If you’ve been lying awake for hours night after night, counting sheep until your brain screams for mercy, you’re not broken. You’re not lazy. And no, drinking more wine or taking melatonin isn’t going to fix this. Chronic insomnia isn’t just bad sleep-it’s a persistent condition that rewires your brain’s relationship with rest. According to the American Academy of Sleep Medicine, it’s defined as trouble falling or staying asleep, or waking up feeling unrefreshed, happening at least three nights a week for three months or more. And here’s the hard truth: if you’ve been told to just “sleep better” by avoiding caffeine or turning off your phone, you’ve been given a bandage for a broken bone.
Why Sleep Hygiene Isn’t Enough
You’ve heard it all: no screens before bed, keep your room cool, avoid alcohol, stick to a schedule. These are the staples of sleep hygiene. And yes, they help-if you’re dealing with a temporary bout of stress or jet lag. But for chronic insomnia? They’re like trying to stop a leaky roof with duct tape. The Sleep Foundation and multiple clinical guidelines confirm that sleep hygiene alone has only moderate evidence of effectiveness. In fact, leading researchers like Dr. Jack D. Edinger say it should never be used as a standalone treatment for chronic cases.Why? Because chronic insomnia isn’t about habits-it’s about conditioned anxiety. Your brain has learned to associate your bed with frustration. You lie down at 11 p.m., wake up at 1 a.m., check the clock, panic, try harder to sleep, and fail again. Over time, your body starts reacting to your bedroom like a threat. No amount of blackout curtains or lavender spray will undo that. That’s why sleep hygiene, while helpful as a supporting tool, fails to address the core problem: the mental loops and physical habits that keep insomnia alive.
What CBT-I Really Is (And Why It Works)
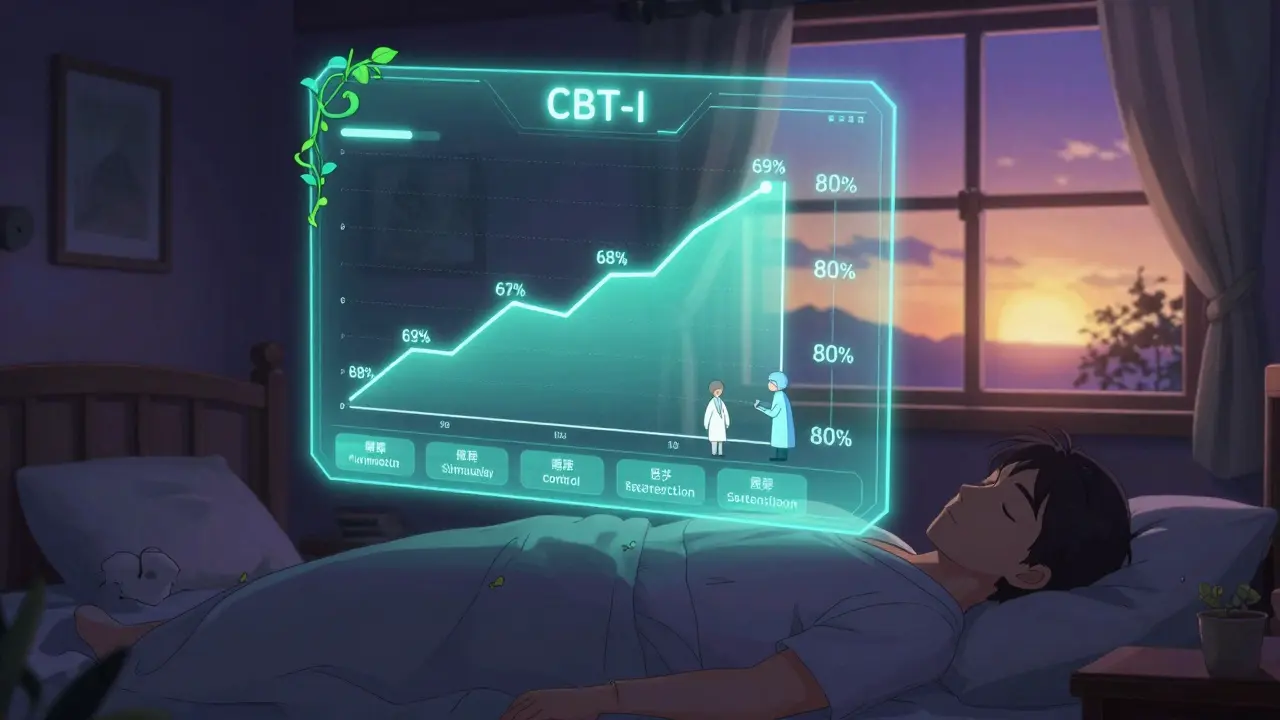
Cognitive Behavioral Therapy for Insomnia, or CBT-I, is the only treatment backed by decades of research as the first-line solution for chronic insomnia. It’s not a pill. It’s not a gadget. It’s a structured, evidence-based program that reteaches your brain how to sleep. The American College of Physicians, the American Academy of Sleep Medicine, and even the U.S. military all recommend it as the gold standard.CBT-I isn’t one thing-it’s five tools working together:
- Stimulus Control: Your bed is only for sleep and sex. No reading, no scrolling, no worrying. If you’re not asleep in 15-20 minutes, get up. Go to another room. Do something quiet and boring until you feel sleepy. Then return to bed. Repeat. This breaks the mental link between your bed and wakefulness.
