Every year, over 100,000 people in the U.S. die from drug overdoses. Most of these deaths happen at home - not in hospitals or emergency rooms. And in many cases, the person who could have saved a life was right there - but didn’t know what to do. If someone in your home takes prescription opioids, benzodiazepines, or even just a mix of medications, you need a clear, simple plan. Not someday. Not "if something happens." Now.
Why This Plan Isn’t Optional
You don’t need to be an addict or live with substance use disorder to need this plan. Overdoses happen to people taking pain meds as directed. They happen to elderly parents mixing prescriptions. They happen to teens experimenting with pills they found in a cabinet. The most dangerous drugs today - fentanyl, carfentanil, synthetic opioids - are so strong that a single pill can kill. And they often hide in pills that look like ordinary painkillers.The good news? You can stop most of these deaths before 911 arrives. Naloxone, the overdose-reversal drug, works in 2 to 5 minutes. But only if it’s nearby, you know how to use it, and you act fast. Studies show that when families have a plan and naloxone on hand, they reverse overdoses correctly 93% of the time. Without it, people wait an average of 6 to 8 minutes before calling for help. That’s often too long.
Step 1: Know Who’s at Risk
Start by listing everyone in your household who takes any medication that could cause an overdose. This includes:- Opioids (oxycodone, hydrocodone, morphine, tramadol)
- Benzodiazepines (alprazolam, diazepam, clonazepam)
- Sleep aids (zolpidem)
- Any medication taken with alcohol or other drugs
If someone is on more than 50 morphine milligram equivalents (MME) per day, the CDC says they’re at high risk. Even if they’re not on opioids, mixing medications increases danger. Don’t assume someone is safe just because they’re "taking it as prescribed." Tolerance changes. Pills get mixed up. People forget what they took.
Step 2: Get Naloxone - and Keep It Accessible
Naloxone (brand names Narcan, Kloxxado, or generic nasal spray) is the only drug that can reverse an opioid overdose. It’s safe. It won’t harm someone who didn’t take opioids. It’s not addictive. And in every U.S. state, you can get it without a prescription at pharmacies.Buy two or three nasal spray kits. Fentanyl is so potent that one dose may not be enough. Store them where everyone can reach them - not locked in a cabinet, not buried in a drawer. A hook by the front door, a drawer in the kitchen, a purse - just make sure every adult and teen in the house knows exactly where they are. Keep them at room temperature, away from sunlight. Check the expiration date every 18 months. Most kits last two years, but heat and light can ruin them faster.
Cost? Many pharmacies sell generic naloxone for $25 or less with insurance. Some CVS, Walgreens, and local health departments give them out for free. In Bristol, you can pick one up at the Southmead Health Centre or through the Bristol Drug and Alcohol Service.
Step 3: Learn the Signs of Overdose
An overdose doesn’t always look like a movie. People don’t always collapse dramatically. Look for these three signs:- Unresponsive: Shake their shoulders hard. Yell their name. If they don’t wake up, it’s an emergency.
- Slow or stopped breathing: Count breaths for 15 seconds. If they take fewer than 4 breaths, they’re in danger. Lips or fingernails turning blue or gray is a late sign - don’t wait for it.
- Pinpoint pupils: Shine a light in their eye. If the black center is tiny like a pinprick, it’s a strong indicator of opioid overdose.
Don’t mistake it for sleep. If someone is unusually hard to wake, especially after taking meds, assume it’s an overdose. Time is everything.

