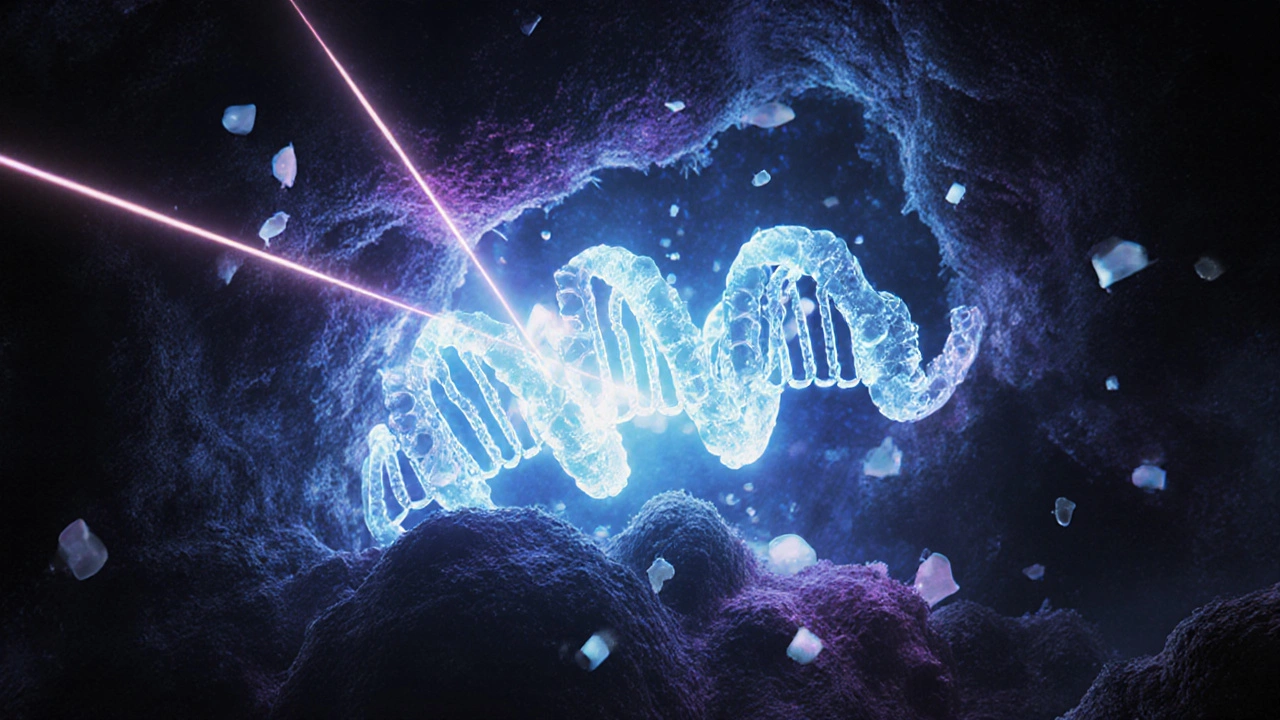
For decades, cancer treatment meant one thing: poison. Chemotherapy attacked every fast-dividing cell in the body-cancerous or not. Patients lost their hair, their energy, their appetite. Many didn’t survive. But today, something quieter, smarter, and more powerful is replacing that old model. Targeted therapy doesn’t guess. It doesn’t scatter shot. It reads the DNA of your tumor and strikes only what’s broken.
How Targeted Therapy Works
Think of cancer cells as cars with stuck accelerators. Normal cells have brakes-genes like TP53 or PTEN that tell the cell when to stop dividing. In cancer, those brakes fail. At the same time, the accelerator pedal-genes like EGFR, ALK, or BRAF-gets jammed down. Targeted therapy doesn’t blow up the whole car. It finds the stuck pedal and cuts the fuel line.
This isn’t science fiction. It’s based on data from The Cancer Genome Atlas, which mapped the DNA of over 20,000 tumors across 33 cancer types. The results were clear: cancers that look the same under a microscope can have wildly different genetic causes. That’s why two patients with lung cancer might need completely different drugs. One might have an EGFR mutation. Another, an ALK fusion. The treatment isn’t about where the tumor lives-it’s about what’s broken inside it.