- Sleep Restriction: This sounds counterintuitive-and it’s the hardest part. You’re told to spend less time in bed, not more. If you’re only sleeping 5 hours a night, you’re told to limit your time in bed to 5 hours. That means going to bed later and waking up earlier. It’s brutal for the first two weeks. You’ll feel exhausted. But it rebuilds your sleep drive. As your sleep efficiency climbs above 85%, your time in bed slowly increases. Studies show this alone can increase sleep efficiency from 68% to 89% in just 8 weeks.
- Cognitive Restructuring: You think, “If I don’t get 8 hours, I’ll collapse at work.” Or, “I’m going to fail because I slept badly.” These thoughts aren’t facts-they’re fears. CBT-I helps you challenge them. One 2019 study found that 65% of patients saw a major drop in sleep-related anxiety after just 6 sessions of cognitive restructuring.
- Relaxation Training: Not just deep breathing. Techniques like progressive muscle relaxation, diaphragmatic breathing, and mindfulness help calm your nervous system so your body doesn’t stay stuck in fight-or-flight mode at night.
- Sleep Hygiene: Yes, it’s still part of it-but now it’s used as a support, not the main event. Keeping your room at 65°F (18.3°C), using white noise, and cutting caffeine after 2 p.m. help reinforce the changes, not create them.
CBT-I typically takes 6-8 weekly sessions with a trained therapist. But even short, 2-session versions have shown results. The goal isn’t to fall asleep instantly-it’s to stop fighting sleep. And the results? 70-80% of people see clinically meaningful improvement. That’s better than any medication.
Why Medications Fall Short
Pills like zolpidem, eszopiclone, or suvorexant might help you fall asleep faster the first week. But after 4-6 weeks, their effect fades. Worse-they come with risks: dependence, memory fog, next-day grogginess, and even increased fall risk in older adults. A 2020 meta-analysis showed that while medications reduce sleep onset latency by about 12 minutes, CBT-I knocks off 18 minutes-and keeps working after you stop. Medication benefits vanish when you quit. CBT-I’s gains last for years.One Reddit user wrote: “The first two weeks of sleep restriction felt like torture. I was a zombie. But by week 6, I was falling asleep in 15 minutes instead of 2 hours. I haven’t taken a pill in 14 months.” That’s not luck. That’s science.
