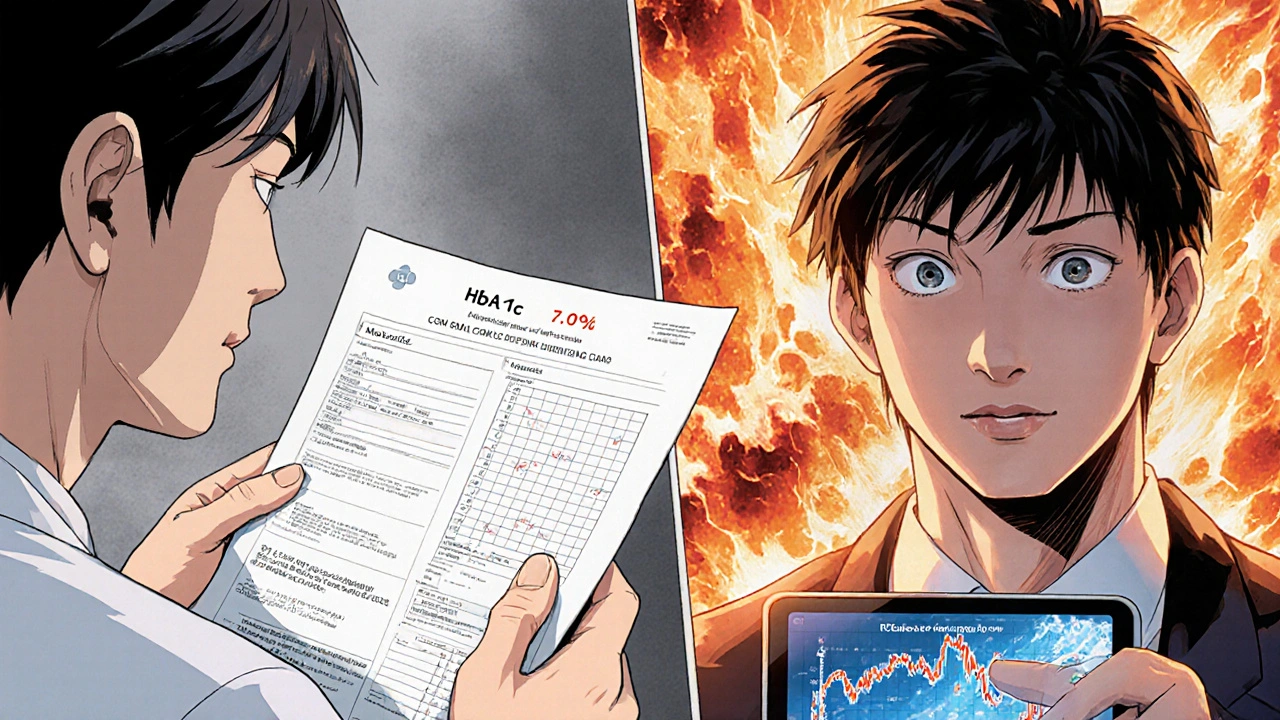
Most people with diabetes know their HbA1c number. It’s the number doctors check every three months - a single number that claims to tell you how well your blood sugar is controlled. But what if that number is lying to you? Two people can have the same HbA1c of 7.0%, yet one spends 18 hours a day with blood sugar in range, while the other spikes to 250 mg/dL after every meal and crashes to 55 mg/dL at night. Their HbA1c looks identical. Their risks? Not even close.
This is where Time in Range changes everything.
Time in Range (TIR) isn’t just another metric. It’s the first real window into your daily glucose patterns. Instead of averaging your blood sugar over months, TIR shows you exactly how much time you spend between 70 and 180 mg/dL (3.9-10.0 mmol/L) - the sweet spot where your body functions best without the danger of highs or lows. The goal? At least 70% of the day, or about 17 hours. That’s not a suggestion. It’s the standard endorsed by the American Diabetes Association in their 2025 Guidelines.
