Anaphylaxis Symptom Checker
Test your symptoms against medical criteria for medication-induced anaphylaxis. This tool is not a diagnosis but can help identify when immediate medical attention is needed.
Check Your Symptoms
Select any symptoms you're experiencing after taking a medication:
What to do next
This symptom combination matches anaphylaxis criteria. Please call 911 immediately and seek emergency medical help.
Possible anaphylaxis
This symptom combination could indicate anaphylaxis. Call 911 immediately and give epinephrine if you have it.
Low risk of anaphylaxis
Symptoms do not match anaphylaxis criteria. However, if symptoms worsen or you experience breathing difficulties, seek medical attention immediately.
What Anaphylaxis Really Looks Like When It’s Caused by Medication
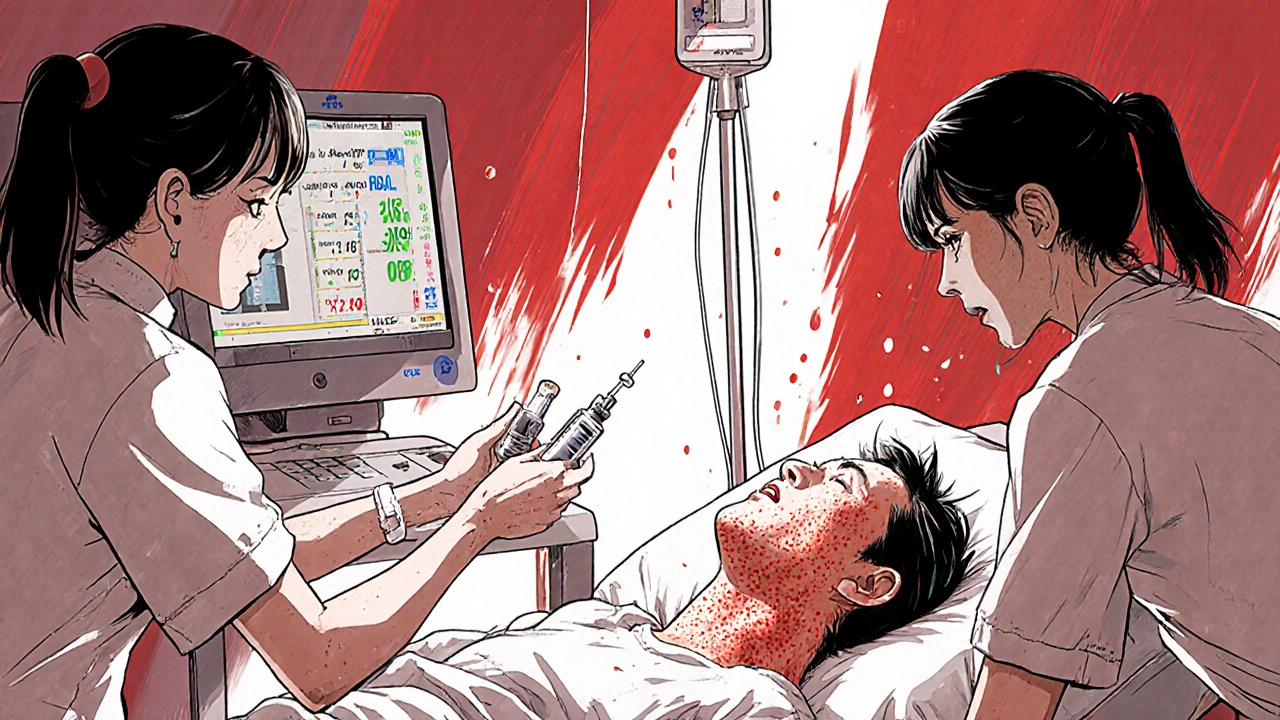
It starts fast. One minute you’re fine. The next, your throat feels tight, your skin breaks out in hives, and your chest feels like it’s being crushed. This isn’t anxiety. It’s not a panic attack. It’s anaphylaxis - a life-threatening allergic reaction triggered by a medication you just took. And if you don’t act within minutes, it can kill you.
Medications are the third most common cause of anaphylaxis, behind foods and insect stings. But unlike food reactions, which often happen at home, drug-induced anaphylaxis can strike anywhere - in a hospital, a clinic, or even after you’ve swallowed a pill at home. The problem? Many people, even doctors, miss the signs at first. Symptoms get blamed for something else: a drop in blood pressure? Must be dehydration. Trouble breathing? Must be asthma. Skin rash? Probably just a side effect.
Here’s the truth: anaphylaxis from medication doesn’t wait. It hits hard and fast. And knowing the exact signs - not just the textbook ones, but the real-world ones - can save your life or someone else’s.
The Four Systems That Give It Away
Anaphylaxis doesn’t just affect one part of your body. It hits multiple systems at once. The American Academy of Allergy, Asthma & Immunology (AAAAI) says you’re likely having anaphylaxis if you meet any of these three criteria after taking a drug:
- Skin or mucosal changes (hives, swelling, itching) plus trouble breathing or low blood pressure
- Two or more systems affected - skin, lungs, heart, gut - after drug exposure
- Low blood pressure after exposure to a drug you know you’re allergic to
Let’s break down what each system looks like in real time.