The Real Barriers to Getting Help
You might be thinking: “This sounds perfect. Where do I find it?” That’s the problem. There are only about 0.5 certified CBT-I therapists per 100,000 people in the U.S. In rural areas, 78% of counties don’t have a single sleep specialist. Insurance often covers only 3-4 sessions, even though 6-8 are recommended. Many people give up because they can’t finish the program.But digital options are changing that. Apps like Sleepio and SHUTi have been tested in randomized trials and shown 50-60% remission rates-far better than control groups at 15-20%. The FDA has cleared digital CBT-I programs like Somryst as prescription digital therapeutics. They use the same protocols as in-person therapy, delivered through video modules, sleep diaries, and AI feedback. One 2021 JAMA study found users of these apps slept 30 minutes longer per night and had 40% less insomnia severity after 12 weeks.
Even wearables are catching on. Fitbit now includes sleep restriction guidance in its Sleep Profile feature, using 30+ nights of data to suggest optimal bedtimes. It’s not a replacement for full CBT-I, but it’s a step toward accessibility.
What to Expect in the First Few Weeks
If you start CBT-I, prepare for discomfort. The first two weeks are the hardest. Sleep restriction means you’ll be tired. You might feel irritable. You might question whether it’s worth it. That’s normal. Sixty-two percent of users report worse sleep in the beginning. But here’s what happens next:- By week 3: You start sleeping more efficiently. Less time awake in bed.
- By week 5: You stop checking the clock. Your anxiety drops.
- By week 8: You’re falling asleep faster. Waking up less. Feeling rested.
And the daytime benefits? Just as powerful. A 2022 Sleepio survey found 78% of users reported less fatigue, better focus, and improved mood. That’s not just better sleep-it’s a better life.
How to Start
You don’t need to wait for a therapist to begin. Here’s your starter plan:- Track your sleep for 7-14 days. Write down when you get in bed, when you fall asleep, when you wake up, and how many times you wake during the night. Use a notebook or a free app like Sleep Cycle.
- Calculate your average total sleep time. If you’re sleeping 5.5 hours, that’s your starting time in bed.
- Set a fixed wake-up time-even on weekends. This is non-negotiable.
- Go to bed only when you’re sleepy. No forcing it.
- If you’re not asleep in 15-20 minutes, get up. Go to another room. Read a dull book under dim light. Return only when sleepy.
- Cut caffeine after 2 p.m. No alcohol within 4 hours of bed. No fluids after 7 p.m. to avoid bathroom trips.
- Keep your bedroom at 65°F. Use blackout curtains. Try a white noise machine.
Do this for 4 weeks. Then re-evaluate. If your sleep efficiency (total sleep time divided by time in bed) is above 85%, you can slowly add 15 minutes to your bedtime. If it’s below 80%, stay where you are.
When to Seek Professional Help
If after 4 weeks you’re still sleeping less than 5 hours a night, or your insomnia score (using the Insomnia Severity Index) is above 15, it’s time to find a CBT-I specialist. Look for a licensed psychologist or sleep therapist trained in CBT-I. Ask: “Do you use the full protocol-stimulus control, sleep restriction, and cognitive restructuring?” If they say “just avoid caffeine and relax,” walk away.Insurance may not cover it fully, but some employee wellness programs do. Companies like Apple, Google, and Microsoft now offer CBT-I through their health benefits. Check your HR portal. If you’re in the UK, the NHS is slowly rolling out digital CBT-I programs like Sleepio through local clinics.
Chronic insomnia isn’t a life sentence. It’s a learned pattern-and like any learned pattern, it can be unlearned. You don’t need more pills. You need better tools. And CBT-I is the only one proven to give you back your nights, your days, and your peace.






Harshit Kansal January 7, 2026
This is the most honest thing I've read about insomnia in years. No fluff, no magic pills, just real science. I tried everything from chamomile tea to sleep masks. None of it stuck. Sleep restriction felt like torture at first, but by week 4 I was actually sleeping through the night. No more 3 a.m. panic sessions.
Isaac Jules January 9, 2026
Of course it works. Everything works if you’re willing to suffer enough. Meanwhile, people are still popping zolpidem like candy and wondering why they’re zombies. CBT-I isn’t ‘therapy’-it’s behavioral boot camp. If you can’t handle 2 weeks of exhaustion, maybe you don’t deserve to sleep.
