan for rescue inhaler use keep the balance right between protecting your heart and breathing easy.
Can I use an inhaled steroid if I’m on metoprolol?
Yes. Inhaled corticosteroids act on inflammation, not on beta‑receptors, so they’re safe and often recommended to lower the baseline risk of bronchoconstriction while you’re on a beta‑blocker.
Is atenolol a safer alternative to metoprolol for asthma?
Atenolol is also β₁‑selective, but some studies suggest a slightly higher spill‑over at comparable doses. Metoprolol has more extensive safety data in asthma, so it’s usually preferred if dosing stays low.
What dose of metoprolol is considered low enough for asthma patients?
Most guidelines cite ≤50 mg once daily as the low‑dose threshold. Below this, the risk of bronchoconstriction is minimal for mild‑to‑moderate asthma.
Should I stop metoprolol if I have an asthma flare?
Do not stop abruptly. Contact your doctor; they may lower the dose or switch you to a different cardiovascular drug while you recover.
Are there any non‑beta‑blocker blood pressure meds that are safer for asthma?
ACE inhibitors (e.g., lisinopril) and ARBs (e.g., losartan) have no effect on beta‑receptors and are widely used for hypertension in asthmatic patients.






Lionel du Plessis October 25, 2025
Metoprolol's β1 affinity is high but spill‑over at >100 mg is a real pharmacodynamic concern especially in asthmatics with hyper‑responsive airways
Andrae Powel October 28, 2025
I get how unsettling it can feel to take a heart medication when you also battle asthma. The key is to treat both conditions as a coordinated plan rather than isolated fixes. First, make sure your prescribing clinician knows the exact severity of your asthma – include recent spirometry numbers and how often you reach for your rescue inhaler. Starting metoprolol at 25 mg once daily is generally safe for most mild‑to‑moderate asthmatics, but keep a close eye on any subtle changes in breathing. Schedule a baseline lung function test before you begin the drug, and repeat it after two weeks to catch any early drop in FEV₁. If the follow‑up shows more than a 5 % reduction, discuss lowering the dose or switching to a different β1‑selective blocker such as bisoprolol, which some patients tolerate better. Remember that even a modest dose can cause bronchoconstriction in people with severe airway hyper‑reactivity, so listen to your body. Keep your short‑acting bronchodilator at hand and use it at the first hint of wheeze rather than waiting for a full attack. Many patients report that using an inhaled corticosteroid alongside metoprolol helps dampen baseline inflammation and provides a safety net. If you notice increased rescue inhaler usage – more than twice a week – that’s a red flag that warrants a prompt call to your doctor. In emergency situations, never stop metoprolol abruptly; sudden withdrawal can trigger rebound tachycardia or angina. Instead, have a plan with your provider to taper or substitute the medication under supervision. For those who cannot tolerate any β‑blocker, ACE inhibitors or ARBs are solid alternatives that have no effect on β2 receptors. Lifestyle measures such as regular aerobic exercise and a low‑salt diet can also improve blood pressure without additional drugs. Keep a written log of your blood pressure readings, heart rate, and peak flow values – the data will make it easier for your clinician to adjust therapy safely. Ultimately, open communication and routine monitoring are the best ways to protect both your heart and your lungs.
Leanne Henderson October 31, 2025
Wow, this guide really breaks it down, doesn’t it? I love how it charts the dose‑response curve, and the way it highlights the “start low, go slow” mantra is just spot‑on! It’s reassuring to see the numbers laid out, especially that ≤50 mg threshold, which feels like a safe sweet spot for most of us dealing with mild asthma. Also, the reminder to keep that rescue inhaler handy – that tiny puff can be a lifesaver, no joke! I’ve personally found that logging peak flow each morning adds an extra layer of confidence, you know? And the table comparing different beta‑blockers? Super helpful, I’ll definitely keep it bookmarked. Thanks for the thorough rundown, it’s exactly the kind of practical info we need!
Megan Dicochea November 3, 2025
Metoprolol can be used safely if you stay under the 50 mg mark. Watch for any increase in inhaler use. A simple spirometry check after two weeks helps catch issues early. Talk to your doctor about alternative blood pressure meds if problems arise. Keep a daily log of symptoms.
Jennie Smith November 6, 2025
Think of metoprolol as a gentle conductor guiding your heart’s rhythm, while your asthma is the wind section that needs breathing space. When the dosage stays low, the orchestra plays in harmony. If the beat gets too loud, the wind can sputter – that’s why you’ll want that rescue inhaler as your backstage pass. Keep the volume low, check your lung scores, and let your doc fine‑tune the meds. Your health symphony will stay in tune!
Anurag Ranjan November 9, 2025
Low‑dose metoprolol (≤50 mg) is generally safe for asthma; monitor lung function after dose changes.
James Doyle November 12, 2025
From a cardiological standpoint, the beta‑adrenergic blockade conferred by metoprolol offers undeniable benefits in reducing myocardial oxygen demand, yet the pharmacodynamic nuance of β2 receptor spill‑over cannot be dismissed outright. The literature underscores a dose‑dependent gradient where supratherapeutic dosing (>100 mg) skews the selectivity index, thereby precipitating bronchoconstrictive sequelae in susceptible phenotypes. Moreover, the interplay between adrenergic tone and airway hyper‑responsiveness is a classic example of iatrogenic compromise, demanding vigilant titration. Clinical guidelines rightly advocate for a “start low, go slow” paradigm, but real‑world adherence to this principle remains sporadic at best. Patients often report an insidious onset of wheeze, which may be misattributed to environmental triggers rather than medication effect. Consequently, a multidisciplinary approach involving both cardiology and pulmonology should be institutionalized. Routine spirometry, coupled with peak flow diary maintenance, provides objective metrics for early detection. In cases where lung function deteriorates, transitioning to alternative agents such as bisoprolol or non‑beta‑blocker antihypertensives is both prudent and evidence‑based. Ultimately, the clinician’s duty is to balance hemodynamic optimization with respiratory safety, lest we gamble with preventable exacerbations.
Greg Galivan November 14, 2025
Don’t ignore the warning signs.
ALBERT HENDERSHOT JR. November 16, 2025
Your enthusiasm for patient empowerment is commendable, and the emphasis on self‑monitoring aligns with best‑practice principles. By maintaining a systematic log of peak flow readings, individuals can detect subtle trends before they culminate in an acute episode. This proactive stance not only safeguards pulmonary function but also reinforces adherence to cardiovascular therapy. The integration of such self‑care strategies exemplifies a holistic model of chronic disease management 😊.
Suzanne Carawan November 19, 2025
Oh sure, because logging numbers magically cures asthma, right?
Edward Brown November 21, 2025
Some pharma trials hide the true spill‑over risks they claim to study, so the data we see may be filtered to protect market share.
Kala Rani November 23, 2025
Even the “high‑dose” threshold is arbitrary, real world patients vary wildly.