When your body stops making insulin, life changes fast. Type 1 diabetes doesn’t wait for a warning. One day you’re tired all the time, drinking water nonstop, and losing weight even though you’re eating more. The next, you’re in the hospital fighting diabetic ketoacidosis. There’s no slow build-up here-this hits hard and fast. And if you’re reading this, chances are you or someone you care about is facing it head-on.
What Actually Happens in Type 1 Diabetes?
Type 1 diabetes isn’t caused by sugar or laziness. It’s an autoimmune disease. Your immune system, which normally fights off viruses and bacteria, turns on your own pancreas. It destroys the beta cells that make insulin-the hormone your body needs to turn sugar from food into energy. Without insulin, glucose piles up in your blood. Your cells starve. Your body starts breaking down fat for fuel, producing toxic acids called ketones. That’s when things get dangerous.
This isn’t rare. Around 1.6 million Americans live with type 1 diabetes, and it’s growing. About 5 to 10% of all diabetes cases are type 1. It often shows up in kids and teens, but nearly half of all diagnoses happen in adults. You can get it at 5 or at 50. There’s no cure yet. But with the right tools, you can live well.
Classic Symptoms You Can’t Ignore
The signs of type 1 diabetes don’t whisper-they shout.
- Polyuria: You’re peeing every hour. Not because you drank too much coffee-because your kidneys are trying to flush out the sugar flooding your blood.
- Polydipsia: You’re constantly thirsty. No matter how much water you drink, it’s never enough. Your body’s desperate to replace the fluids lost through urine.
- Unintentional weight loss: You’re losing pounds even if you’re eating normally. Your body’s burning muscle and fat because it can’t use glucose for energy.
- Extreme fatigue: You feel like you’ve run a marathon just by getting out of bed. Your cells are starving.
- Blurred vision: High blood sugar swells the lenses in your eyes. Things go fuzzy. It’s temporary-but it’s a red flag.
- Slow-healing cuts: High glucose slows circulation and weakens your immune response. A small scrape takes weeks to close.
- Extreme hunger: You’re eating more but losing weight. Your body can’t use the food you’re swallowing.
- Dry mouth and fruity-smelling breath: This is ketones building up. It smells like nail polish remover. If you notice this, don’t wait-go to the ER.
These symptoms don’t creep in over months. They show up in days or weeks. And if you miss them, diabetic ketoacidosis (DKA) can hit in under 24 hours. DKA is life-threatening. It’s not something you can treat at home. If you’re vomiting, confused, breathing fast, or smell fruity, call 999 or go to A&E immediately.
How Doctors Diagnose Type 1 Diabetes
Diagnosis isn’t just about symptoms. It’s about numbers. Blood tests tell the real story.
The A1C test measures your average blood sugar over the past 2 to 3 months. If it’s 6.5% or higher on two separate tests, you have diabetes. But A1C alone doesn’t tell you if it’s type 1 or type 2. That’s where autoantibody tests come in.
GAD65 antibodies are the first test doctors order. If they’re present, it’s almost certainly type 1. If not, they’ll check for IA2 or ZNT8 antibodies. These are the body’s fingerprints of autoimmune attack.
C-peptide is another key test. It shows how much insulin your body is still making. In type 1, C-peptide is low-even when blood sugar is sky-high. In type 2, it’s high because the body’s still making insulin, just not using it well.
Other tests include:
- Fasting plasma glucose: 126 mg/dL (7.0 mmol/L) or higher after 8+ hours without food.
- Random plasma glucose: 200 mg/dL (11.1 mmol/L) or higher, especially if you have symptoms.
- Oral glucose tolerance test: Blood sugar of 200 mg/dL or higher two hours after drinking a sugary solution.
If DKA is suspected, doctors check blood pH, bicarbonate, and ketones in blood or urine. A pH below 7.3 and ketones above 3.0 mmol/L mean emergency treatment is needed.

Insulin Therapy: The Lifeline
You can’t survive without insulin. But how you get it has changed dramatically.
Multiple Daily Injections (MDI), also called basal-bolus therapy, is still the most common method. You take a long-acting insulin once or twice a day to cover your baseline needs (basal). Then you take rapid-acting insulin before meals to handle the sugar from food (bolus). Common basal insulins include glargine (Lantus), detemir (Levemir), and degludec (Tresiba). Rapid-acting ones are lispro (Humalog), aspart (NovoRapid), and glulisine (Apidra).
