When someone is diagnosed with Huntington’s disease, it’s not just a medical label-it’s a life shift. The news doesn’t come with a cure, a quick fix, or even a clear timeline. Instead, it brings a cascade of questions: How did this happen? What will my body do next? How do I plan for a future I can’t control? This isn’t theoretical. For families affected by HD, these are daily realities.
The Genetic Time Bomb
Huntington’s disease isn’t caught like a cold or triggered by lifestyle. It’s inherited. If one parent carries the mutated gene, each child has a 50% chance of getting it. No exceptions. No luck. Just pure, cold genetics. The problem lies in a single gene on chromosome 4 called HTT. Inside that gene, a tiny sequence-CAG-is repeated too many times. Normal people have 10 to 26 repeats. If you have 40 or more, you will develop Huntington’s. There’s no gray area. Between 36 and 39, it’s uncertain-some will, some won’t. But 40 and above? It’s guaranteed.The more repeats, the earlier the symptoms start. Someone with 50 repeats might show signs in their teens. Someone with 45? Maybe their early 30s. And if the mutation comes from the father, it’s more likely to grow bigger during sperm production. That’s why 85% of juvenile cases-those starting before age 20-come from the dad’s side. This is called genetic anticipation. It’s not magic. It’s biology. And it means a father who lived into his 60s with mild symptoms could pass on a version so aggressive that his child is wheelchair-bound by 16.
That’s why genetic testing is so heavy. People who have a parent with HD often wait years-sometimes decades-to get tested. Why? Because knowing doesn’t change the outcome. It just changes how you live. A 2023 survey from the European Huntington’s Disease Network found that 72% of at-risk individuals delay testing until symptoms appear. They’re not avoiding it out of ignorance. They’re protecting their peace.
Chorea: The Unwanted Dance
If you’ve never seen chorea, it’s hard to describe. Imagine your body moving without permission. Fingers twitch. Shoulders shrug. Feet tap. Then your head jerks. Your arm swings out like you’re waving at someone who isn’t there. These movements aren’t rhythmic. They’re random. Wild. Unpredictable. And they disappear when you sleep.This isn’t just embarrassing-it’s exhausting. People with chorea can’t hold a cup without spilling. They can’t walk a straight line. They can’t sit still in a meeting. At first, it’s mild. Maybe just a fidgety hand or an odd facial tic. Doctors call this a UHDRS score of 1 or 2. By the time it hits 3 or 4, the movements are constant. The body doesn’t rest. The person doesn’t rest.
Chorea happens because the brain’s control center-the striatum-is dying. Specifically, the neurons that calm movement are the first to go. Without them, the body overreacts. Every signal becomes noise. And as the disease progresses, chorea doesn’t stay alone. It brings friends: stiffness, slow movements, muscle cramps. What looked like dancing becomes a tangled mess of muscle failure.
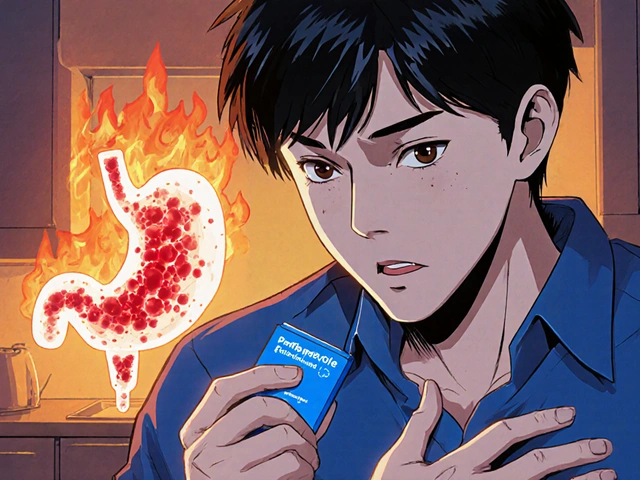
The only FDA-approved drugs for chorea are tetrabenazine and deutetrabenazine. Both work by lowering dopamine in the brain. They can reduce movements by about 25-30%. But they come with a cost. One in five people get depressed. Many feel drained, sluggish, or emotionally flat. That’s why some patients refuse them. They’d rather keep the chorea than lose themselves.
There’s a newer option, valbenazine, approved in 2023. It’s slightly less likely to cause depression, but still carries risks. And it doesn’t stop the disease. It just tries to quiet the noise.

