Missing a few pills here and there might seem harmless-but for someone managing diabetes, high blood pressure, or heart failure, it’s not. Non-adherence to medication is one of the biggest silent killers in modern healthcare. It leads to avoidable hospital visits, worsening conditions, and costs the U.S. system over $300 billion every year. The problem isn’t always forgetfulness. It’s often that the plan doesn’t fit the person’s life. That’s where achievable adherence goals come in-not just telling someone to take their medicine, but helping them build a real, trackable habit that sticks.
Why Most Medication Plans Fail
You’ve probably heard the advice: "Take your pills every day." Simple, right? But if you’re working two jobs, can’t afford co-pays, or get dizzy when you stand up too fast, that instruction doesn’t help. Studies show that up to 50% of patients with chronic illnesses don’t take their meds as prescribed. And when doctors ask, patients often say they’re doing fine-because they don’t want to disappoint them. Self-reporting overstates adherence by 30-40%. That’s why tracking matters more than ever.What Makes a Goal Actually Achievable?
Forget vague promises like "I’ll take my meds better." Real progress starts with structure. The SMART framework-Specific, Measurable, Achievable, Relevant, Time-bound-isn’t just corporate jargon. It’s been proven in clinics across the country to boost adherence by up to 35%. Here’s how to make it work for real people:- Specific: Instead of "take my blood pressure pill," say: "I will take my 10mg lisinopril every morning after brushing my teeth, at the kitchen table, to keep my BP under control so I can play with my grandkids without getting winded."
- Measurable: How will you know you did it? Use pill counts, smartphone apps like Medisafe, or smart bottles that log when they’re opened. Electronic monitoring is 98% accurate-way better than memory.
- Achievable: If someone works nights, don’t set a 7 a.m. pill time. Adjust it to after their evening meal. If they can’t afford the full prescription, work with their pharmacist on a 7-day starter pack.
- Relevant: Connect the goal to what the patient cares about. Not "this reduces your HbA1c," but "this helps you walk to the store without stopping to catch your breath."
- Time-bound: "This week, I’ll take all my pills on time." Not "next month," not "soon." A week is a good starting point. Too long, and motivation fades.
Some clinics now use B-SMART-adding "Barriers" as the first step. Before setting any goal, ask: What’s stopping you? Transportation? Cost? Confusion about instructions? Fear of side effects? If the answer is "I can’t afford it," then the goal isn’t about adherence-it’s about access. Fix that first.
How to Track Progress Without Overwhelming the Patient
Tracking doesn’t mean logging every single pill in a notebook. It means finding the easiest, most natural way to see progress. Here’s what works:- Smart pill bottles: Devices like AdhereTech or Hero track when the bottle opens. No app needed. Just plug it in. Data syncs to the provider’s EHR.
- Pharmacy refill records: Your doctor can check your Medication Possession Ratio (MPR). If you refill your statin every 28 days, you’re likely taking it. If you wait 60 days? Red flag.
- Digital biomarkers: For diabetes, continuous glucose monitors show patterns. If glucose spikes every Tuesday, maybe you skipped your metformin that weekend.
- Wearables: Fitbit or Apple Watch users who link their medication reminders to daily step goals see 29% better adherence. Movement and meds become part of the same routine.