The first big win came with imatinib (Gleevec) in 2001. It targeted a specific fusion gene in chronic myeloid leukemia. Before imatinib, 20-30% of patients survived one year. After? 89%. That wasn’t just an improvement. It was a revolution.
What Gets Targeted?
Most targeted drugs focus on oncogenes-genes that have gone rogue and are pushing cells to multiply nonstop. These include:
- EGFR: Common in lung cancer, especially in non-smokers. Drugs like osimertinib block its signal.
- ALK: Found in about 5% of lung cancers. Crizotinib and alectinib shut it down.
- BRAF: Present in melanoma and some colorectal cancers. Vemurafenib and dabrafenib target it.
- HER2: Overactive in 20% of breast cancers. Trastuzumab sticks to it like a magnet.
- NTRK: Rare, but found in many tumor types. Larotrectinib works across lung, thyroid, even salivary gland cancers if NTRK is present.
These drugs come in two main forms. Small molecules-like pills you swallow-get inside the cell and block signals from the inside. Monoclonal antibodies-like trastuzumab-are lab-made proteins that latch onto targets on the cell surface, like flags on a battlefield.
There’s one big gap: tumor suppressor genes. These are the brakes that break. TP53, for example, is mutated in over half of all cancers. But we still don’t have drugs that can fix a broken brake. That’s the next frontier. Right now, 92% of approved targeted therapies go after the accelerator-not the brake.

How Do You Know If It’s Right for You?
Before you start any targeted therapy, you need a genetic map of your tumor. This isn’t a blood test. It’s a biopsy-tissue from the tumor is sent to a lab for next-generation sequencing (NGS). Panels like FoundationOne CDx or MSK-IMPACT scan 300 to 500 cancer-related genes at once.
It takes about 14 to 21 days to get results. You need at least 20 nanograms of DNA and 20% tumor cells in the sample. If the sample is too small or too full of normal cells, the test fails. That’s why some patients get false negatives.
And not everyone qualifies. Only about 13.8% of cancer patients have a mutation that matches an approved targeted drug. For some, like those with NTRK fusions, the drug works no matter where the cancer started. That’s called “tissue-agnostic” treatment. Larotrectinib, for example, has a 75% response rate across 17 different cancers if NTRK is present. But for most, the drug only works for one cancer type.
How Effective Is It?
When it works, it works dramatically.
In EGFR-mutant lung cancer, osimertinib extends the time before the cancer grows from 10.2 months with chemo to 18.9 months. That’s nearly double. And side effects? Far milder. Only 15-30% of patients on targeted drugs get severe reactions. With chemo, it’s 50-70%.
One patient in Bristol, diagnosed with stage IV lung cancer and an EGFR mutation, started osimertinib in early 2024. Within eight weeks, her tumor shrank by 80%. She didn’t lose her hair. She kept working. She traveled to see her grandchildren. That’s not just survival. That’s living.
But here’s the catch: targeted therapy doesn’t cure most cancers. It controls them-for a while. In 70 to 90% of cases, the cancer finds a way around the drug. New mutations pop up. The brake fails again. The accelerator reactivates. That’s why doctors now use liquid biopsies-blood tests that catch tumor DNA floating in the bloodstream. These can spot resistance mutations months before a scan shows growth.

The Cost and Access Problem
Targeted therapy isn’t cheap. A single month can cost $15,000 to $30,000. Chemo? $5,000 to $10,000. And the testing? Around $5,500 per panel.
Insurance denials are common. One in two patients with rare mutations report delays or refusals for testing. Some wait over a month just to get approval. A 2023 study found 40% of patients on targeted therapy faced financial hardship-losing savings, skipping meals, or skipping doses to save money.
Access isn’t equal. In the U.S., 65% of advanced cancer patients get genomic testing. In Europe, it’s 22%. In parts of Asia, it’s 8%. Even within the U.S., community hospitals often lack the labs, pathologists, or genetic counselors needed. Only 32% of community hospitals have molecular tumor boards. Academic centers? 89% do.