Care Planning: The Real Treatment
Here’s the truth most people don’t talk about: There is no cure. But care planning saves lives. A 2021 study from the Enroll-HD global registry showed that patients who had structured care plans lived 2.3 years longer than those who didn’t. Why? Because they avoided hospitalizations. They didn’t choke on food. They didn’t take their own lives. They didn’t get lost in the system.Care planning isn’t a one-time meeting. It’s a roadmap that changes as the disease moves. In the early stage-right after diagnosis-people need to talk about what they want if they can’t speak for themselves. Only 37% of patients in general neurology clinics do this. At specialized HD centers, it’s 82%. That gap is deadly.
By year five, most people need help with daily tasks. Bathing. Dressing. Eating. Occupational therapists teach new ways to hold a toothbrush. Speech therapists help with slurred speech. Nutritionists adjust diets to prevent choking. By year ten, nearly half of patients need speech therapy. By year fifteen, most can’t live alone.
By year twenty, 89% need full-time residential care. The average annual cost? $125,000. And that’s in the U.S. Many families spend over $5,000 out-of-pocket each year on therapies insurance won’t cover. Aquatic therapy helps balance better than land-based exercises. But not everyone can afford a pool.
Coordination is the biggest hurdle. One caregiver told the HDSA forum: “I spend 20 hours a week just scheduling appointments.” Neurologist. Psychiatrist. PT. OT. Social worker. Dietitian. Genetic counselor. Each one has their own office, their own schedule, their own paperwork. Getting them to talk to each other? That’s the real challenge.
Specialized HD centers-there are 53 in the U.S.-do this well. They hold quarterly team meetings. They keep full care plans. They train staff in HD-specific communication. But only 53% of them actually meet quarterly. Insurance doesn’t pay enough. Staff burn out. Patients fall through.

What Works-And What Doesn’t
There’s a lot of hype around new drugs. Wave Life Sciences’ SELECT-HD trial showed a 38% drop in mutant huntingtin protein after 135 weeks. Roche’s tominersen trial was paused, then restarted with lower doses. These are promising. But they’re years away from being widely available. And even if they work, they won’t fix what’s already broken.Right now, the most effective treatment isn’t a pill. It’s a team. A care plan. A conversation.
People who start planning early live longer. They stay out of the ER. They avoid feeding tubes. They die with dignity, not chaos. One doctor at Johns Hopkins put it plainly: “Even with successful gene therapies, comprehensive care planning will remain critical for the 40,000+ Americans currently living with HD.”
That’s the hard truth. Science might one day stop Huntington’s. But today, it’s care planning that keeps people alive.
Where to Start
If you or someone you love has been diagnosed:- Find an HD specialty center. Use the HDSA website to locate one. They know the system. They’ve seen this before.
- Do advance directives now. Not someday. Not when you’re “ready.” Now. A living will. A healthcare proxy. Name who speaks for you.
- Get genetic counseling. Even if you’re not tested, understanding inheritance helps your family.
- Build your team. Neurologist, therapist, social worker. Don’t wait for a crisis to call them.
- Connect with others. The HDSA forum and r/huntington on Reddit are full of people who get it. They share tips, resources, and sometimes just silence.
There’s no perfect path. But there is a better one. And it starts with planning-not waiting.
Is Huntington’s disease always inherited?
Yes. Huntington’s disease is caused by a single mutated gene passed down from parent to child. If a parent has the mutation, each child has a 50% chance of inheriting it. In rare cases (under 1%), a person can have the mutation without a known family history due to a new mutation or misattributed parentage, but this is extremely uncommon.
Can you get Huntington’s disease if neither parent has it?
Almost never. HD is an autosomal dominant disorder, meaning you need only one copy of the mutated gene to develop it. If neither parent carries the mutation, you cannot inherit it. Very rarely, a new mutation can occur during sperm or egg formation, but this is estimated to happen in less than 1% of cases.
What does chorea look like in early-stage Huntington’s?
In early stages, chorea is often subtle. It might look like fidgeting, restlessness, or minor facial grimacing. People may seem clumsy-dropping things, stumbling slightly, or having trouble with fine motor tasks like buttoning a shirt. These movements are involuntary and disappear during sleep. Often, family members notice them first, thinking it’s just nervous energy or stress.
Are there any drugs that stop Huntington’s from progressing?
No. Currently, no medication can slow or stop the underlying brain degeneration caused by Huntington’s disease. Treatments like tetrabenazine, deutetrabenazine, and valbenazine only manage chorea symptoms. Experimental therapies targeting the mutant huntingtin protein are in clinical trials, but none have been proven to halt progression yet.
Why is care planning so important in Huntington’s disease?