Why HbA1c Isn’t Enough Anymore
HbA1c measures the percentage of hemoglobin coated in glucose over the past 90 days. It’s useful. But it’s like reading the last page of a novel and calling it a summary. You miss the plot twists, the tension, the near-misses.
Imagine you’re driving. Your speedometer says you averaged 55 mph all day. Sounds fine, right? But what if you spent 4 hours stuck in traffic at 10 mph, then 3 hours speeding at 90 mph? You’d be in danger the whole time - and your average speed wouldn’t tell you that. That’s HbA1c. TIR is the dashboard showing you every second of your drive.
Studies show that even when HbA1c is “good,” people with low TIR are still at higher risk for complications like nerve damage, eye problems, and heart disease. One 2023 study from the Cleveland Clinic found that patients with identical HbA1c levels had wildly different TIR values - and those with lower TIR had more frequent hypoglycemic events, even if they never felt them.
That’s the hidden danger. You can feel fine, have a “normal” HbA1c, and still be doing damage - quietly, constantly.
How CGM Makes TIR Possible
Time in Range only exists because of continuous glucose monitoring (CGM). These small sensors, worn on your arm or belly, measure your interstitial glucose every 5 minutes. That’s over 1,400 readings in two weeks. No fingersticks. No guessing. Just raw, real-time data.
CGM devices from Dexcom, Abbott, and Medtronic don’t just show you a number. They show you a story. A graph. A pattern. You can see how your blood sugar reacts to coffee, stress, walking after dinner, or that “healthy” granola bar you thought was safe.
For someone with type 2 diabetes not on insulin, this is revolutionary. Before 2025, CGM was mostly reserved for insulin users. Now, the ADA says: if you’re on metformin, GLP-1s, or SGLT2 inhibitors - you should consider CGM. Why? Because even non-insulin users have dangerous glucose swings. And TIR helps you catch them.
The data isn’t just for your doctor. It’s for you. You learn what your body does - not what the chart says it should do.
The Three Key Metrics You Need to Know
TIR doesn’t work alone. It’s part of a trio:
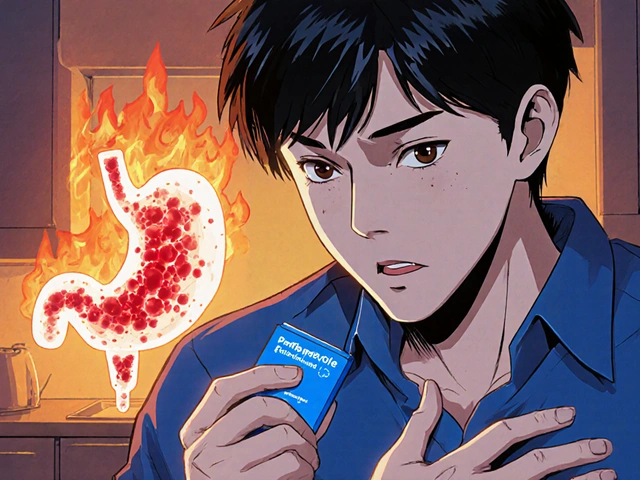
- Time in Range (TIR): 70-180 mg/dL. Aim for at least 70% of the day.
- Time Below Range (TBR): Below 70 mg/dL. Keep it under 4% of the day - that’s less than an hour. Below 54 mg/dL? That’s severe hypoglycemia. Keep it under 1%.
- Time Above Range (TAR): Above 180 mg/dL. Less than 25% is ideal. The lower, the better.
These numbers are your daily scorecard. If your TIR is 65%, your TBR is 6%, and your TAR is 30%, you’re not just “managing” diabetes - you’re fighting it. But if your TIR jumps to 75%, TBR drops to 2%, and TAR falls to 18%, you’re winning.
Some people aim for “Time in Tight Range” - 70-140 mg/dL. That’s what people without diabetes spend most of their time in. It’s ambitious. Not for everyone. But for those chasing optimal health, it’s a real target.