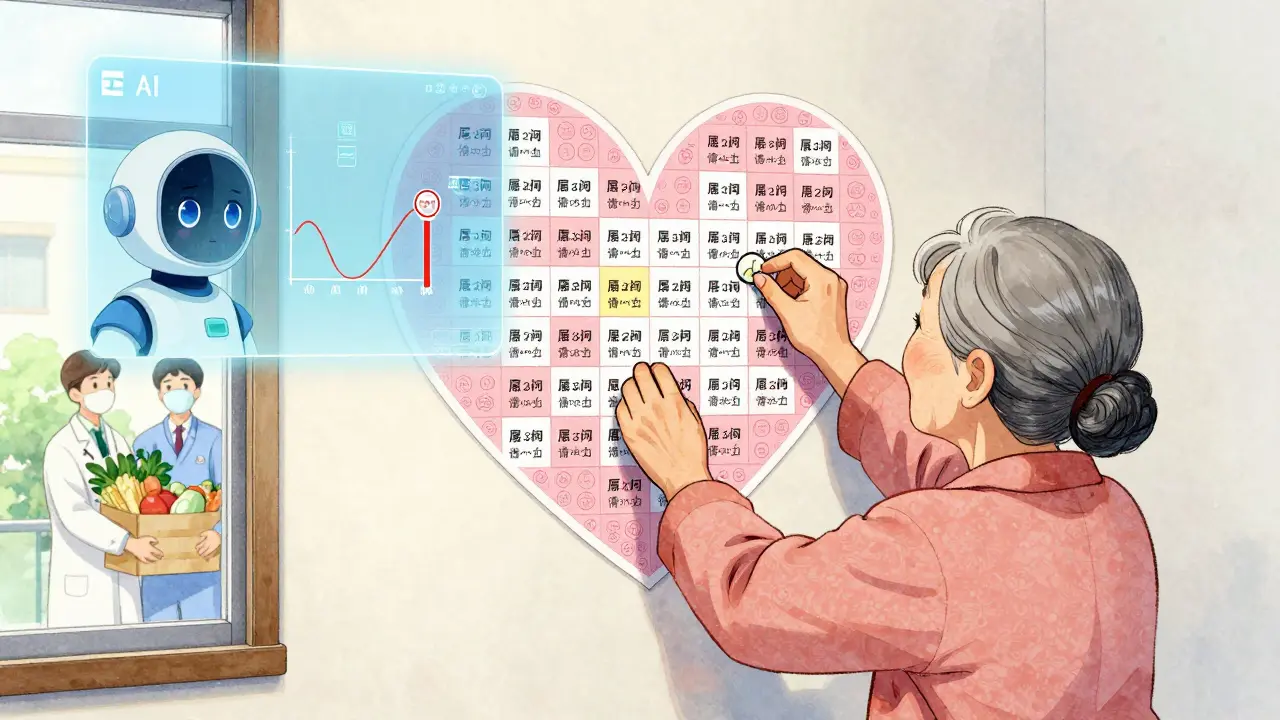
Visual progress matters. A patientBetter survey found 78% of patients prefer charts and stickers over text messages. One diabetes educator used a simple sticker chart: every time Mrs. Johnson weighed in, she got a sticker. After five stickers, she got a small reward-a new pair of walking shoes. Her weigh-ins jumped from twice a week to five. Small wins build momentum.

Tools That Actually Help (And Which Ones to Avoid)
There are hundreds of apps claiming to improve adherence. Most fail because they’re too complicated or don’t connect to real life. Here’s what’s working in 2026:| Tool | Accuracy | Best For | Downsides |
|---|---|---|---|
| Smart pill bottles (AdhereTech, Hero) | 98% | Older adults, those with memory issues | Requires Wi-Fi, upfront cost |
| Medisafe app | 92% (self-reported) | Younger adults, tech-savvy users | Requires phone, can be ignored |
| NovoPen Echo (insulin pens) | 99.2% | Diabetes patients | Only works with specific insulin |
| Propeller Health (asthma inhalers) | 95% | Asthma/COPD patients | Needs Bluetooth, limited to respiratory meds |
| Pharmacy refill data | 85% | Providers, clinics without tech budget | Delayed-only shows after refill, not real-time |
Don’t force digital tools on someone who doesn’t use smartphones. For older adults, a simple pill organizer with alarms or a weekly call from a family member often works better than an app. The goal isn’t tech-it’s consistency.
What Providers Need to Do Differently
Doctors and nurses aren’t failing patients-they’re overwhelmed. A typical 15-minute visit doesn’t leave room to unpack why someone isn’t taking their meds. Here’s what helps:- Use motivational interviewing: Ask open questions. "What’s been hard about taking your pills?" not "Why aren’t you taking them?"
- Use EHR templates. Systems like Epic and Cerner now have built-in SMART goal fields. No more typing free text-just pick from dropdowns: barrier type, metric, deadline.
- Start small. One goal per visit. Not five. If they nail one, celebrate it. Then add another next time.
- Automate reminders. Systems that send automated texts or calls when a goal is missed improve follow-through by 41%.
Providers who use structured goal tracking report 63% less variability in documentation. That means better coordination, fewer errors, and more time for actual care.
When SMART Goals Don’t Work (And What to Do Instead)
SMART goals aren’t magic. They don’t fix poverty, lack of transportation, or untreated depression. If a patient can’t afford their insulin, no amount of goal-setting will help. In those cases:- Connect them to patient assistance programs. Many drugmakers offer free or low-cost meds.
- Work with community health workers. They can help with rides, food access, or translating instructions.
- Adjust the goal. Instead of "take all meds daily," try "take your BP pill 4 out of 7 days this week." Progress isn’t all-or-nothing.
Patients with cognitive decline or severe mental illness may need simpler systems: color-coded pill boxes, caregiver involvement, or even weekly medication delivery. The goal isn’t perfection-it’s safety.