Care planning directly impacts survival and quality of life. Studies show that patients with structured, early care plans live 2.3 years longer on average. They’re less likely to be hospitalized for pneumonia, falls, or suicide. Planning ensures someone can speak for the patient when they can’t speak for themselves. It coordinates specialists, prevents gaps in care, and helps families prepare emotionally and financially for the long haul.
How much does Huntington’s disease care cost?
The average annual cost of care in the U.S. is about $125,000 per person by the late stages. This includes medications, therapy, home care, and eventually residential facilities. Out-of-pocket expenses for non-covered services-like specialized therapy or adaptive equipment-can exceed $5,000 a year for many families. Total U.S. healthcare spending on HD is estimated at $1.5 billion annually.
Can genetic testing predict exactly when symptoms will start?
Not precisely. While the number of CAG repeats correlates with likely age of onset-more repeats usually mean earlier symptoms-it’s not exact. Two people with 45 repeats might develop symptoms 10 years apart. Other genetic and environmental factors play a role. Testing gives a range, not a calendar date.
What’s the difference between tetrabenazine and deutetrabenazine?
Both reduce chorea by lowering dopamine levels. Tetrabenazine (Xenazine) was approved in 2008 and requires multiple daily doses. Deutetrabenazine (Austedo), approved in 2017, is chemically modified to last longer, so it’s taken twice daily instead of three or four times. Austedo has a slightly lower risk of depression and sedation, which is why it now holds 65% of the chorea treatment market.





aditya dixit December 4, 2025
It’s wild how genetics doesn’t care about your plans. You can meditate, save money, learn five languages - none of it matters when your DNA has already written the ending. But knowing that doesn’t make it easier. It just makes you more intentional. I’ve watched my uncle go from chess champion to needing help tying his shoes. He never got tested. Said he’d rather live with hope than live with certainty. I get it.
There’s no heroism in waiting. Just humanity.
And yeah - care planning isn’t glamorous. But it’s the quietest form of love there is.
Lynette Myles December 5, 2025
They’re lying about the 50% chance. It’s not random - it’s controlled. The gene was engineered. You think Big Pharma wants a cure? No. They want patients on Austedo for life. That’s why the trials are slow. That’s why they buried the real data. Watch the videos - the chorea disappears in some cases after fasting. They don’t want you to know that.
Annie Grajewski December 5, 2025
Okay but like… why is everyone so chill about this? Like, ‘oh yeah my dad’s gonna turn into a human marionette by 40’? Bro. That’s not a ‘life shift.’ That’s a horror movie where the protagonist is your mom.
And why do we act like tetrabenazine is the only option? What about CBD? Or that guy in Oregon who cured his Huntington’s with mushroom tea? No one talks about that. Probably because the FDA doesn’t sell mushrooms.
Also - why are we still using ‘chorea’? Sounds like a dance move from 1998. Just say ‘random body spasms.’ Less fancy, more real.
Jimmy Jude December 7, 2025
Let me tell you something - this isn’t about genetics. This is about the collapse of the American family. You think your kid’s gonna get this because of DNA? Nah. It’s because you didn’t show up. You didn’t talk. You didn’t hold their hand when they were scared. So now they’re alone in a hospital with a nurse who doesn’t know their name.
And don’t get me started on ‘care planning.’ That’s just a fancy word for giving up. You don’t plan for death. You fight it. Every day. Even if you’re shaking. Even if you can’t speak. You fight.
My cousin died at 32. He danced until his last breath. That’s the real legacy. Not a living will.
Stop planning. Start living. Even if it’s broken. Especially if it’s broken.
Mark Ziegenbein December 8, 2025
Look - I’ve read every paper on HTT since 2012. I’ve sat in three clinical trials. I’ve watched my sister’s striatum decay on an fMRI like a time-lapse of a dying star. And let me tell you - the idea that ‘care planning saves lives’ is the most patronizing thing I’ve ever heard. Of course it does. But that’s like saying ‘wearing a seatbelt saves lives’ after you’ve been hit by a train.
Yes - structured care reduces hospitalizations. Yes - coordination matters. But none of it changes the fact that your brain is being eaten alive by a CAG repeat that shouldn’t exist. And the fact that we treat this like a logistics problem instead of a tragedy is the real crime.
And don’t get me started on those ‘HD centers.’ They’re glorified call centers with white coats. Half the staff don’t know the difference between dyskinesia and dystonia. And insurance pays them $120 an hour to say ‘we’re here for you’ while your daughter chokes on her oatmeal.