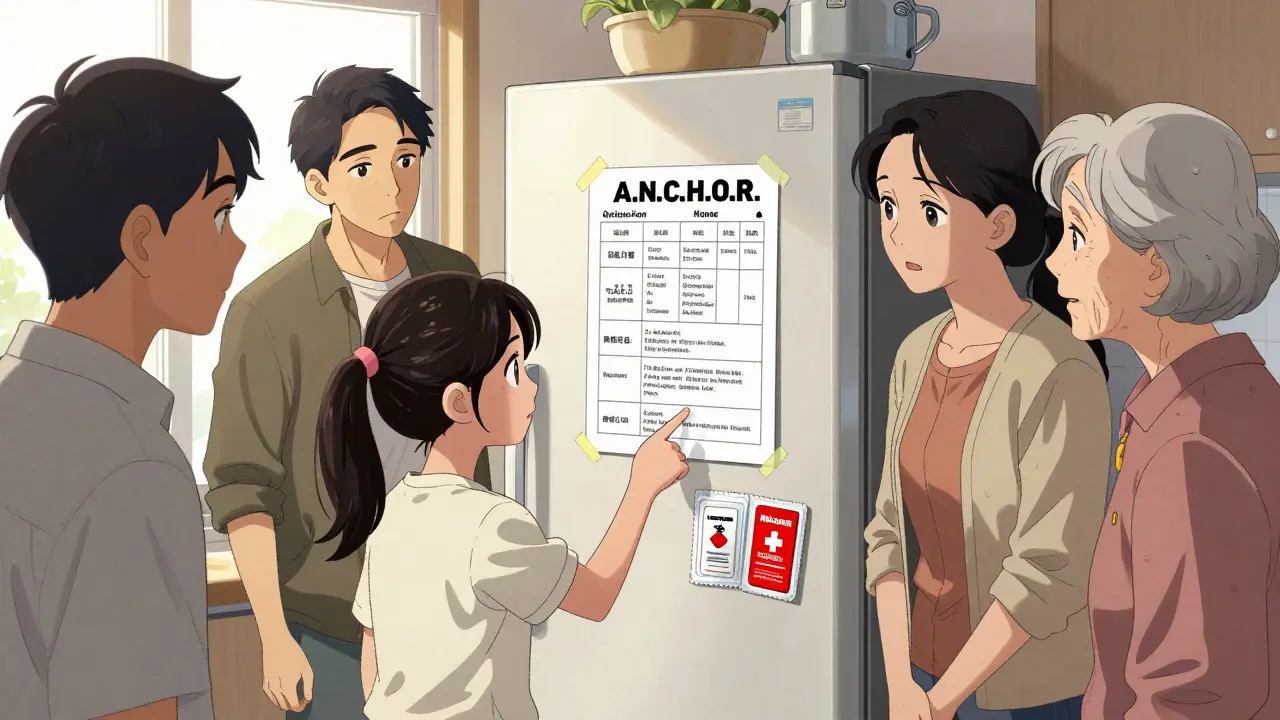
Step 4: Create Your Action Plan
Write down a simple sequence. Laminate it. Put it on the fridge. Teach it to everyone in the house. Use the A.N.C.H.O.R. method:- Assess: Check for responsiveness and breathing. If they’re not waking up and breathing too slowly, act immediately.
- Naloxone: Spray one dose into one nostril. Don’t wait for EMS. Don’t call 911 first. Give naloxone now.
- Call 911: After giving naloxone, call emergency services. Say: "I gave naloxone for a suspected opioid overdose. They’re not breathing." Stay on the line.
- Have more ready: If they don’t wake up in 3 minutes, give a second dose in the other nostril. Keep the second kit open and ready.
- Observe: Even if they wake up, stay with them. Naloxone wears off in 30 to 90 minutes. The overdose can come back. Keep them awake and breathing until help arrives.
- Review: After the emergency, talk as a family. What worked? What didn’t? Update your plan.
Step 5: Train Everyone - Even Teens
You can’t rely on one person to be the "responder." If the parent is unconscious, who acts? A 16-year-old might be the first person on the scene. That’s why training isn’t optional.Watch a 15-minute video from the American Red Cross. Do a practice run with a training kit (they’re free online). Practice spraying into an orange. Time how long it takes to find the kit and give the dose. If it takes more than 30 seconds, you’re not ready.
Teach teens how to use it. Don’t avoid the conversation because it’s uncomfortable. Say it plainly: "If someone stops breathing in this house, we use this spray. It saves lives. You might be the one who has to do it. I’m proud you’re ready."
What to Do After the Emergency
Even if naloxone works, the person needs medical care. Overdose can cause lung damage, brain injury, or a return of symptoms hours later. Never assume they’re fine just because they woke up.After the emergency, talk to a doctor. Ask about tapering opioids, switching to safer pain meds, or connecting with addiction services. Most people who survive an overdose with naloxone go on to get treatment - 89% do, according to SAMHSA. This isn’t the end. It’s a turning point.