And when a drug is approved for one cancer type but works in another? Insurance often says no. A Reddit user with an NTRK fusion wrote: “My tumor is in my salivary gland. Larotrectinib works for 75% of people with this mutation, no matter where it is. But my insurer says it’s ‘not standard for my cancer type.’”
What’s Next?
The field is moving fast. Researchers are testing combinations-targeted drugs with immunotherapy, or two targeted drugs together-to delay resistance. The NCI’s RESPOND initiative is investing $195 million to fix racial disparities in testing and treatment. AI tools like IBM Watson for Oncology now match tumor profiles to therapies with 93% accuracy.
By 2030, McKinsey predicts 40% of cancer patients will get treatment based on their tumor’s genetics. But that future depends on three things: better access, lower costs, and smarter science.
We’re learning how to target not just the tumor’s mutations, but its environment-its blood supply, its immune defenses, its hidden allies. The goal isn’t just to shrink tumors. It’s to turn cancer into a chronic condition, like diabetes or high blood pressure. Manageable. Controllable. Not a death sentence.
For now, targeted therapy isn’t for everyone. But for those it helps, it’s not just treatment. It’s time. Time to live. Time to be with family. Time to hope.
How is targeted therapy different from chemotherapy?
Chemotherapy attacks all fast-growing cells-cancerous and healthy-leading to side effects like hair loss, nausea, and low blood counts. Targeted therapy only attacks cancer cells with specific genetic mutations. It’s like using a key to unlock a single door instead of blowing up the whole building. Side effects are usually milder, and response rates are much higher in patients whose tumors have the right mutation.
Do all cancer patients qualify for targeted therapy?
No. Only about 10-15% of solid tumors have currently actionable genetic targets. For some cancers, like lung or melanoma, the chance is higher-up to 30-40%. For others, like pancreatic or ovarian, it’s much lower. Testing is required to find out. Even then, only 13.8% of patients in large studies have a mutation that matches an approved drug.
How long does genetic testing take?
Standard tumor genetic testing takes 14 to 21 days from the time the biopsy is sent to the lab. Some faster tests can return results in 7-10 days, but they often cover fewer genes. Insurance approval and sample quality can add delays. If the sample doesn’t have enough tumor DNA, the test may need to be repeated.
What happens if targeted therapy stops working?
Resistance is common. In 70-90% of cases, the cancer develops new mutations that bypass the drug’s effect. When that happens, doctors often order another biopsy or a liquid biopsy to find the new mutation. Sometimes, a second-line targeted drug can be used. In other cases, chemotherapy, immunotherapy, or clinical trials become the next step.
Can targeted therapy be used for early-stage cancer?
Yes-but only in specific cases. For example, EGFR inhibitors are now used after surgery in early-stage lung cancer with EGFR mutations to reduce the risk of recurrence. This is called adjuvant therapy. But most targeted therapies are still used for advanced or metastatic disease, where the genetic changes are easier to detect and the benefits are clearer.
Are there any targeted therapies for breast cancer?
Yes. HER2-positive breast cancer is one of the biggest success stories. Trastuzumab, pertuzumab, and ado-trastuzumab emtansine (T-DM1) target the HER2 protein and have dramatically improved survival. For hormone-receptor-positive breast cancer, drugs like palbociclib and ribociclib block cell cycle proteins (CDK4/6) and are used with hormone therapy. Testing for HER2 and hormone receptors is now standard for all breast cancer patients.
Why isn’t targeted therapy used for all cancers yet?
Because not all cancers have known, druggable targets. Many tumors have mutations in genes we can’t yet target-like TP53, which is broken in over half of all cancers. Also, some mutations are too complex to block with a pill. Drug development takes years. And even when a target exists, the drug must be tested in clinical trials, approved by regulators, and made affordable. It’s a slow, expensive process.
Is genetic testing covered by insurance?
Most major insurers in the U.S. cover FDA-approved genomic tests for advanced cancers, especially if a targeted therapy is available. But prior authorization is often required, and denials are common-especially for rare mutations or off-label use. Patients may need to appeal or seek help from patient advocacy groups. In the UK, testing is available through the NHS for certain cancers, but access varies by region and tumor type.
