Every year, millions of people with asthma face worse symptoms not because their medication stopped working, but because the air they breathe is getting worse. Air pollution doesn’t just irritate your lungs-it actively triggers asthma attacks, sends more people to the ER, and makes daily life harder. If you or someone you care for has asthma, reducing exposure to polluted air isn’t optional. It’s essential.
How Air Pollution Makes Asthma Worse
Asthma isn’t just about allergies or genetics. One of the biggest drivers of flare-ups is outdoor air pollution. The main culprits are tiny particles called PM2.5 and PM10, nitrogen dioxide from car exhaust, ground-level ozone on hot days, and sulfur dioxide from industrial smokestacks. These pollutants don’t just hang in the air-they get deep into your lungs, inflame your airways, and make them hyper-sensitive.
Studies show that even short-term spikes in pollution lead to more asthma attacks. In a 2024 study published in PubMed, people with asthma who got real-time alerts about high pollution days saw their asthma control scores improve by over 15% in just eight weeks. That’s not a small change-it means fewer rescue inhaler uses, less missed work or school, and fewer trips to the hospital.
During the pandemic lockdowns, when traffic and industrial activity dropped, researchers saw something remarkable: asthma control scores jumped. Hospital visits for asthma dropped by nearly 40% in some cities. This wasn’t luck. It was proof that when pollution goes down, asthma gets better.
Check the Air Quality Index-Before You Step Outside
The easiest way to protect yourself is simple: check the Air Quality Index (AQI) before heading out. You don’t need a fancy app. The EPA’s AirNow.gov site gives you real-time data for your zip code, and it’s free.
Here’s what the numbers mean for asthma:
- AQI 51-100 (Moderate): Sensitive groups-like asthma patients-should cut back on long outdoor workouts.
- AQI 101-150 (Unhealthy for Sensitive Groups): Everyone with asthma should limit time outside, especially during peak traffic hours.
- AQI 151-200 (Unhealthy): Avoid prolonged outdoor activity. Even walking the dog can trigger symptoms.
- AQI 201+ (Very Unhealthy to Hazardous): Stay indoors. Close windows. Turn on your air purifier.
Many people check the weather-but few check the air quality. That’s a mistake. One user on the American Lung Association’s forum said her daughter’s rescue inhaler use dropped by 45% after she started using the AirVisual app to plan walks and outdoor playtime. It’s not magic. It’s strategy.
Make Your Home a Safe Zone
Indoor air can be just as bad as outdoor air-sometimes worse. Cooking, cleaning products, dust mites, and even outdoor pollution that sneaks in through windows can build up inside. The key is filtration.
Not all air purifiers are created equal. Look for one with a HEPA filter. True HEPA filters capture 99.97% of particles as small as 0.3 microns-exactly the size of the worst asthma triggers. For your HVAC system, use a filter with a MERV rating of 13 to 16. That’s the sweet spot between trapping pollutants and not restricting airflow too much.
For portable units, match the Clean Air Delivery Rate (CADR) to your room size. For a 300-square-foot bedroom, you need a CADR of at least 200. A too-small purifier won’t help. A too-big one wastes money and energy.
One 2021 Johns Hopkins study found homes with HEPA filters had 55-67% lower indoor PM2.5 levels than homes without them. That’s the difference between needing an inhaler every night and sleeping through the night.
But here’s the catch: 57% of people don’t replace their HEPA filters on time. Most filters need changing every 3 to 6 months. A clogged filter doesn’t clean-it just becomes a dust trap. Set a reminder on your phone. It’s that simple.
What About N95 Masks?
During wildfire season or high pollution days, you might think an N95 mask is your best bet. And yes, it can help-if worn correctly.
N95 masks block 95% of airborne particles, but only if they seal tightly to your face. Many people wear them loosely, or kids can’t keep them on. Dr. John Balmes from UCSF warns that masks can give a false sense of safety, especially for children. If the mask slips, it’s useless.
They’re useful for short outdoor trips-like walking to the car or picking up groceries-but not for all-day use. They’re also uncomfortable for long periods. For most people, staying indoors with clean air is better than trying to breathe through a mask all day.
