What Is Complex Regional Pain Syndrome?
Complex Regional Pain Syndrome is a chronic neurological condition that causes severe, burning pain in an arm, leg, hand, or foot after an injury, even if the injury itself was minor. It used to be called Reflex Sympathetic Dystrophy (RSD), but now it’s known as CRPS, with two types: Type I (no confirmed nerve damage) and Type II (with clear nerve injury). About 90% of cases are Type I.
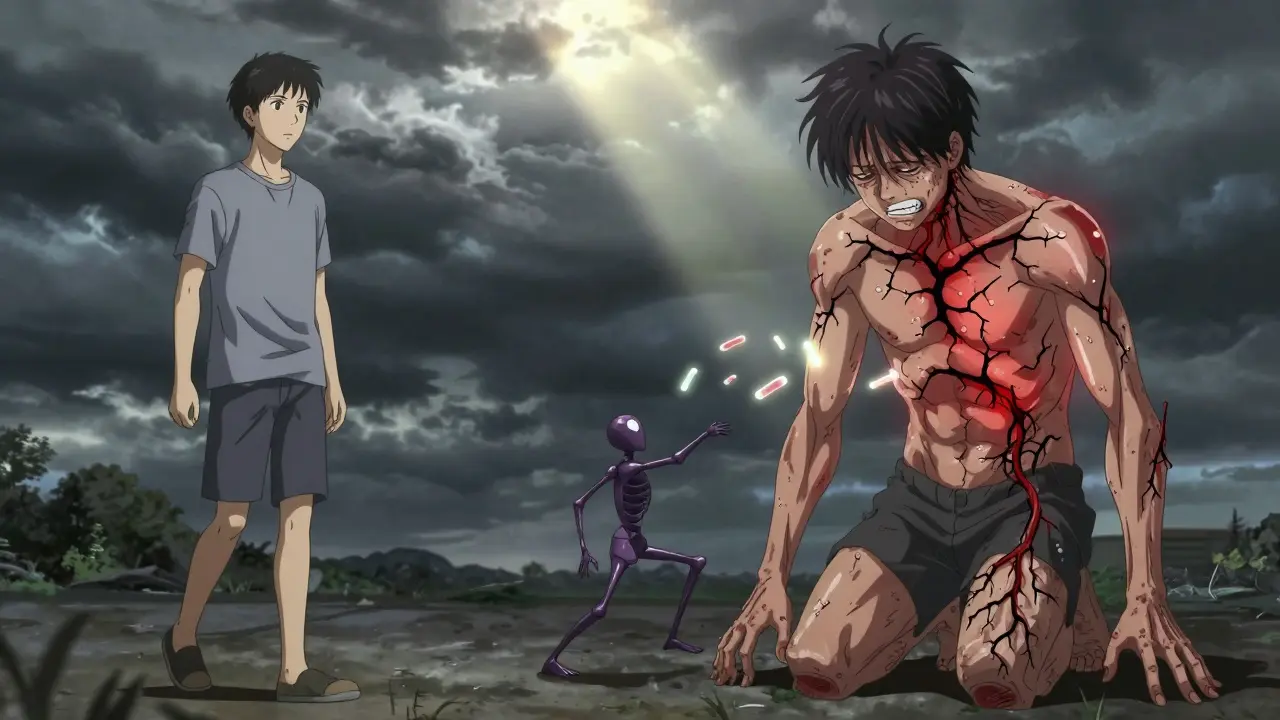
Unlike normal pain that fades as an injury heals, CRPS pain doesn’t stop. It gets worse over time. People describe it as a constant burning, stabbing, or electric shock feeling deep inside the affected limb. The pain is way out of proportion to what happened - a simple wrist fracture, a sprain, or even a needle stick can trigger it.
Why Does the Pain Feel So Extreme?
Your nervous system normally sends pain signals to warn you of damage. Once the injury heals, those signals stop. With CRPS, something goes wrong. The nerves keep firing, even when there’s no tissue damage left. The brain starts interpreting normal sensations - like light touch or a breeze - as agony.
It’s not just nerves misfiring. Inflammation plays a big role, especially in the first few months. Blood vessels in the affected area swell, skin turns red or blotchy, and the limb may feel warmer or colder than the other side. Some research suggests the immune system might be attacking the body’s own nerves, a possible autoimmune response. In 30% of patients, scientists have found unusual antibodies linked to CRPS.