Targeted therapy is changing the way we think about cancer-not as a single disease, but as hundreds of diseases, each defined by its own genetic fingerprint. The future isn’t about one-size-fits-all treatment. It’s about matching the right drug to the right mutation, for the right person. We’re still early in this journey. But for the first time, many patients aren’t just surviving cancer. They’re living with it.





Liam Strachan November 19, 2025
Really well written piece. I’ve got a cousin who’s on osimertinib right now-she’s back to gardening and even took a trip to Scotland last month. No hair loss, no nausea, just… living. It’s wild how much this stuff changes the game when it works.
Katie Magnus November 21, 2025
OMG this is so basic. Like… duh. Of course you don’t blast the whole body. I mean, I read this in a magazine in 2015. Why is this even a thing now?? Also, I heard the drugs are basically just fancy placebos for rich people. #FakeScience
King Over November 21, 2025
imatinib changed everything. 89% survival? yeah. no more chemo for some. that’s it. done. next
Johannah Lavin November 23, 2025
THIS. I’m crying. My mom got on larotrectinib last year-salivary gland cancer, rare as hell. She’s been in remission for 14 months. No chemo. No hospital stays. She’s baking pies again 🥧💖. If you’re reading this and you’ve been told ‘there’s nothing more we can do’… get that genetic test. Please. It’s worth the fight.
Ravinder Singh November 25, 2025
Bro, this is the future right here. In India, we barely have access to basic chemo, let alone NGS panels. But I’ve seen patients in Pune get tested through NGOs-$200 instead of $5k. One guy with NTRK fusion? Lived 4 years on larotrectinib. We need global equity here. Not just for the rich. Not just in the US. Cancer doesn’t care where you live. Neither should treatment.
Also, TP53 is the holy grail. If we crack that, we’re talking about curing half of all cancers. Someone’s gotta fund that. We can’t just keep patching accelerators forever.
And hey-doctors, please stop acting like patients are dumb. We read. We Google. We want to understand. Just talk to us like humans, not problems to solve.
Russ Bergeman November 25, 2025
Wait-so you’re telling me… we’re spending $30K a month… on a pill… that… doesn’t even cure… and only works for 13.8% of people? And you call this progress? What about all the people who don’t qualify? Are they just… left to die? And why is insurance denying it? Are we just… playing roulette with people’s lives now? This is insane. I’m not mad… I’m just… disappointed.
Dana Oralkhan November 27, 2025
I work in oncology nursing. I’ve seen the before and after. One patient, 62, with metastatic melanoma-BRAF mutation. Started dabrafenib. Walked into the clinic in a wheelchair. Left three weeks later, walking to the parking lot without help. She cried. I cried. This isn’t just science. It’s dignity. But I also see the ones who can’t afford it. Or wait six months for insurance. Or get a false negative because their biopsy was too small. We need better systems. Not just better drugs.
Jeremy Samuel November 28, 2025
targeted therapy? more like targeted marketing. i heard they just repackage old drugs and call it new. also, why do all these studies only use white people? my cousin in australia has the same mutation as that lady in the article but they told her 'nope, not for you' because her skin is darker. so… yeah. not so smart after all.
Destiny Annamaria November 29, 2025
Just moved from Nigeria to the States last year. In Lagos, my uncle got chemo with no CT scan, no blood work, just a needle and hope. Here? They do 500-gene panels, AI matching, clinical trials. It’s like comparing a bicycle to a rocket. But then I see people complaining about $15k/month and I just… I don’t know. We’re so lucky. And so broken at the same time. 💔
Alyssa Torres December 1, 2025
My sister got tested after her recurrence. Found an NTRK fusion. They said ‘this drug doesn’t have your cancer type on the label.’ But it worked. For her. For 75% of others. So why is insurance so scared of science? Why are we still treating cancer like it’s one disease? We need to stop letting bureaucracy kill people who already have enough to fight. I’m not asking for a miracle. I’m asking for fairness.