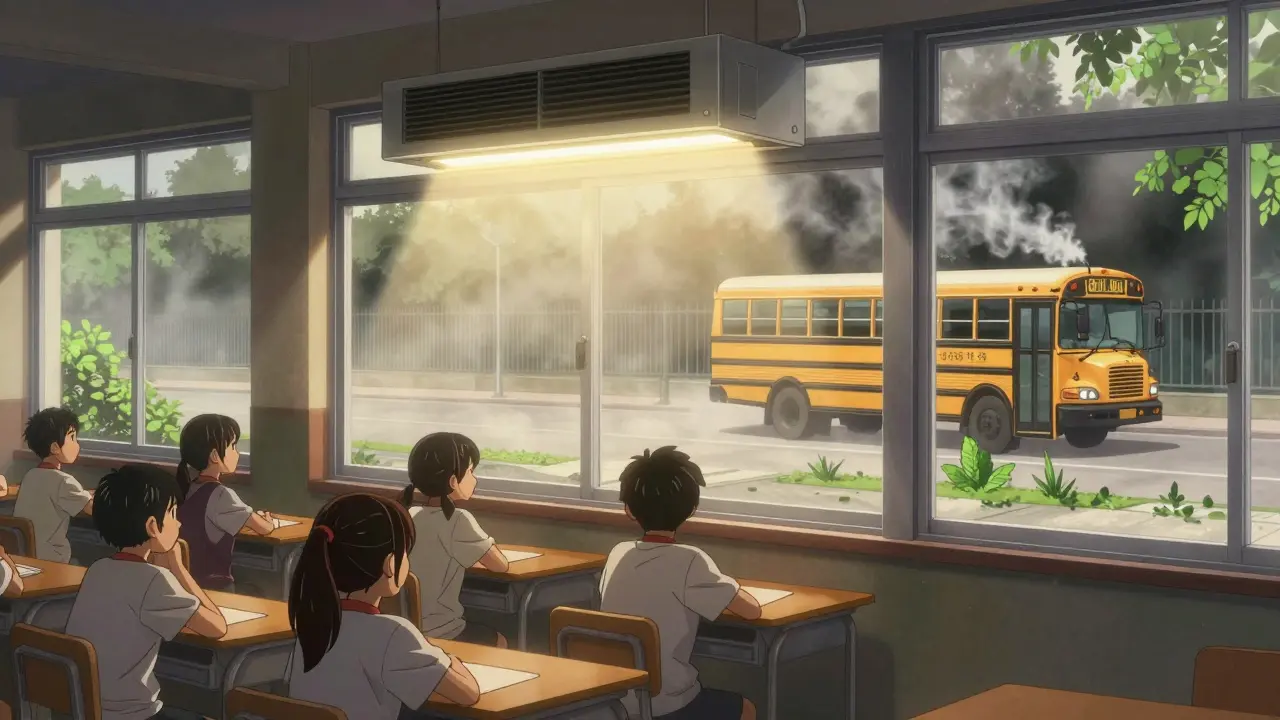
Schools and Workplaces Need Action Too
Most asthma attacks in children happen at school. Why? Because schools are often built near busy roads, and buses idle outside classrooms. In Massachusetts, schools that moved bus parking 500 feet away from playgrounds and banned idling saw indoor PM2.5 levels drop by 22-35%. Asthma-related absences fell by 41%.
Parents can push for change. Ask your child’s school if they follow the Massachusetts School Air Quality Checklist. It’s free, easy to use, and includes simple steps like:
- Keeping windows closed during high pollution days
- Using HEPA filters in classrooms
- Not allowing buses to idle near entrances
At work, talk to your HR department about indoor air quality. The CDC recommends keeping humidity between 30% and 50% to prevent mold and dust mites. A basic dehumidifier costs $100-$300 a year to run-and it’s cheaper than asthma medications.
Why Individual Efforts Aren’t Enough
It’s tempting to think if you just filter your air, avoid traffic, and wear a mask, you’re safe. But here’s the hard truth: if the air outside is toxic, your home will still get polluted.
California researchers found that even with windows closed and HVAC on recirculation, indoor PM2.5 levels reach 60-80% of outdoor levels within an hour during wildfires. No filter can keep up with that kind of influx.
That’s why policy matters. The EPA’s current PM2.5 standard is 12 μg/m³ annually. But the American Thoracic Society says it should be 8 μg/m³ to truly protect asthma patients. In 2024, the EPA proposed lowering it to 9-10 μg/m³-still not enough.