Real-Life Wins: What TIR Actually Changes
One patient in Bristol, a 58-year-old with type 2 diabetes on metformin, had an HbA1c of 7.1%. She felt fine. But her CGM showed she was below 70 mg/dL three times a week - often at 3 a.m. She didn’t wake up. No shakiness. No sweating. Just silent lows.
Her TIR was only 58%. Her doctor adjusted her evening medication timing. She started eating a small protein snack before bed. Two weeks later, her TIR was 74%. Her TBR dropped to 1.5%. Her HbA1c didn’t change much - still 7.0%. But her risk of falling, of brain fog, of hospital visits? Plummeted.
Another man noticed his glucose spiked after eating quinoa. He thought it was a “healthy carb.” His CGM said otherwise. He swapped it for lentils. His TIR jumped 12% in a month.
These aren’t miracles. They’re adjustments. Based on data. Not guesswork.
What Gets in the Way?
CGM isn’t perfect. Sensors can fall off. Some people get skin irritation. Others feel overwhelmed by the numbers. One woman told me she cried the first time she saw her graph - “It was like seeing my body scream for help.”
Cost and access still matter. In the UK, NHS access to CGM for type 2 diabetes is still patchy. Private options exist, but they’re expensive. Insurance coverage in the US improved after the 2025 ADA guidelines, but many still fight for approval.
And then there’s the learning curve. You can’t just slap on a sensor and know what to do. You need to understand the graphs. Know what “coefficient of variation” means (it’s how much your glucose swings - lower is better). Learn how to spot patterns: dawn phenomenon, post-meal spikes, overnight drops.
That’s why working with a diabetes educator matters. The Association of Diabetes Care & Education Specialists (ADCES) has training programs specifically for interpreting TIR data. One visit isn’t enough. You need follow-ups. You need to ask: “Why did I spike after lunch? Was it the bread? The stress? The lack of sleep?”

The Future Is Here - And It’s Personal
The global CGM market is growing fast - from $4.8 billion in 2022 to an expected $18.6 billion by 2030. Why? Because people are realizing: control isn’t about averages. It’s about consistency.
AI is starting to help. Some newer CGM apps now suggest: “Your TIR dropped last night. Try moving your dinner earlier.” Or: “You had 3 spikes after pasta. Try reducing portion size by 20%.”
And research is catching up. A 2025 study in the Journal of Clinical Endocrinology & Metabolism found that people who spent more than 80% of their day in range had a 40% lower risk of kidney disease progression over five years - even after adjusting for HbA1c.
That’s the power of TIR. It doesn’t just help you feel better today. It helps you live longer.
Where to Start
If you’re not using CGM yet, here’s how to begin:
- Ask your doctor if CGM is right for you - especially if you’re on any glucose-lowering medication, even if you don’t use insulin.
- Request a 14-day CGM trial. Most manufacturers offer them.
- Wear it consistently. At least 70% of the time - that’s 10+ days. No skipping nights.
- Look at your TIR, TBR, and TAR every week. Don’t just glance. Ask: What’s causing the dips? The spikes?
- Bring your data to your next appointment. Don’t just say “I’m doing okay.” Show them your graph.
Don’t wait for your HbA1c to be “bad.” If you’re already at 7%, you’re not safe. You’re just not showing symptoms yet.
Time in Range isn’t about perfection. It’s about awareness. It’s about catching the spikes before they become complications. It’s about knowing your body - not just your lab report.
The future of diabetes care isn’t just about pills and insulin. It’s about data. And if you’re not using TIR, you’re flying blind.





Bailey Sheppard November 18, 2025
Really appreciate this breakdown. I’ve been on CGM for a year now and TIR changed everything - not because my HbA1c dropped, but because I stopped waking up terrified at 3 a.m. The graph showed me my body was crashing silently. Now I eat a handful of almonds before bed. Simple. No drama. Just data.