The Bigger Picture: Why This Matters Now
In 2024, Medicare and Medicaid started tying reimbursement to adherence metrics for 12 chronic conditions. Hospitals get paid more when patients stay out of the ER. That’s why 62% of big health systems now use digital tracking tools. But independent clinics? Only 28% have them. That gap is widening.And it’s getting worse. Patients on Medicaid are 23% less likely to meet SMART goals-not because they’re less motivated, but because they face more barriers: food insecurity, unstable housing, no reliable internet. New "adaptable SMART" frameworks are being rolled out in 2025 to adjust goals based on ZIP code resources. If you live in a food desert, your nutrition goal might be "eat one vegetable per day" instead of "follow a DASH diet."
The future is AI. Tools like ThoroughCare’s 2023 analytics can predict 89% of adherence failures 14 days before they happen. Voice-activated trackers like Amazon Halo are testing well in pilot programs. Ingestible sensors that send signals when swallowed are approved by the FDA. But none of this matters if the patient doesn’t trust the system-or if the provider doesn’t know how to use it.
Start Here: Your First Adherence Goal
You don’t need fancy tech. You don’t need a 30-minute counseling session. Just do this:- Choose one medication that’s most important to your health right now.
- Ask: What’s one thing that makes it hard to take this pill? (Cost? Side effects? Forgetting?)
- Set a tiny goal: "I will take this pill every day for the next 7 days, right after I eat breakfast."
- Use something you already do: a phone alarm, a sticky note on the mirror, a pill box with days of the week.
- At the end of the week, check in. Did you do it? If yes, celebrate. If not, figure out why-and adjust.
Adherence isn’t about willpower. It’s about design. The right system turns a chore into a habit. And habits, not guilt, are what keep people healthy.
What’s the most common mistake people make when setting medication goals?
The biggest mistake is setting goals that are too broad or unrealistic. Saying "I’ll take all my meds every day" doesn’t help. You need to be specific: which pill, when, how, and why. Also, many people skip the "achievable" part. If you work two shifts, don’t set a 7 a.m. pill time. Adjust it to fit your life.
Can I track my medication adherence without an app?
Absolutely. Many people do. Use a pill organizer with compartments for each day. Mark off days on a calendar. Set a daily alarm on a basic phone. Ask a family member to check in. Even a simple checklist taped to the fridge works better than nothing. Tech helps, but it’s not required.
How do I know if my goal is working?
Look for two things: consistency and outcomes. Are you taking your pills on schedule? And are your health numbers improving? For example, if you’re on blood pressure meds, check your readings weekly. If your HbA1c drops after 3 months of consistent use, your goal is working. If not, talk to your provider-maybe the goal needs tweaking.
What if I miss a dose? Does that mean I failed?
No. Missing one dose doesn’t mean you failed. It means you’re human. The goal isn’t perfection-it’s progress. If you miss a dose, don’t panic. Just take it as soon as you remember (unless the instructions say not to). Then, figure out why it happened. Was it a change in routine? A new side effect? Use that insight to adjust your next goal.
Are SMART goals only for older adults with chronic illness?
No. SMART goals work for anyone taking long-term medication-whether you’re 25 with asthma, 40 with depression, or 65 with heart disease. The key is tailoring the goal to your life. A college student might set a goal around taking their ADHD med before class. A new parent might link their blood pressure med to feeding their baby. It’s not about age-it’s about fit.
Can my doctor help me set these goals?
Yes-and they should. But many don’t know how. Ask your provider: "Can we set one small, specific goal for my medication this visit?" If they’re unfamiliar with SMART goals, suggest they look into the B-SMART model, which starts by identifying barriers. Most clinics now have templates built into their electronic records. It’s becoming standard.
Next Steps: What to Do Today
If you’re managing a chronic condition and struggling with adherence:- Choose one medication you want to improve.
- Write down the one biggest barrier keeping you from taking it.
- Set a 7-day SMART goal using the framework above.
- Use one simple tracking method-phone alarm, pill box, or calendar check.
- At the end of the week, reflect: Did you meet your goal? Why or why not?
If you’re a provider:
- Use your EHR’s built-in SMART goal template-don’t type free text.
- Ask one open-ended question about adherence in every visit.
- Offer at least one low-tech tracking option for patients without smartphones.
- Celebrate small wins. A quick "You did it!" goes further than a lecture.
Adherence isn’t about compliance. It’s about connection. When people feel heard, supported, and given tools that match their lives, they don’t just take their pills-they take control of their health.







