When it comes to your medicine, you should have a real say
You’re sitting in the doctor’s office. They hand you a prescription. You nod. You pay. You take it. But did you ever really get to choose? Or were you just told what to do?
For decades, medicine operated like this: doctor knows best. But that’s changing. Today, more patients are asking: What are my options? And they’re not just asking-they’re demanding to be part of the decision. This isn’t about being difficult. It’s about control over your own body.
Medication autonomy means you have the right to accept, refuse, or swap out a drug-even if your doctor thinks it’s the best choice. It’s not just ethics. It’s law. Since the 1970s, courts in the U.S. have ruled that patients must be told the real risks, benefits, and alternatives before giving consent. That includes side effects, costs, and even non-drug options. And it’s not just about signing a form. It’s about understanding.
Why medication choices feel different than other medical decisions
Getting an X-ray? You don’t live with the machine in your body. Surgery? It’s a one-time thing. But pills? They’re daily. Monthly. Yearly. They change your sleep, your mood, your sex life, your weight. Some cause nausea. Others make you feel numb. A few cost hundreds per month.
That’s why 73% of patients in a 2022 JAMA survey said they worried more about medication side effects than about diagnostic tests. A scan doesn’t change how you feel on Tuesday morning. A pill might.
And then there’s cost. One in three Medicare users in 2023 skipped doses or switched meds because they couldn’t afford them. That’s not noncompliance. That’s survival. If you can’t pay, you don’t have autonomy-you have a forced choice.
Direct-to-consumer ads make it worse. You see a commercial for a new antidepressant. You walk in and ask for it. Your doctor might say no. But now the conversation isn’t about what’s best for you-it’s about what you saw on TV.
How shared decision-making actually works (and why it often doesn’t)
Shared decision-making isn’t a buzzword. It’s a process. It means your doctor doesn’t just tell you what to take. They help you weigh options based on your life, your values, your fears.
For example: Two people have depression. One wants to avoid weight gain. The other can’t stand taking pills in the morning. One works nights. The other is a single parent. Same diagnosis. Different needs.
Studies show that when patients are involved in choosing their meds, they’re 82% more likely to stick with them. That’s huge. Adherence drops to 65% when the doctor picks for you.
But here’s the problem: most appointments are 15 minutes long. In that time, doctors are expected to diagnose, explain, prescribe, answer questions, and update records. No one has time to walk through a 10-option comparison chart.
Only 45% of primary care doctors consistently use shared decision-making for meds. Compare that to 68% for surgery. Why? Because pills feel routine. But they’re not.

The tools that help-when they’re actually used
There are tools designed to make this easier. Decision aids from places like the Mayo Clinic give clear, visual comparisons: Drug A reduces symptoms by 55%, but causes dry mouth in 1 in 4. Drug B works slower, but has fewer side effects. These aren’t marketing brochures. They’re evidence-based, updated quarterly, and free.
Some clinics use pre-visit questionnaires. You fill them out online before your appointment: What’s your biggest worry about this medication? What’s your budget? What’s your daily routine like? That gives your doctor a head start. One VA pilot cut patient decision conflict by 42% using this method.
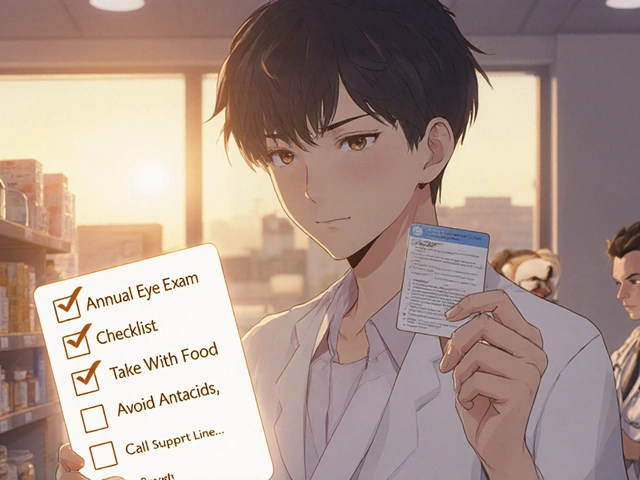
Pharmacists are stepping in too. Medication Therapy Management (MTM) services-offered by pharmacies like CVS and Walgreens-give you 30-minute one-on-one sessions. They check your whole list of meds, spot interactions, and help you understand why you’re taking each one. Patients using MTM are 31% more likely to take their meds as prescribed.
But here’s the catch: only 38% of Epic EHR systems-the most common electronic records in U.S. hospitals-have a way to document your medication preferences. So even if you talk about it, your next doctor might never see it.
Who gets left out-and why
Autonomy sounds great. But not everyone gets to use it equally.
Black patients are 25% less likely than white patients to report being involved in medication decisions. Hispanic patients? The gap is similar. Why? Language barriers. Cultural norms around respecting authority. Doctors assuming they won’t understand. Or worse-assuming they can’t afford it and skipping expensive options without asking.
Immigrant patients often don’t feel comfortable questioning a doctor’s advice. One survey found 35% of immigrants felt it was rude to challenge a prescription. That’s not compliance. That’s silence.