Melanie Clark January 9, 2026
Ive been reading this for 20 minutes and im still not sure if this is a medical article or a cult recruitment script. You say sleep hygiene is useless but then you list 7 rules for your bedroom. So which is it? Are we supposed to trust the science or the ritual? Also why is everyone suddenly obsessed with 65 degrees F? Is that the temperature of heaven? I think this is all just corporate sleep industry propaganda designed to sell apps and therapy sessions. I used to have insomnia and i just stopped caring. Now i sleep fine. Maybe the answer is nihilism.
Cam Jane January 10, 2026
YES. This. I was skeptical too. Thought CBT-I was just another wellness fad. But I did the 8-week program through my employer’s health plan. Week 1: I cried. Week 3: I almost quit. Week 6: I fell asleep watching Netflix on the couch. Week 8: I woke up at 6:30 a.m. without an alarm and didn’t want to go back to bed. It’s not about willpower. It’s about rewiring. You’re not broken-you’re just stuck in a loop. And this breaks it. Thank you for writing this.
Stuart Shield January 10, 2026
There’s something deeply poetic about the idea that sleep isn’t something you chase-it’s something you stop fighting. Like trying to hold water in your fists. The harder you grip, the more slips away. CBT-I teaches you to open your hands. Not to force sleep, but to make space for it. I used to lie there like a soldier on watch, counting every breath. Now? I just let the night carry me. It’s not magic. It’s mercy.
Mukesh Pareek January 10, 2026
While the framework presented is methodologically sound, it lacks critical consideration of neuroendocrine dysregulation as a primary etiological factor. The stimulus control protocol, while aligned with behavioral conditioning paradigms, fails to account for cortisol rhythm abnormalities and GABAergic downregulation in chronic insomnia phenotypes. A more integrative model incorporating polysomnographic biomarkers and HPA axis modulation is required for longitudinal efficacy.
Jeane Hendrix January 11, 2026
Wait so if I'm sleeping 4.5 hours and i restrict to 4.5 hours... does that mean i have to stay awake for 19.5 hours? That sounds like a recipe for a nervous breakdown. I tried this for 3 days and i started hallucinating my cat talking to me. I think i need meds after all. Also i think the app is tracking my sleep wrong because it says i was awake at 2:17 but i was definitely asleep. Or was i? I don't know anymore.
Tom Swinton January 13, 2026
I just want to say thank you for writing this. I’ve been suffering for 7 years. I’ve seen 12 doctors, tried 5 different meds, slept on 3 different mattresses, bought a $300 pillow that did nothing, and cried in the shower more times than I can count. CBT-I was the first thing that didn’t make me feel like a failure. The sleep restriction part? Yeah, I hated it. But I stuck with it because I had nothing left to lose. And now? I wake up without dread. I don’t check the clock. I don’t panic. I just... sleep. And that’s worth every second of those brutal first weeks. You’re not alone. Keep going.
Tiffany Adjei - Opong January 14, 2026
So let me get this straight-you’re telling me the solution to chronic insomnia is to force yourself to be sleep-deprived for two weeks and then magically your brain gets smarter? And you’re not even going to mention that this only works for people with privilege? People who can afford to take time off work, who don’t have kids, who aren’t working two jobs? Meanwhile, my cousin works night shifts, has PTSD, and can’t even afford a white noise machine. This isn’t science. It’s a luxury wellness fantasy.
Lily Lilyy January 15, 2026
You are not alone. You are not broken. You are not weak. I know how hard this is. I’ve been there. And I’m telling you-it gets better. Not because of magic. Not because of pills. But because you are strong enough to try something that feels impossible. One step. One night. One quiet moment. You’ve already done more than you think. Keep going. You’ve got this.
Venkataramanan Viswanathan January 16, 2026
As someone from India, I’ve seen how mental health is treated here-ignored, stigmatized, or sold as a ‘spiritual cleanse.’ This article is a rare beacon. CBT-I isn’t Western medicine-it’s human science. My sister tried it after 10 years of insomnia. She didn’t need pills. She needed structure. She needed to stop blaming herself. Now she teaches yoga and sleeps like a baby. This isn’t just treatment. It’s liberation.