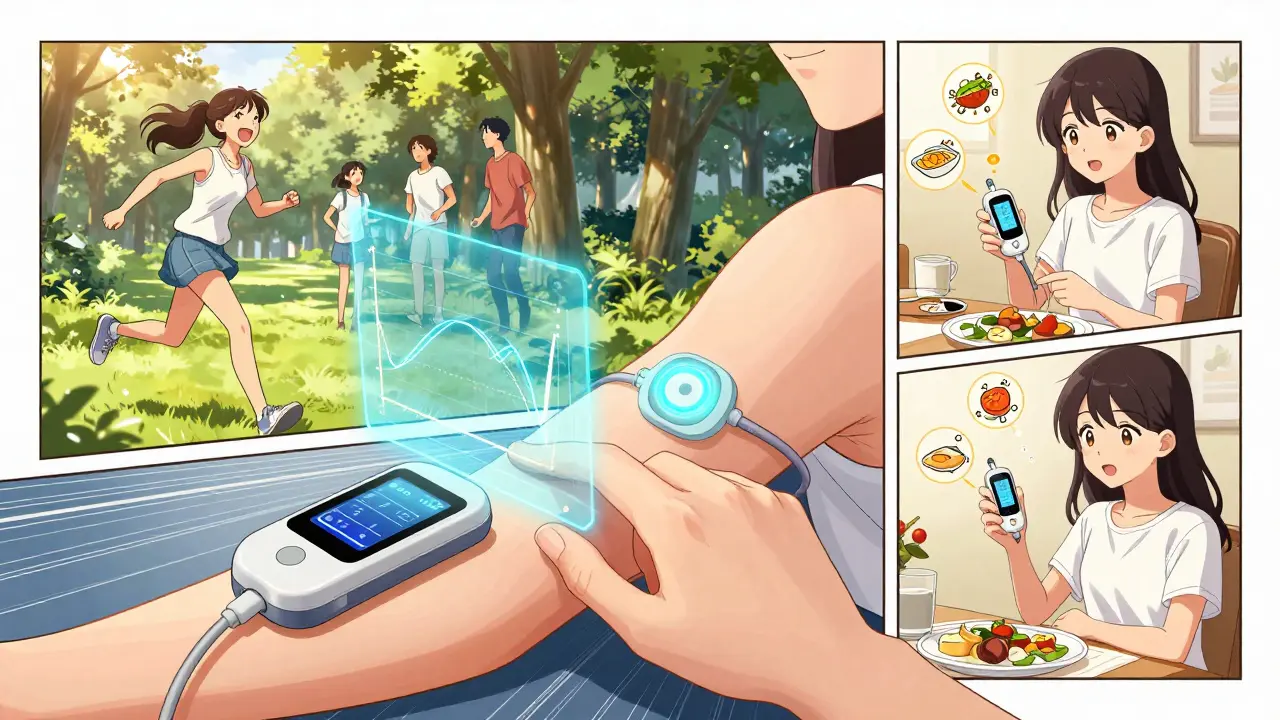
Insulin pumps deliver rapid-acting insulin through a tiny tube under your skin. You wear it 24/7. Modern pumps don’t just deliver insulin-they talk to your continuous glucose monitor (CGM). Systems like Medtronic’s MiniMed 780G and Tandem’s t:slim X2 with Control-IQ can automatically adjust insulin doses based on your glucose trends. No more guessing. No more fingersticks every hour.
These hybrid closed-loop systems have changed everything. Studies show they boost time-in-range-from 50% to 70-75% of the day spent between 70 and 180 mg/dL. That means fewer highs, fewer lows, and less brain fog.
What Good Control Looks Like
The American Diabetes Association recommends these targets for most adults:
- Before meals: 80-130 mg/dL (4.44-7.22 mmol/L)
- Two hours after meals: Under 180 mg/dL (10.0 mmol/L)
- A1C: Under 7% (53 mmol/mol)
But these aren’t one-size-fits-all. If you’re older, have heart disease, or get frequent lows, your doctor might aim for 7.5% or even 8%. The goal isn’t perfection-it’s safety and sustainability.