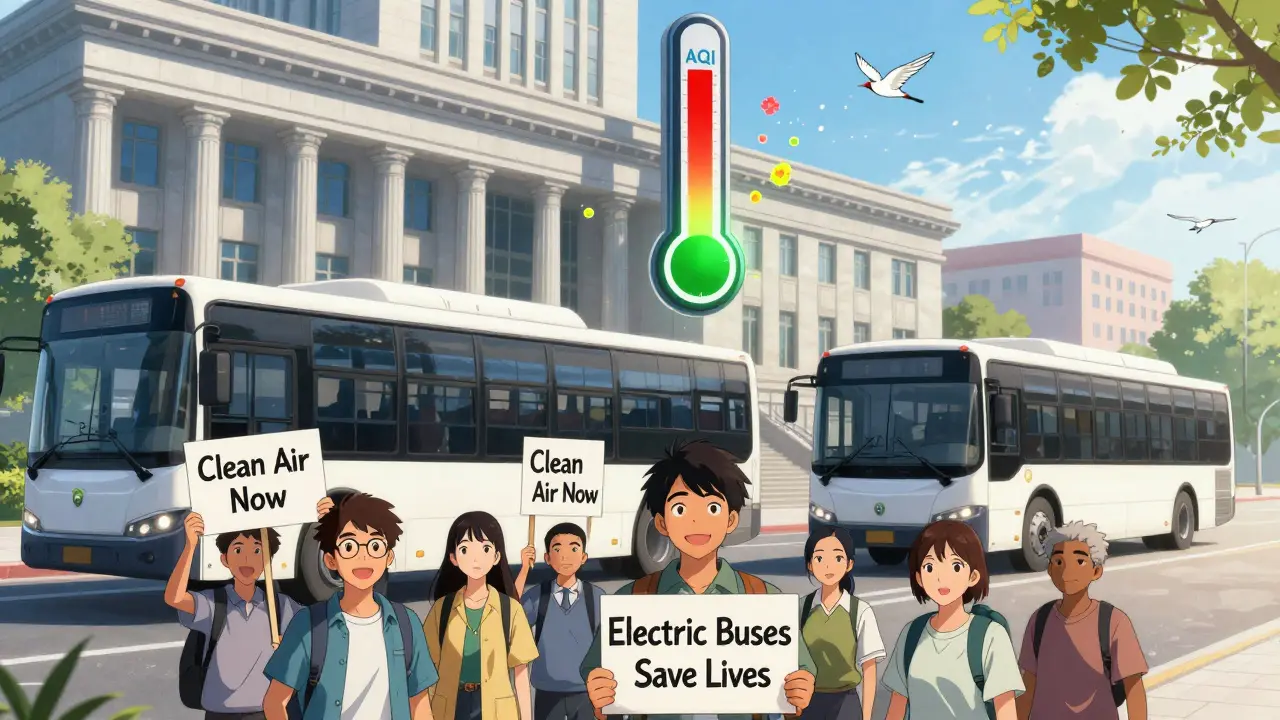
Meanwhile, cities like London have shown what real change looks like. After launching its Ultra Low Emission Zone, childhood asthma hospitalizations dropped by nearly 12% in just two years. California is replacing all its diesel school buses with electric ones by 2035. That’s expected to cut kids’ exposure to traffic pollution by 60%.
Individual actions save lives. But systemic change saves millions.
What Works Best-And What Doesn’t
Not every solution is worth your time or money. Here’s what the data says:
| Strategy | Effectiveness | Cost | Ease of Use |
|---|---|---|---|
| AQI alerts + behavior change | High (15%+ improvement in asthma control) | Free | Easy |
| HEPA air purifiers | Very High (55-67% PM2.5 reduction) | $50-$800 + $20-$100/year in filters | Moderate (requires maintenance) |
| N95 masks | Moderate (only if fitted properly) | $1-$3 per mask | Hard (poor compliance, especially in kids) |
| School anti-idling policies | High (22-35% indoor PM2.5 drop) | Free | Requires advocacy |
| Electric school buses | Very High (up to 60% exposure reduction) | High upfront cost, low long-term cost | Policy-driven |
The best approach? Combine them. Use AQI alerts to know when to stay inside. Run a HEPA filter in your bedroom. Push your school to stop idling buses. Support clean air policies. Together, they add up.