Skin and mucous membranes: This is the most obvious sign - but not always present. About 72% of medication-induced cases show hives, flushing, or swelling. But here’s the catch: 1 in 5 people have NO skin symptoms at all. Swelling of the lips, tongue, or throat can happen without any rash. That’s why you can’t wait for the rash to appear.
Respiratory: This is where things turn dangerous fast. Wheezing, shortness of breath, a feeling of your throat closing, or hoarseness aren’t normal side effects. They’re emergency signals. In medication-induced cases, wheezing happens in 71% of reactions - higher than with food triggers. If you’re on an IV drip and suddenly can’t catch your breath, don’t wait. Call for help.
Cardiovascular: This is the silent killer. Low blood pressure doesn’t always mean you feel dizzy. Sometimes you just feel weird - cold, clammy, nauseated, or confused. Your pulse may race, then weaken. In hospital settings, this is often mistaken for a vasovagal reaction (fainting) or sepsis. But if it comes on within minutes of a drug being given, and you have other symptoms, it’s anaphylaxis.
Gastrointestinal: Nausea, vomiting, cramps, or diarrhea can happen, especially with oral medications. But alone, these aren’t enough to diagnose anaphylaxis. They become critical when paired with breathing or circulation problems.
Which Medications Are Most Likely to Trigger It?
Not all drugs carry the same risk. Some are far more dangerous than others. Here’s what the data shows:
- Antibiotics (69% of drug reactions): Penicillin and related drugs like amoxicillin are the biggest culprits. If you’ve ever had a rash after penicillin, assume you’re allergic - even if it was years ago. Many people outgrow food allergies, but drug allergies often stick.
- NSAIDs (15%): Ibuprofen, naproxen, aspirin. These aren’t classic allergens like penicillin, but they can still trigger severe reactions by bypassing the immune system in a different way. People with asthma or nasal polyps are at higher risk.
- Monoclonal antibodies (6%): Drugs like rituximab, cetuximab, and trastuzumab (used in cancer and autoimmune diseases) are growing in use - and so are reactions. These are often given in hospitals, but the first dose can be deadly if not monitored.
- Chemotherapy agents (4%): Platinum-based drugs like cisplatin can cause anaphylaxis. The reaction might be delayed - up to 6 hours - which makes it harder to connect to the drug.
- IV contrast (dyes for scans): Often mistaken for an allergic reaction, but it’s not always true anaphylaxis. Still, it can kill, and the treatment is the same.
Here’s a key point: you don’t need to have had a reaction before to have anaphylaxis on the first dose. Many people have no history of drug allergies. That’s why hospitals monitor patients for 15-30 minutes after high-risk drugs.
Why Epinephrine Is the Only Thing That Stops It
There is no other treatment that works like epinephrine. Antihistamines? They help with itching and hives. Steroids? They prevent delayed reactions. But neither stops the drop in blood pressure or the swelling of the airway.
Epinephrine works by tightening blood vessels, opening airways, and stopping the runaway immune response. And it has to be given fast. The AAAAI says: if symptoms start, give epinephrine within 5 to 15 minutes. Delay it beyond 30 minutes, and your risk of death triples.
Here’s how to give it right:
- Use an auto-injector (like EpiPen or Adrenaclick) in the middle of the outer thigh. Even through clothing.
- Hold it in place for 3 seconds.
- Call 911 immediately - even if you feel better. Symptoms can come back.
78% of fatal cases involve no epinephrine at all. 34% of patients in hospitals never get it because staff misdiagnose the reaction. Don’t be one of them. If you’re unsure, give it anyway. It’s safe. Even if you’re wrong, it won’t hurt you.
What Hospitals Are Doing to Prevent It
It’s not just about recognizing the reaction - it’s about stopping it before it starts.
Johns Hopkins Hospital cut anaphylaxis cases by 47% by creating an Allergy Alert System. When a patient’s chart says “penicillin allergy,” the system blocks all related drugs, flags the record, and reminds staff to double-check. That’s simple, but it works.
The Joint Commission now requires all accredited hospitals to have an anaphylaxis protocol by January 2024. That means:
- Epinephrine must be available in every treatment area - not just the ER.
- Staff must be trained annually on recognition and treatment.
- Allergy histories must be documented clearly - not buried in notes.
But here’s the problem: 63% of medication errors happen because the allergy info is missing or wrong in electronic records. A patient says they’re allergic to penicillin - but no details. Was it a rash? A throat swelling? A drop in blood pressure? The difference matters. A mild rash doesn’t mean you’re at risk for anaphylaxis. But if you’ve ever had trouble breathing after a drug, that’s a red flag.
What You Can Do Right Now
If you’ve ever had a reaction to a medication - even a mild one - get it documented properly. Don’t just say “I’m allergic to penicillin.” Say: “I had hives and swelling of the tongue after amoxicillin in 2018.”
Ask for an allergy card or app reminder. Some pharmacies offer free wallet cards that list your drug allergies.