The sympathetic nervous system - the part that controls things like heart rate and sweat - also gets stuck in overdrive. This is why one limb might be sweaty and shiny while the other is dry. The body’s natural pain control system breaks down, and the pain signal becomes self-sustaining.
What Triggers CRPS?
Most cases start after trauma. Fractures are the top trigger - about 40% of CRPS cases follow a broken bone, especially in the wrist. Surgery is another common cause, like carpal tunnel repair or knee arthroscopy. Even minor injuries like sprains, cuts, or burns can lead to CRPS. Surprisingly, some people develop it without any clear injury at all.
It’s not about how bad the injury was. Two people can break the same bone in the same way. One recovers fine. The other develops CRPS. Why? No one knows for sure. Genetics might play a role. So might stress, anxiety, or how someone responds emotionally to pain. But no single gene or test can predict who will get it.
What Are the Signs You Might Have CRPS?
CRPS doesn’t show up on X-rays or MRIs. Diagnosis is based on symptoms and physical exam using the Budapest Criteria. If you have pain that’s:
- Disproportionate to the original injury
- Constant or intermittent, with burning, shooting, or electric sensations
- Worsened by touch, temperature, or movement
- Along with at least one sign from three categories - changes in skin temperature, color, or texture; swelling or sweating; limited movement or weakness
Early signs include:
- Skin that’s shiny, thin, or overly sweaty
- Changes in color - red, purple, pale
- Nails growing faster or becoming brittle
- Hair growth speeding up or stopping
- One limb noticeably warmer or cooler than the other
- Difficulty moving the limb - stiffness, tremors, or muscle spasms
These symptoms often start within four to six weeks after the injury. If you notice them, don’t wait. Early diagnosis is the biggest factor in stopping CRPS from becoming permanent.

Who Gets CRPS?
CRPS is rare, but it’s not random. Women get it about three times more often than men. It’s most common between ages 40 and 60, but teens and young adults can develop it too. People with a history of anxiety, depression, or chronic pain conditions may be more vulnerable, but even healthy, active individuals aren’t immune.
One big red flag: if your cast or bandage feels too tight, and the pain keeps getting worse instead of better, that’s a warning sign. So is pain that spreads beyond the original injury site - like pain moving from your wrist up your arm.
How Is CRPS Treated?
There’s no magic cure, but early treatment can stop it from getting worse. The goal is to reset the nervous system before it gets stuck in pain mode.
Physical therapy is the most important first step. Moving the affected limb - even if it hurts - helps retrain the brain. A therapist will guide you through gentle exercises to keep joints flexible and muscles strong. Avoiding movement makes CRPS worse. Many people delay therapy out of fear, but that’s the worst thing you can do.
Medications help manage symptoms:
- NSAIDs like ibuprofen for inflammation in early stages
- Corticosteroids (like prednisone) for swelling and redness
- Neuropathic pain drugs like gabapentin or pregabalin to calm overactive nerves
- Antidepressants like amitriptyline to help with pain signaling and sleep
For more severe cases, doctors may try nerve blocks - injecting numbing medicine near the affected nerves to interrupt pain signals. Spinal cord stimulation, where a small device sends mild electrical pulses to the spine, can also help. Ketamine infusions are being studied for stubborn cases, showing promise in resetting pain pathways.
What Happens If It’s Not Treated?
CRPS can get worse over time. Without treatment, the limb may become stiff, weak, and hard to use. Muscles can shrink. Skin and bones can thin. Pain can spread to other parts of the body. The emotional toll is heavy - depression, anxiety, and sleep loss are common. Some people lose their jobs. Others can’t hold their kids or drive.
But here’s the hopeful part: if caught early - within the first three months - up to 80% of people see major improvement or full recovery. The longer it goes untreated, the harder it becomes to reverse.
Can CRPS Go Away on Its Own?
Some cases do improve without treatment. But waiting is risky. Pain that lingers for months or years becomes harder to treat. The nervous system adapts to the pain, making it a permanent part of how the brain works. That’s why experts say: if you suspect CRPS, act fast.