Getting Started: Your 7-Day Action Plan
You don’t need to fix everything at once. Here’s a realistic plan:
- Day 1: Go to AirNow.gov. Bookmark it. Check the AQI daily.
- Day 2: Buy one HEPA filter for your bedroom if you don’t have one. Look for CADR ≥ 200 for rooms under 300 sq ft.
- Day 3: Set a phone reminder to check your air purifier filter. Replace it if it’s been 3 months.
- Day 4: Call your child’s school. Ask if they have an air quality plan. If not, ask how to start one.
- Day 5: Avoid running the stove fan or opening windows when AQI is over 100.
- Day 6: Talk to your doctor about your exposure. Ask if your asthma action plan includes pollution triggers.
- Day 7: Sign up for a local clean air group. Change doesn’t happen alone.
It’s not about perfection. It’s about progress. Even small changes-like checking the AQI before taking a walk-can make a real difference.
What’s Next? The Future of Asthma and Air Quality
Scientists are now testing wearable sensors that track your personal exposure to pollution and send alerts to your phone. The NIH is funding pilot programs that connect air quality data directly to electronic health records-so your doctor knows when pollution spikes and can adjust your treatment.
But technology alone won’t fix this. We need stronger rules on emissions, cleaner public transit, and better urban planning. Every electric bus, every closed factory chimney, every tree planted near a school is a step toward cleaner air.
And if you have asthma-you’re not just a patient. You’re part of the solution. When you speak up, when you demand clean air, when you choose better filters and push for change-you’re not just protecting yourself. You’re protecting everyone with lungs.
Can air pollution cause asthma in people who never had it before?
Yes. A 2019 study in The Lancet Planetary Health found that air pollution contributes to about 4 million new pediatric asthma cases every year worldwide. Children exposed to high levels of traffic pollution, especially in the first few years of life, are at higher risk of developing asthma even if they have no family history.
Are air purifiers worth the cost?
For people with asthma, yes. A 2021 Johns Hopkins study showed HEPA filters reduce indoor PM2.5 by 55-67%. That translates to fewer nighttime symptoms, less inhaler use, and better sleep. A good unit costs $200-$500, with $20-$100 in annual filter replacements. Compared to emergency room visits or missed work, it’s one of the most cost-effective health investments you can make.
Should I use an air purifier in my child’s bedroom?
Absolutely. Children’s lungs are still developing, and they breathe more air per pound of body weight than adults. A HEPA filter in their bedroom can cut nighttime coughing and wheezing. Look for a quiet model with a CADR rating matched to the room size. Avoid ionizers or ozone generators-they can worsen asthma.
Does living near a highway increase asthma risk?
Yes. Studies show people living within 500 feet of a major highway have up to a 30% higher risk of asthma attacks. Traffic pollution includes ultrafine particles and nitrogen dioxide, both strong asthma triggers. Schools and homes should be built at least 500 feet away from busy roads. If you already live nearby, use HEPA filters, keep windows closed during rush hour, and avoid outdoor play during peak traffic times.
Can climate change make air pollution worse for asthma?
Yes. Warmer temperatures increase ground-level ozone, which spikes on hot, sunny days. Wildfires, made worse by drought and heat, release massive amounts of PM2.5. The American Public Health Association warns that without action, ozone-related asthma cases could rise 10-15% by 2050. Reducing fossil fuel emissions is the only long-term solution.
Is it safe to exercise outdoors with asthma?
It depends on the air quality. On days with AQI under 50, outdoor exercise is generally safe. Between 51-100, limit intense activity. Above 101, avoid prolonged outdoor workouts. Morning hours often have cleaner air than afternoon. Always carry your rescue inhaler. If you notice symptoms during exercise, stop and go indoors.
What’s the best way to reduce pollution exposure at work?
If you work indoors, ask your employer to upgrade HVAC filters to MERV 13 or higher. Avoid sitting near windows on high-pollution days. If you work outside, check the AQI daily and reschedule heavy tasks for low-pollution hours. Use a portable air purifier if possible. If you’re in a high-risk job like construction, talk to your union or safety officer about air quality protections.