Common Mistakes and How to Avoid Them
- Expired naloxone: 31% of failed attempts involved old kits. Set a calendar reminder every 18 months.
- Wrong administration: 24% of people sprayed into the wrong nostril or didn’t push the plunger fully. Practice with a trainer.
- Waiting too long: 63% of preventable deaths involved delays in calling 911. Give naloxone first, then call.
- Keeping it locked up: If you can’t reach it in 10 seconds, it’s useless. Keep it visible and accessible.
- Thinking it’s not your problem: 78% of U.S. households have at least one prescription medication. Only 12% have a plan. You’re not alone - but you’re also not safe unless you act.
Resources You Can Use Right Now
- Free naloxone: Visit naloxonefinder.org to find free kits near you.
- Training videos: The American Red Cross offers a free 15-minute online course.
- Local help: In Bristol, contact the Bristol Drug and Alcohol Service for free kits and training.
- Wallet card: Make a laminated card with names of people on meds, dosages, prescribing doctors, and emergency contacts. Keep it in your wallet or phone case.
Creating this plan takes two hours. It could save a life tomorrow. Don’t wait for a crisis to start preparing.
Can I give naloxone to someone who didn’t take opioids?
Yes. Naloxone only works on opioids. If someone didn’t take them, it won’t hurt them. It won’t wake them up if they’re asleep from alcohol or another drug - but it won’t make things worse either. If you’re unsure, give it anyway. It’s safe.
Is naloxone legal in the UK?
Naloxone is available in the UK as a pharmacy-only medicine. You can get it without a prescription at most pharmacies, including in Bristol. Pharmacists can provide training and kits. While the U.S. has more widespread access, the UK’s NHS and local drug services also distribute naloxone to at-risk households and families.
What if I’m afraid to call 911 because of legal trouble?
In the U.S., all 50 states have Good Samaritan laws that protect people who call for help during an overdose. You won’t be arrested for possessing drugs if you’re seeking help. In the UK, emergency services prioritize saving lives over legal consequences. Calling 911 is the right thing to do - and you’re protected.
Can I use naloxone on a child?
Yes. Naloxone is safe for children and teens. The dose is the same regardless of age - one nasal spray (4mg) per dose. If the child is under 12 and still not breathing after the first dose, give a second dose. Always call 911 after.
How often should I refresh the plan?
Review your plan every 6 months. Check expiration dates on naloxone kits. Re-train everyone in the house - even if they’ve done it before. Skills fade. Stress changes how people react. A 10-minute family check-in every few months keeps everyone ready.
What if I don’t have insurance?
You don’t need insurance to get naloxone. Many pharmacies sell it for under $25. Free kits are available through local health departments, harm reduction programs, and pharmacies like CVS and Walgreens. In Bristol, contact your local council or NHS pharmacy - they often provide free kits to residents.
Next Steps
If you have opioids or other high-risk meds in your home:- Order two naloxone kits today.
- Watch the Red Cross video before bedtime.
- Put one kit where you sleep, one where you cook.
- Have a 10-minute family talk this week: "What would we do if someone stopped breathing?"
You don’t need to be a doctor. You don’t need to be perfect. You just need to be ready. One plan. Two doses. One conversation. That’s all it takes to turn panic into action - and maybe, just maybe, to save someone you love.






Ayush Pareek January 15, 2026
This is the kind of post that should be shared everywhere. I’m from India, and we don’t talk about this enough - even when people are on painkillers after surgery or elderly parents mix meds without knowing the risks. I’ve seen it happen. A simple plan, a nasal spray within reach, and a family that knows what to do - that’s all it takes. No heroics. Just preparation.
Thanks for laying it out so clearly. I’m printing this and posting it on our fridge tonight.
Diane Hendriks January 16, 2026
Let’s be honest - this isn’t about harm reduction. It’s about enabling. The real problem is the normalization of pharmaceutical dependency in this country. You hand out naloxone like candy and people think they’re invincible. Why not focus on stopping the overprescribing in the first place? Instead of training teens to revive their parents, why not teach them to say no to pills handed out like candy by doctors who don’t even know their patients’ names?