If you’ve had anaphylaxis before, you should have two epinephrine auto-injectors with you at all times. Insurance often covers them. If cost is an issue, ask your doctor about generic brands or patient assistance programs. A $500 auto-injector is cheaper than an ICU stay.
Teach your family how to use it. Most reactions happen outside the hospital. If you collapse, your spouse or child needs to know how to give the shot.

Common Mistakes That Cost Lives
Doctors and nurses aren’t the only ones who misread these signs. Patients do too.
Mistake 1: “I had a rash once, so I’m allergic to all antibiotics.” Not true. You might only be allergic to one specific drug. Get tested if you’re unsure.
Mistake 2: “I felt weird after the IV, but I thought it was nerves.” Nerves don’t cause your tongue to swell or your blood pressure to crash.
Mistake 3: “I took this drug before and was fine.” That doesn’t mean you’re safe. Allergies can develop after repeated exposure. You can be fine on the first ten doses - and react on the eleventh.
Mistake 4: “I didn’t get epinephrine, so I’m fine now.” Symptoms can return hours later. That’s called a biphasic reaction. You need to be observed for at least 4-6 hours after the reaction.
What to Do After a Reaction
Surviving anaphylaxis is only half the battle. The next step is prevention.
- See an allergist. They can test you to find exactly which drug caused it.
- Get a medical alert bracelet. It saves lives when you can’t speak for yourself.
- Make sure your primary care doctor, dentist, and pharmacist all have your updated allergy list.
- Ask if you can be desensitized. For some drugs - like chemotherapy or essential antibiotics - you can be slowly exposed under medical supervision to build tolerance.
And if you were never given an epinephrine auto-injector after your reaction? Demand one. A 2022 survey found over half of patients left the hospital without one. That’s unacceptable. You’re at higher risk for another reaction - and next time, you might not survive.
Final Thought: Speed Saves Lives
Anaphylaxis from medication doesn’t care if you’re young, healthy, or have never had an allergy before. It doesn’t wait for a diagnosis. It acts in seconds.
Knowing the signs - skin, breathing, circulation, gut - gives you power. Having epinephrine gives you a chance. Acting fast gives you life.
Don’t wait for the textbook symptoms. Don’t wait for a doctor to confirm it. If you think it’s anaphylaxis - give epinephrine. Call 911. Save a life. Yours or someone else’s.






Brian Bell November 14, 2025
Bro this is legit life-saving info. I had no idea NSAIDs could do this. Just got my EpiPen refill today after reading this. 🙌
Nathan Hsu November 15, 2025
In India, we don't have EpiPens everywhere... but I've seen people react to antibiotics at roadside clinics. This article is so important. Please, if you're a doctor, listen. If you're a patient, know your history. Don't ignore that rash. Don't blame it on stress. It could be the start of death.
Ashley Durance November 16, 2025
The data here is mostly anecdotal. 72% skin involvement? Where's the peer-reviewed source? And you say 'many people outgrow food allergies'-that’s misleading. Only 20% of peanut allergies resolve. Also, epinephrine isn't 'safe' if you have undiagnosed cardiomyopathy. You're dangerously oversimplifying.
Scott Saleska November 17, 2025
Hey, I'm a nurse in Ohio and I see this all the time. People come in saying 'I'm allergic to penicillin' and they got a rash when they were 8. But then they get Cipro and go into shock-because they never got tested. You're right about the records being messed up. My hospital has a form now where you have to write the exact symptom, date, and drug. It's a pain, but it saves lives. Also, epinephrine isn't just for the ER-my unit has it in every med cart now.
Ryan Anderson November 18, 2025
This is one of the most important posts I’ve read this year. 🩺❤️ I had a reaction to ibuprofen last year-swelling, throat tightness, but no rash. They thought it was a virus. I’m now carrying two EpiPens. I taught my 12-year-old how to use them. If you’re reading this and you’ve ever felt ‘weird’ after a drug-don’t brush it off. Get tested. Get the auto-injector. You’re not being dramatic. You’re being smart.
Eleanora Keene November 18, 2025
I just wanted to say thank you for writing this. My mom had anaphylaxis after a CT scan dye and they didn’t give her epinephrine right away. She’s okay now, but she’s got the bracelet, the cards, the two pens. I’m so glad you’re spreading this info. If you’re reading this and you’re scared to ask for a prescription-please do. It’s not a luxury. It’s like a fire extinguisher. You hope you never need it… but you’re glad it’s there.
Joe Goodrow November 19, 2025
Why are we letting foreigners dictate our medical protocols? We don't need some fancy Johns Hopkins program. We need common sense. If you're allergic, don't take the drug. Simple. Stop overcomplicating it with apps and cards and training. Americans are too soft. Just say no.
Don Ablett November 21, 2025
The statistical prevalence figures presented are compelling, particularly the 69% attribution to antibiotics. However, the absence of confidence intervals or study design details in the source material precludes robust validation. Furthermore, the assertion that epinephrine is universally safe without contraindications warrants caution, given documented cases of arrhythmia in patients with preexisting cardiac conditions. A more nuanced discussion of risk stratification would enhance clinical utility.