Science is coming. But it’s coming too late for the people who needed it yesterday.
Laura Saye December 9, 2025
I just want to say - I see you. All of you. The ones who are scared. The ones who are tired. The ones who pretend they’re okay so they don’t break in front of their kids.
There’s no need to be brave right now. Just be present. Even if it’s messy. Even if you cry in the car after the appointment. Even if you can’t say the word ‘Huntington’s’ out loud yet.
That’s enough. That’s everything.
And if you need someone to sit with you in silence - I’m here. No advice. Just presence.
luke newton December 10, 2025
People keep saying ‘care planning saves lives’ like it’s some moral victory. But let’s be real - it’s just delaying the inevitable while you go broke. Why are we glorifying this? Why not just say ‘this disease kills you slowly and the system is rigged’?
And who are we kidding? The only people who get ‘structured care’ are the ones with money, insurance, and white skin. My cousin in Alabama got a pamphlet and a prayer. He died at 38. No therapist. No team. Just a hospice nurse who didn’t know his name.
Stop pretending this is about ‘planning.’ It’s about class. And privilege. And who gets to die with dignity.
Ali Bradshaw December 11, 2025
I’ve been a caregiver for 11 years. My wife was diagnosed at 34. We didn’t know what we were doing. We still don’t. But we learned one thing - small things matter.
Like leaving the lights on at night so she doesn’t fall.
Like playing her favorite album on loop so she can hum along even when she can’t speak.
Like holding her hand when the chorea hits hard and she’s screaming inside but can’t make a sound.
There’s no grand plan. Just presence. And love. And showing up. Even when you’re exhausted.
That’s the real treatment.
an mo December 12, 2025
Let’s not sugarcoat this - this is a genetic flaw in the white population. HD is overrepresented in Western countries because of inbreeding, poor gene pools, and low birth control rates in certain demographics. We’re seeing the cost of liberal eugenics. The solution isn’t ‘care plans.’ It’s population control. And maybe stopping people with the gene from reproducing.
Also - why are we funding research when we could just cut Medicaid for HD patients? Saves money. Reduces burden. Common sense.
Juliet Morgan December 14, 2025
My mom has HD. She’s 58. She still laughs. Still cooks. Still tells bad jokes. The chorea? Yeah. It’s there. But she doesn’t let it win.
She started planning when she was 45. Got her will. Named my sister and me as proxies. Learned to use a speech app. Found a therapist who didn’t treat her like a patient.
She didn’t wait. She didn’t cry for a year. She just… did it.
I used to think that was strength. Now I think it’s just love.
Don’t wait for ‘ready.’ Just start.
Norene Fulwiler December 15, 2025
In my village in Nigeria, we don’t have HD centers. We don’t have Austedo. We have family. We have songs. We have hands that wash, feed, hold.
They don’t call it ‘care planning.’ They call it ‘we don’t leave our own.’
Maybe the real lesson isn’t in the gene - it’s in the community.
Don’t let the system make you feel alone. You’re not.
Stephanie Fiero December 16, 2025
So I just got tested. 47 repeats. I’m 29. I’ve been waiting 10 years. I didn’t cry. I just stared at my coffee. Then I called my sister and said ‘we need to talk about the will.’
My therapist said I was ‘processing well.’ I told her I wasn’t processing. I was just… existing.
But I’m not done yet.
I’m gonna learn to dance. Even if my body shakes. I’m gonna say ‘I love you’ every day. Even if I forget to say it later.
And if I can’t speak? I’ll write it down.
This disease doesn’t get to take my voice. Not yet.
Krishan Patel December 17, 2025
Genetics is a myth. HD is a scam created by the medical-industrial complex to sell drugs. The CAG repeat is just a biomarker - not a cause. The real cause is glyphosate in our food and 5G radiation. Look at the data - HD rates spiked after 2008. Coincidence? I think not.
Also - why are you trusting doctors? They’re paid by pharma. They don’t care about you. They care about their bonuses.
Try magnesium. Or turmeric. Or fasting. Those work. Not your fancy pills.
Wake up. This isn’t science. It’s control.
Carole Nkosi December 17, 2025
My grandmother had HD. She danced until she couldn’t stand. Then she sat. Then she whispered. Then she was gone.
We didn’t have money for therapists. We didn’t have a care plan. We had stories. We had her voice. We had her laugh.
They say you need a team. I say you need a memory.
She’s still here. In the way I hold my spoon. In the way I hum when I’m nervous.
That’s the cure. Not a pill. Not a plan. Just love that outlives the body.