Angela Stanton January 7, 2026
Okay but let’s be real - most of these ‘SMART goals’ are just corporate wellness fluff dressed up as clinical innovation. 98% accuracy? With smart bottles? 😂 Most of my grandma’s generation can’t even figure out how to turn on the TV, let alone sync a Wi-Fi-enabled pill dispenser. And don’t get me started on ‘digital biomarkers’ - if your glucose monitor is spiking because you skipped metformin, congrats, you’re now a data point. Not a person. 📊🩸
Johanna Baxter January 8, 2026
I took my blood pressure meds for 3 days then stopped because my doctor didn’t ask how I was FEELING just if I was taking them. Like I’m a robot. 😭 I cried in the pharmacy parking lot. I just wanted someone to say ‘this sucks, I’m sorry.’ Not a checklist.
Jeffrey Hu January 10, 2026
Actually, the 50% non-adherence stat is misleading. It conflates intentional non-adherence (like skipping meds due to cost) with forgetfulness. The real issue isn’t goal-setting - it’s systemic underfunding. You can’t ‘SMART’ your way out of a $600 insulin bill. The article ignores socioeconomic determinants entirely. This is like telling someone to ‘eat healthy’ while living in a food desert. 🤦♂️
Jacob Paterson January 11, 2026
Wow. Another ‘let’s track everything with tech’ fantasy. So now we’re gonna monitor your pill bottle opening like it’s a prison cell? Next thing you know, your Fitbit’s gonna report your ‘medication compliance score’ to your employer. This isn’t healthcare. It’s surveillance capitalism with a stethoscope. 💊👁️
Kiruthiga Udayakumar January 11, 2026
As someone from India, I’ve seen this firsthand. My aunt takes her pills only when the doctor visits - because that’s the only time someone cares. No apps. No smart bottles. Just fear of being scolded. We need community health workers, not tech. Tech is a luxury. Survival is not. 🇮🇳
Patty Walters January 12, 2026
i used a pill organizer with days of the week and stuck it next to my coffee maker. every morning i’d pour my coffee, pop the pills, and boom - habit. no app needed. no guilt. just coffee and consistency. also, i stopped caring about perfection. missed one? okay. tomorrow’s a new day. 🫖💊
Phil Kemling January 12, 2026
What’s fascinating here is the implicit assumption that adherence is a personal failure. But what if it’s a systemic one? We ask individuals to optimize their behavior while ignoring the structures that make it impossible - unstable housing, wage theft, mental health neglect. The ‘design’ isn’t broken - the system is. And until we fix that, no sticker chart will save us. 🌍
tali murah January 12, 2026
Let’s not romanticize ‘simple solutions.’ A sticker chart? For diabetes? That’s like handing a drowning person a rubber duck. This article is a masterclass in performative empathy - rich with buzzwords, empty of structural accountability. If you’re not addressing access, you’re not helping. You’re just curating a TED Talk. 🎤📉
Jenci Spradlin January 14, 2026
my dad used a pillbox with big letters and a wind-up alarm clock. every day at 8am, that thing went off like a fire drill. he’d grumble, take his meds, and go back to bed. no smartphone. no app. just a dumb clock and a man who refused to die before his grandkids graduated. sometimes the tech is just… a person who cares.
Catherine Scutt January 15, 2026
if you’re telling someone to take their meds after brushing their teeth but they don’t even have a toothbrush, what’s the point? this whole thing feels like blaming the victim for not having a fancy kitchen. real talk: if you can’t afford food, you’re not gonna prioritize a pill you don’t understand.
Darren McGuff January 17, 2026
Interesting how the article completely ignores the role of polypharmacy. I’m on 11 medications. Trying to ‘SMART’ that is like juggling chainsaws while riding a unicycle. The real solution isn’t tracking - it’s deprescribing. Less is more. Always has been. 🤔
Alicia Hasö January 19, 2026
You’re not alone. I’ve seen patients transform with just one small win - a weekly call from a volunteer, a sticker on the fridge, a ‘you did it!’ text. It’s not about tech. It’s about being seen. When someone says, ‘I noticed you took your meds all week,’ it changes everything. That’s the real magic. 💛
Ashley Kronenwetter January 19, 2026
While the framework is sound, the implementation assumes a level of health literacy and digital access that is not universal. For patients with low literacy, even a ‘simple’ pill organizer can be overwhelming. We must prioritize universal design principles - visual cues, audio prompts, caregiver integration - before deploying any ‘innovation.’
Aron Veldhuizen January 19, 2026
So let me get this straight - we’re celebrating a 35% improvement in adherence through SMART goals… but the baseline was 50% non-adherence? That means we’re still failing 65% of people. Is this really progress? Or just a statistical illusion designed to make hospitals look good on their quarterly reports? 🤨