This isn’t prevention. It’s damage control for a broken system.
Annie Choi January 17, 2026
YESSSS. This is the blueprint. Naloxone isn’t a last resort - it’s a first line of defense. I’ve trained my whole household - including my 14-year-old - and we do a 60-second drill every time we do laundry. Practice makes panic-proof.
Pro tip: Buy the 8mg kits. Fentanyl’s not playing. And keep one in your car. You never know when you’ll be the first responder at a gas station parking lot.
Also - if you’re still hiding it in the medicine cabinet? You’re not ready. You’re just pretending.
Go get yours. Now. I’ll wait.
Arjun Seth January 17, 2026
Why are we even doing this? People who OD are just lazy. They don’t care. They take drugs because they’re weak. Why waste money and time on people who choose to destroy themselves? If they didn’t take the pills, they wouldn’t need saving. This plan is just giving them a safety net so they can keep doing it. No. Just no.
My cousin died from an overdose. He was 23. He had a job. He had a family. But he still chose to get high. This isn’t prevention - it’s enabling.
Dan Mack January 18, 2026
EVERYTHING is a government scam. Naloxone? It’s not to save lives - it’s to keep the opioid pipeline flowing. The CDC, the FDA, the pharmacies - they’re all in on it. They want you dependent. They want you coming back. That’s why they make it so easy to get. That’s why they push this ‘plan’ nonsense. It’s not about saving you - it’s about keeping you in the system.
And don’t even get me started on the ‘Good Samaritan’ laws. That’s just another trap. They record your voice. They track your IP when you call 911. You think you’re protected? You’re being cataloged.
Don’t trust the plan. Trust your gut. And keep your meds locked up. Always.
Amy Vickberg January 20, 2026
Arjun, I hear you - but this isn’t about judgment. It’s about love. My brother took a mislabeled pill at a party. He didn’t know it was fentanyl. He wasn’t using. He was just trying to feel okay after a bad day. Naloxone saved him. He’s been clean for two years now.
This isn’t about enabling. It’s about giving people a second chance - not because they deserve it, but because we’re human. And sometimes, the person who needs saving is the one you never expected.
Just… please don’t assume you know the whole story.
Nishant Garg January 20, 2026
From Delhi to Detroit - this is the same story. In India, grandmas mix painkillers with Ayurvedic tonics. In the States, teens grab pills from Mom’s nightstand. The drugs change. The fear doesn’t.
I showed this to my family last night. We laughed. Then we cried. Then we put one naloxone kit by the TV, one by the kitchen sink, and one in my sister’s backpack. My 70-year-old dad said, ‘I didn’t know I could save a life with this.’ He’s now the one reminding us to check expiration dates.
It’s not about politics. It’s about who’s in the room with you when the silence comes. That’s the moment that matters.
Thank you for writing this. Not just for me - for everyone who didn’t know they needed it.
Nicholas Urmaza January 21, 2026
Professional recommendation: This plan is clinically sound and operationally viable. The A.N.C.H.O.R. protocol aligns with CDC and WHO guidelines for community-based overdose response. The emphasis on accessibility, repetition, and multi-user training significantly increases survival probability.
Organizations should adopt this model as a standard for household risk mitigation. Training modules should be integrated into primary care visits, school curricula, and workplace wellness programs.
Implementation is not optional. It is a public health imperative.
Do not delay.
Nilesh Khedekar January 22, 2026
Wow. A whole 10-page essay on how to save someone who probably shouldn’t have been given the pills in the first place. Brilliant. Let’s just hand out naloxone like free samples at a Costco. Next thing you know, we’ll be having ‘Narcan Bingo’ at family reunions.
Meanwhile, in India, we just tell people: ‘Don’t take pills you don’t understand.’ Radical, I know.
But hey - at least you’re not the one cleaning up the mess when the 16-year-old wakes up confused and asks, ‘Why did you save me?’
Just saying. Maybe the real problem isn’t the lack of spray… it’s the lack of boundaries.