And older adults? 37% say they struggle to use digital tools that help with medication choices. Apps, portals, online forms-they’re designed for people who grew up with smartphones. Not for people who still use landlines.
Autonomy isn’t just about information. It’s about access. If you don’t have internet, transportation, time off work, or someone to help you understand, your "choice" is an illusion.
What happens when autonomy goes wrong
Some worry that giving patients full control leads to bad choices. And sometimes, it does.
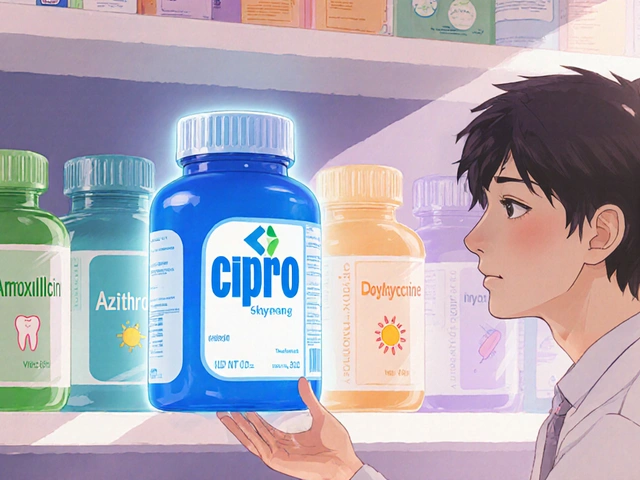
After social media spread false claims about antibiotics causing "long-term damage," requests to refuse them jumped 40% in 2022-2023. That’s dangerous. Antibiotics save lives. But patients don’t always know the difference between a viral cold and a bacterial infection.
Then there’s the "therapeutic misconception." Some patients think a clinical trial is just a better version of regular care. They sign up for a new drug, thinking it’s guaranteed to work. It’s not. That’s not autonomy-it’s misunderstanding.
And some doctors still withhold options. A 2023 AMA report called out cases where low-income patients were denied biologic drugs-expensive but life-changing treatments for arthritis and Crohn’s-because doctors assumed they couldn’t handle the cost or the complexity. That’s not protecting patients. It’s deciding for them.
True autonomy means offering all options-even the expensive, complicated, or inconvenient ones-and then helping the patient decide.

Where things are heading
Medicine is shifting. In January 2024, the American Society of Health-System Pharmacists launched the first official Medication Autonomy Framework. It’s 12 clear standards for how clinics should support patient choice.
The FDA now requires drugmakers to collect data on patient preferences before launching new medications. That means companies will ask: Would you rather take one pill a day or two? Would you trade a bit less effectiveness for fewer side effects? That’s new.
And pharmacogenomics? That’s the future. For under $250 now, you can get a DNA test that tells you how your body processes certain drugs. Maybe you’re a slow metabolizer of SSRIs. That means higher doses cause side effects. Your doctor can skip the trial-and-error. That’s personalized medicine-and real autonomy.
But here’s the hard truth: this progress won’t reach everyone. Rural clinics still lack resources. Understaffed hospitals can’t train staff in shared decision-making. And without systemic change, autonomy will remain a privilege for those who know how to ask.
What you can do right now
You don’t need to wait for the system to fix itself. Here’s how to take control:
- Ask for alternatives. "What are my other options?" Not just "Is there a cheaper one?"-but "What else works?"
- Ask about side effects. "How common is this?" Not "What are the risks?"-but "How many people actually get this?"
- Ask about cost. "Can you check if this is covered? Is there a generic? A coupon? A patient assistance program?"
- Ask about lifestyle. "Can I take this with food? At night? Will it make me drowsy?"
- Ask for time. "Can we schedule a follow-up to talk about how this is working?"
And if your doctor dismisses you? Find another one. Your health isn’t a one-size-fits-all product. It’s your life.
Medication autonomy isn’t about being difficult. It’s about being human.
It’s the cancer patient who refuses opioids because of her faith-and gets a better pain plan because her doctor listened.
It’s the diabetic who switched providers because her doctor wouldn’t discuss alternatives to Ozempic.
It’s the single mom who picks a once-daily pill because she can’t remember four doses.
Autonomy isn’t perfect. It’s messy. It takes time. It requires honesty-from both sides. But when it works, it changes everything. You’re not just taking a pill. You’re choosing your life.
Can I refuse a medication even if my doctor recommends it?
Yes. If you have decision-making capacity-meaning you understand the information, can weigh the risks and benefits, and communicate your choice-you have the legal and ethical right to refuse any medication, even if it’s considered standard care. Doctors are required to respect this, as long as you’re not under court order or in an emergency where you’re incapacitated.
What if my doctor won’t discuss other options?
If your doctor dismisses your questions or refuses to explain alternatives, you’re not being difficult-you’re being a responsible patient. Ask again. If they still won’t engage, it’s a red flag. You have the right to seek a second opinion or switch providers. Many clinics now use shared decision-making tools; if yours doesn’t, you can ask them to start.
Do I have to pay for medication decision aids?