Testing frequency matters too. If you’re on MDI, you’ll likely check your blood sugar 4 to 10 times a day. With a CGM, you get readings every 5 minutes. Sensors last 7 to 14 days. You still need to calibrate with a fingerstick occasionally, but you’re seeing trends, not just snapshots.
Managing the Daily Grind
Living with type 1 diabetes isn’t just about insulin. It’s a full-time job.
You’ll need to learn carbohydrate counting. Most people start with an insulin-to-carb ratio-like 1 unit for every 10 grams of carbs. But that changes. Your sensitivity shifts with stress, sleep, hormones, and exercise. A meal of pasta might need 4 units. A salad with chicken might need 1. You learn by trial and error.
Training takes time. Most diabetes education programs require 10 to 20 hours of instruction. You’ll learn carb counting, injection techniques, pump troubleshooting, sick-day rules, and how to treat low blood sugar.
Hypoglycemia is the daily fear. Below 70 mg/dL (3.9 mmol/L), you’re in danger. Symptoms: shaking, sweating, confusion, rapid heartbeat. Treat it fast: 15 grams of fast-acting sugar-glucose tablets, juice, or candy. Wait 15 minutes. Check again. Repeat if needed. Never drive or operate machinery until you’re stable.
People with type 1 diabetes spend 2 to 4 hours a day managing their condition. That’s more than most jobs. It’s exhausting. But you’re not alone.
What’s New? Hope on the Horizon
There’s real progress. In late 2022, the FDA approved teplizumab (Tzield). It’s not a cure-but it’s the first drug that can delay type 1 diabetes in high-risk people. Given as a 14-day IV infusion, it delayed diagnosis by nearly two years in clinical trials. This is for people with stage 2 diabetes-those with autoantibodies but normal blood sugar. It’s a game-changer for families.
Stem cell therapies are coming fast. Vertex Pharmaceuticals’ VX-880 therapy replaces destroyed beta cells with lab-grown ones. In early 2023 trials, 89% of participants stopped needing insulin after 90 days. It’s still experimental, but the results are stunning.
Insulin costs are still brutal. The average person with type 1 spends $20,773 a year on care. Insulin alone makes up 27% of that. In the UK, insulin is free on the NHS-but supplies can be inconsistent. In the US, many still ration insulin. That’s not just a health issue-it’s a human rights crisis.
What Comes Next?
Type 1 diabetes doesn’t go away. But it doesn’t have to control you. With modern tools, you can run marathons, have kids, travel the world, and work full-time. You’ll need discipline. You’ll need support. You’ll need to learn how to talk to your body.
Start with your doctor. Get tested if symptoms match. Learn your insulin. Get a CGM if you can. Join a support group. Read the latest from the American Diabetes Association. You’re not just surviving-you’re adapting. And that’s powerful.
Can type 1 diabetes be cured?
No, there is no cure yet. Type 1 diabetes is a lifelong condition caused by the immune system destroying insulin-producing cells. But new treatments like teplizumab can delay onset in high-risk people, and stem cell therapies like VX-880 have shown promise in restoring insulin production. Research is advancing quickly, but daily insulin therapy remains essential for now.
How is type 1 diabetes different from type 2?
Type 1 is autoimmune-you make little to no insulin. Type 2 is metabolic-you make insulin but your body doesn’t use it well. Type 1 usually starts suddenly in childhood or young adulthood. Type 2 develops slowly, often linked to weight and inactivity. Autoantibody and C-peptide tests confirm type 1. Type 2 is often managed with diet, pills, or GLP-1 agonists-type 1 always needs insulin.
Do I need to avoid sugar completely?
No. People with type 1 diabetes can eat sugar. The key is matching insulin to carbs. A chocolate bar? You’ll need more insulin. A salad? Less. It’s not about banning foods-it’s about balancing them. Carbohydrate counting and insulin-to-carb ratios let you enjoy treats safely. Avoiding sugar entirely isn’t necessary-and can make life harder than it needs to be.
Can I use an insulin pump instead of injections?
Yes, and many people prefer it. Insulin pumps deliver insulin continuously and can be paired with CGMs for automated adjustments. They reduce the number of daily injections and improve time-in-range. But they require training, maintenance, and a willingness to wear a device 24/7. Not everyone likes them-but for many, they’re life-changing.