Girish Pai November 19, 2025
Finally, someone in the West is talking about real metrics. In India, we’ve been using continuous glucose monitoring in urban clinics for years - but Western medicine still clings to HbA1c like it’s gospel. TIR isn’t just better - it’s scientifically superior. The ADA finally caught up. Took them long enough.
Kristi Joy November 20, 2025
If you’re new to CGM, don’t panic when you see spikes. It’s not failure - it’s feedback. I started with a 52% TIR. I thought I was doomed. But I learned that my coffee with creamer spiked me. My evening walk dropped my overnight lows. Small tweaks. Big wins. You got this.
Hal Nicholas November 21, 2025
Everyone’s acting like TIR is some revolutionary breakthrough. Newsflash: we’ve known for decades that averages lie. The real problem? Doctors still don’t know how to interpret this data. Most of them still look at HbA1c and call it a day. This post is good - but the system is broken.
Louie Amour November 23, 2025
Look, if you’re not tracking TIR, you’re not serious about your health. I’ve seen people with HbA1c of 6.5% and TIR of 45% - they’re walking time bombs. And they wonder why they get neuropathy at 45. It’s not magic. It’s math. Stop pretending you’re healthy because your lab report says so.
Kristina Williams November 23, 2025
CGM is a Big Pharma scam. They’re pushing sensors so you’ll buy more insulin and meds. The real cause of diabetes? Glyphosate in your food and vaccines. Look up the CDC’s hidden 2018 memo - they admit glucose spikes are triggered by environmental toxins, not carbs. TIR? Just a distraction.
Christine Eslinger November 25, 2025
I’ve been teaching diabetes self-management for 12 years, and TIR is the single most transformative tool I’ve seen. Not because it’s new - but because it turns abstract numbers into lived experience. One patient cried when she saw her graph: ‘I thought I was fine. But I was falling apart every night.’ That’s the power of visibility. Data doesn’t lie. It just waits for you to look.
It’s not about perfection. It’s about awareness. You don’t need to hit 80% TIR to win. Just move the needle. One percent. One day. One meal at a time.
And if you’re waiting for your doctor to lead you - don’t. Bring the data. Ask the questions. You’re the expert on your body. They’re just the guide.
Denny Sucipto November 26, 2025
My wife started CGM last year after her HbA1c hit 7.3. She thought she was doing fine. Then she saw her graph - spikes after ‘healthy’ oatmeal, crashes after yoga. She swapped oatmeal for eggs. Started walking after dinner. Now her TIR is 78%. She says it’s like she got her life back. Not because she lost weight. Not because her meds changed. Just because she finally saw what was happening.
It’s not about being perfect. It’s about being present. Your body’s talking. Are you listening?
Holly Powell November 28, 2025
Let’s be honest - TIR is just a rebranding of glucose variability metrics that have been studied since the early 2000s. The coefficient of variation, mean amplitude of glucose excursions, LAGE - all of this was published in Diabetologia long before CGMs hit the mainstream. The ADA’s 2025 guidelines are merely catching up to peer-reviewed science that’s been ignored by clinicians for a decade. This isn’t innovation. It’s institutional tardiness.
Emanuel Jalba November 28, 2025
THIS IS THE TRUTH 💔 I used to think I was fine. Then I saw my graph. I was in hypoglycemia 6 hours a day. I didn’t feel it. My kids didn’t know. I almost passed out driving to school. CGM saved my life. 🙏 If you’re not using it - you’re gambling with your future. Don’t be that guy. Get the sensor. NOW. 🚨
Heidi R November 30, 2025
Why are you all so obsessed with numbers? Your body knows what it needs. Stop overanalyzing. Just eat real food and move. The sensor is just another way to stress yourself out.
Brenda Kuter November 30, 2025
CGM is a government mind-control tool disguised as healthcare. They’re tracking your glucose to predict your behavior. You think this is about health? No. It’s about data harvesting. Next thing you know, your insurance will raise your rates if your TIR dips below 70%. This is surveillance capitalism in a bandage.