No. Evidence-based decision aids from reputable sources like the Mayo Clinic, NIH, and the Agency for Healthcare Research and Quality are free to use. Many are available as printable PDFs or online tools. Your pharmacist or clinic may also have them on hand. Avoid commercial tools pushed by drug companies-they’re often biased.
How do I know if I have decision-making capacity?
You have capacity if you can understand your condition and treatment options, appreciate how the choices affect you, reason through pros and cons, and clearly express your decision. Most people do. If you’re confused, anxious, or overwhelmed, it’s okay to ask for more time, bring someone with you, or request written materials. Capacity isn’t about intelligence-it’s about clarity.
Are generic drugs always a good alternative to brand-name ones?
For most medications, yes. Generics have the same active ingredients, strength, and effectiveness as brand-name drugs. They’re tested by the FDA to ensure they work the same way. The only exceptions are a few narrow-therapeutic-index drugs (like warfarin or thyroid meds), where small differences matter. Even then, many patients switch safely. Cost savings can be huge-sometimes 80% less. Always ask your pharmacist: "Is there a generic? Is it safe for me?"
Can I change my mind after I start a medication?
Absolutely. Medication choices aren’t permanent. If you’re having side effects, it’s not working, or your life situation changed, you can talk to your doctor about switching. Many people stop meds in the first year-not because they’re noncompliant, but because they didn’t have enough information upfront. Revisiting your choice is part of responsible care.




Johanna Baxter January 9, 2026
I swear, doctors treat you like a child who can't handle the truth. I asked for a different antidepressant because the one they gave me made me feel like a zombie, and they acted like I was being unreasonable. Guess what? I switched doctors. My life improved overnight. No more crying in the shower at 3 a.m. Just because they went to med school doesn't mean they know what's best for YOU.
Jerian Lewis January 9, 2026
The system is broken. Patients aren't being given real choices-they're being handed a script and told to shut up. I've seen it too many times. Doctors skip the conversation because they're overworked. But that doesn't make it right.
tali murah January 11, 2026
Oh, here we go again. The noble patient demanding autonomy like it's a TED Talk. Let me guess-you also believe in crystal healing and that your ‘intuition’ should override clinical guidelines? The fact that 73% of people worry more about side effects than diagnostic tests tells you everything you need to know: people are terrified of their own bodies. And now we’re rewarding that fear with a 15-minute consult and a pamphlet? Brilliant.
Diana Stoyanova January 11, 2026
I used to think autonomy was just a buzzword until I was diagnosed with chronic migraines and my doctor actually sat down with me and said, ‘Okay, tell me what your life looks like.’ I work two jobs, I’m a single mom, I can’t take a pill every 6 hours. He didn’t push the fancy new drug-he gave me three options, all with side effect charts, costs, and even how they’d mess with my sleep. I picked the one that let me function. I cried. Not because I was sick-but because someone finally saw me as a person, not a case number. This isn’t about being difficult. It’s about being human. And honestly? We all deserve that.
Gregory Clayton January 12, 2026
America’s getting soft. Back in my day, you took what the doctor gave you and didn’t question it. Now everyone wants a vote on their antibiotics like it’s a democracy. We’re not running a town hall meeting-we’re saving lives. If you can’t handle a little authority, maybe you shouldn’t be in charge of your own health.
Ashley Kronenwetter January 13, 2026
While I agree with the principle of patient autonomy, the implementation remains inconsistent across socioeconomic lines. The burden of research, advocacy, and follow-up often falls disproportionately on those with higher health literacy and access to resources. Without structural reforms, the rhetoric of choice masks systemic inequity.
Micheal Murdoch January 15, 2026
I’ve been a nurse for 22 years. I’ve seen patients refuse meds because they saw a scary TikTok video. I’ve seen others refuse meds because their insurance wouldn’t cover it. And I’ve seen doctors ignore patient preferences because they’re running 45 minutes behind. This isn’t about blame. It’s about design. We need longer visits. Better tools. Pharmacists as true partners. And most of all-we need to stop treating patients like passive recipients and start treating them like collaborators. It’s not just ethical. It works.
Lindsey Wellmann January 15, 2026
I just want to say… 🙌 I asked for a generic and my doctor laughed. Like, actually laughed. Then handed me a $400 script. I cried. Then I went to CVS, talked to the pharmacist, and got the same drug for $12. 🥲💊 #PatientPower #StopThePriceGouging
Jacob Paterson January 16, 2026
Oh please. You think you’re so enlightened because you ‘asked for alternatives’? Most people don’t even know what a therapeutic index is. You’re not being autonomous-you’re being reckless. And now we’re rewarding ignorance with a ‘choice’ that could kill someone? Wake up. Autonomy without education is just chaos with better PR.
Kiruthiga Udayakumar January 17, 2026
In India, we don’t even get to ask. My aunt was given a diabetes pill she couldn’t afford. She skipped doses. Got sick. No one asked if she could pay. No one offered alternatives. They just said, ‘Take it.’ So I started teaching my family how to ask. One question at a time. ‘Is there a cheaper one?’ ‘What happens if I skip?’ ‘Can we try something else?’ It’s not rebellion. It’s survival.