It’s not just about pain relief. It’s about protecting your ability to move, work, and live normally. Early intervention - even if it’s just physical therapy and education - makes a huge difference.
What’s New in CRPS Research?
Scientists are working on better ways to diagnose and treat CRPS. Blood tests to detect autoantibodies are in development. Brain imaging is showing how CRPS changes the way the brain processes pain. New drugs targeting inflammation and nerve repair are being tested in clinical trials.
The big shift in thinking: CRPS isn’t just a pain problem. It’s a nervous system disorder with physical, emotional, and immune components. That’s why treatment needs to be multidisciplinary - combining rehab, medicine, psychology, and sometimes nerve stimulation.
One promising area: personalized medicine. If your CRPS is driven by inflammation, you get anti-inflammatories. If it’s nerve damage, you get nerve-targeted drugs. If it’s brain-based, you get cognitive therapy. No one-size-fits-all approach works anymore.
What Should You Do If You Think You Have CRPS?
If you had an injury - even a small one - and now you have burning pain, swelling, or skin changes that won’t go away:
- Don’t ignore it. Don’t assume it’s just "normal" healing.
- See a doctor who knows about CRPS - a pain specialist, neurologist, or physiatrist.
- Ask about the Budapest Criteria and whether CRPS is possible.
- Start physical therapy immediately, even if it hurts.
- Keep moving. Don’t protect the limb - retrain it.
- Get support. CRPS is isolating. Talk to others who have it.
There’s no shame in having CRPS. It’s not your fault. It’s not "all in your head." It’s a real, measurable condition of the nervous system. And with the right care, many people get their lives back.
Can CRPS develop without an injury?
Yes. While most cases follow trauma like fractures or surgery, some people develop CRPS without any clear injury. This is less common, but documented. The nervous system can become dysregulated due to stress, illness, or unknown triggers. The key is recognizing the symptoms - burning pain, skin changes, sensitivity - and seeking help, regardless of how the condition started.
Is CRPS the same as nerve damage?
Not exactly. CRPS Type II involves confirmed nerve injury, but Type I - the most common form - happens without visible nerve damage. Even so, the nervous system still malfunctions. It’s not just about broken nerves; it’s about how the brain and spinal cord interpret pain signals. So yes, nerve dysfunction is central to CRPS, but not always from direct trauma.
Can CRPS spread to other parts of the body?
Yes. In about 70% of cases, pain spreads from the original site - like from the wrist up the arm or from the ankle to the knee. This is called regional spread. In rare cases, it can affect limbs on the opposite side of the body. This is why early treatment is critical: the longer CRPS goes unchecked, the more the nervous system learns to amplify pain everywhere.
Does cold weather make CRPS worse?
Many people with CRPS report that cold, damp weather increases their pain and stiffness. This is likely because temperature changes trigger abnormal nerve signals in the affected area. The limb may already have poor circulation or abnormal temperature control. Keeping the area warm with gloves, socks, or heating pads (on low) can help reduce flare-ups.
Is CRPS permanent?
Not always. About half of people see significant improvement within the first year, especially with early treatment. Some recover fully. But if CRPS lasts more than two years without proper care, it can become long-term or permanent. The key is action - the sooner you start physical therapy and manage symptoms, the better your chances of recovery.







Solomon Ahonsi February 2, 2026
This whole CRPS thing is just another way doctors make money off people who can't walk right. I broke my wrist last year, it hurt for a week, then I got back to lifting. Now some guy's telling me I should've been doing physical therapy for months? Bullshit. If your body can't handle a simple fracture, maybe you're just weak.
George Firican February 3, 2026
What fascinates me about CRPS is how it exposes the fragile, almost poetic architecture of human perception. Pain isn't merely a signal-it's a narrative the brain constructs, and when that narrative becomes self-referential, the body becomes a prison of its own making. The nervous system, once a messenger, becomes the tyrant. The immune system, a protector, turns traitor. We're not just treating a condition; we're negotiating with a mind that has forgotten how to unlearn suffering. It's not a disease of the limb-it's a rebellion of the entire organism against the illusion of safety. And yet, we still have hope: neuroplasticity, that quiet miracle, suggests the brain can relearn peace, even after betrayal.