What should I do if I miss a dose of insulin?
If you miss a basal (long-acting) insulin dose, contact your healthcare provider immediately. You may need a correction dose. If you miss a bolus (mealtime) insulin, check your blood sugar. If it’s high, give a correction dose based on your insulin sensitivity factor. Never double up on basal insulin without medical advice. Missing doses can lead to DKA within hours. Always have a sick-day plan ready.
Can children with type 1 diabetes live normal lives?
Absolutely. With proper management, children with type 1 diabetes play sports, go to school, sleep over at friends’ houses, and thrive. Modern tools like CGMs and insulin pumps make it easier than ever. Schools in the UK are legally required to support children with diabetes. The key is education-for the child, parents, teachers, and caregivers. Many kids grow up to become doctors, athletes, and artists-living full, active lives.
Is type 1 diabetes hereditary?
There’s a genetic link, but it’s not simple. If a parent has type 1, a child’s risk is about 2-5%. If both parents have it, the risk rises to 25-50%. But most people with type 1 have no family history. Environmental triggers-like viral infections-likely play a big role. You can’t prevent it through lifestyle. It’s not your fault.
How often should I get my A1C tested?
Every 3 months if your blood sugar isn’t stable or you’ve changed your treatment. If you’re doing well and your levels are steady, every 6 months is fine. A1C gives a bigger picture than daily readings. It shows whether your overall plan is working. Don’t skip these tests-they’re your roadmap to long-term health.
Final Thoughts
Type 1 diabetes is hard. It’s exhausting. It’s expensive. But it’s not a death sentence. With insulin, monitoring, and support, you can live fully. The tools are better than ever. The science is moving fast. You’re not just managing a disease-you’re mastering a system. And that takes strength. You’ve got this.








Katherine Blumhardt December 24, 2025
I just got diagnosed last month and I’m still trying to figure out how to not cry every time I prick my finger. This post helped more than my endo. Thanks.
Oluwatosin Ayodele December 25, 2025
You people act like type 1 is some tragedy. In Nigeria we don’t even have access to insulin half the time. You’re lucky you have CGMs. Stop complaining about 10 fingersticks a day.
Mussin Machhour December 26, 2025
Bro this is the most real thing I’ve read all year. I’ve been on the pump for 3 years and yeah it’s a pain but I ran a 5K last weekend and didn’t crash. You can do this.
Gary Hartung December 27, 2025
I mean... the fact that you’re even discussing 'insulin therapy options' as if there’s a spectrum of choice is frankly naive. The only real option is a fully closed-loop system paired with a CGM and a PhD in biochemistry. Anything less is just... sad.
Linda B. December 28, 2025
Teplizumab was approved in 2022... but did you know the FDA got pressured by Big Pharma to fast-track it? The real cure is being buried. They don’t want you to be healthy. They want you buying insulin forever.
Michael Dillon December 29, 2025
I’ve had T1D for 22 years and I still think people who use insulin pumps are just trying to look cool. I’ve got my syringes and my pride. And I’m still alive. You’re not special.
Bailey Adkison December 29, 2025
You say type 1 isn’t caused by sugar. That’s technically true. But let’s be honest: if your kid eats nothing but juice boxes and gummy worms for three years, their pancreas is gonna get confused. Blame the parents.
Lindsay Hensel December 30, 2025
To the person in Nigeria: I’m so sorry you’re facing that. I’ve seen insulin shortages in rural clinics in Texas. This isn’t just an American problem. We need global access. No one should choose between food and insulin.
Ben Harris January 1, 2026
I don’t know why anyone still uses MDI. It’s 2024. If you’re not on a hybrid closed-loop, you’re basically living in the 1990s. And yes, I’m judging you.
Carlos Narvaez January 1, 2026
Pump users are just addicted to tech. Real diabetics use pens. And they don’t need to tweet about it.
Sophie Stallkind January 2, 2026
The emotional toll of this disease is rarely discussed. The constant vigilance, the guilt over highs, the fear of lows-these are invisible burdens. Thank you for acknowledging the psychological weight alongside the medical facts.
Jason Jasper January 3, 2026
I’ve been on Tresiba and a Dexcom for 5 years. Time-in-range is 78%. I still hate the noise the pump makes at 3am. But I’m alive. That’s enough.