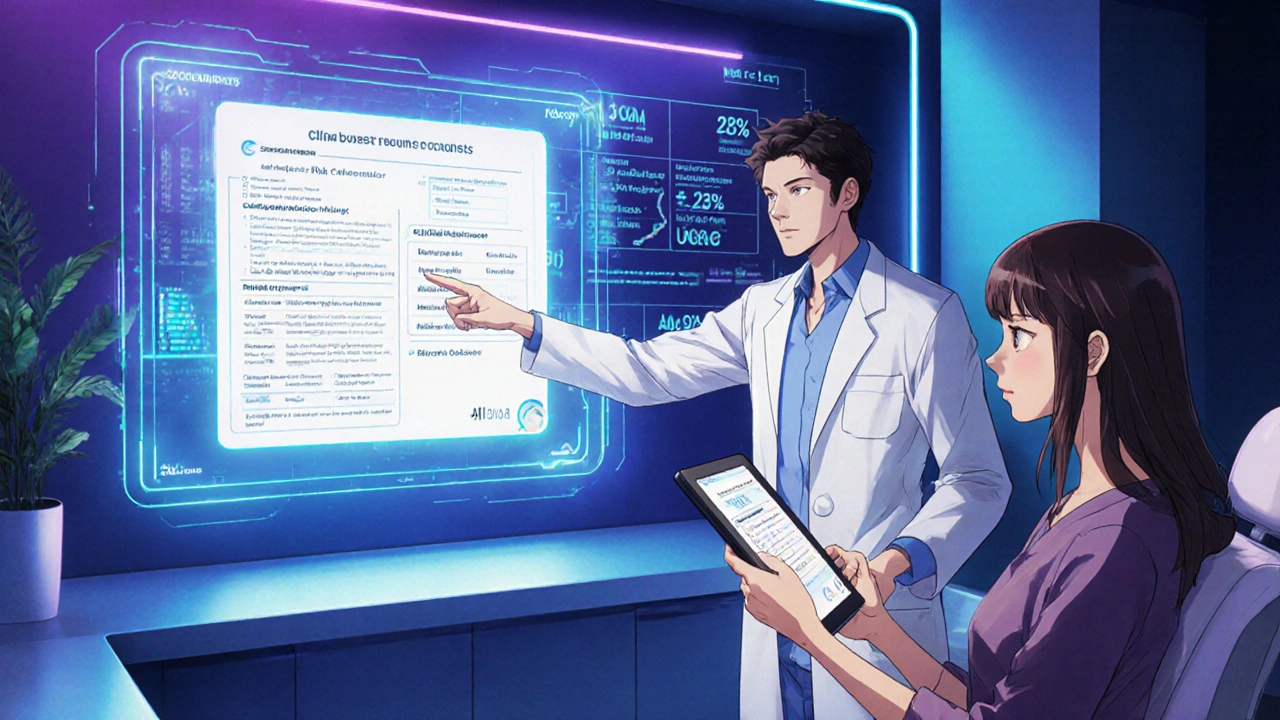
When a treatment promises big benefits but also carries a bundle of possible side effects, patients often feel stuck. Shared Decision-Making (SDM) is a collaborative conversation where clinicians and patients weigh those benefits against the risks, values, and everyday impact of the therapy. Adding a clear script to the mix turns vague talk into an actionable roadmap, helping patients see exactly which side effects matter most to them.
Why SDM matters for side‑effect trade‑offs
Research from the Massachusetts General Hospital Health Decision Sciences Center (2023) shows a 23% drop in decisional conflict when structured SDM is used for high‑risk meds. In oncology, a 2021 JAMA Internal Medicine trial found a 29% reduction in treatment discontinuation after patients received a side‑effect script. These numbers aren’t just statistics - they translate into fewer ER visits, lower costs, and higher patient trust.
- Patients who hear absolute risk numbers (e.g., “15% chance of nausea”) are 37% more likely to understand the trade‑off (Annals of Internal Medicine, 2019).
- Clinicians who spend an average of 7.3 extra minutes on SDM see a 22% cut in follow‑up visits for side‑effect management (Scripps Health, 2022).
- Medicare’s 2023 requirement for documented SDM on high‑risk meds has already boosted adoption by 41% year‑over‑year (KLAS Research).
Core frameworks you can borrow
Two evidence‑based models dominate the field. Both can be adapted into scripts, but they differ in flow.
| Aspect | SHARE Approach (AHRQ) | Three‑Talk Model (AAFP) |
|---|---|---|
| Number of steps | 5 (Seek, Help, Assess, Reach, Evaluate) | 3 (Option Talk, Choice Talk, Decision Talk) |
| Typical use | Broad, multi‑condition settings | Complex, high‑risk decisions (e.g., chemotherapy) |
| Risk framing guidance | Absolute numbers, visual aids | Numerical framing plus values clarification |
| Clinician time impact | +7‑8 min per encounter | +5‑6 min on average |
Both frameworks stress three non‑negotiable ingredients: unbiased evidence, clinician communication skill, and patient values. Choose the one that fits your workflow and specialty.
Building an effective SDM script
Below is a step‑by‑step checklist that works with either model. Each bullet can be turned into a line of a script or a slide in a decision aid.
- Set the stage. "I want to make sure we look at both how this medication can help you and the side effects you might experience. Does that sound okay?"
- Present options with absolute risk. "Option A reduces your blood pressure by an average of 12 mmHg. About 15 % of people feel dizziness, while 85 % do not."
- Ask about personal priorities. "Which side effect would be a deal‑breaker for you? Fatigue, nausea, or something else?"
- Explore trade‑offs. "If we choose Option A, you might need to avoid driving for the first 48 hours because of dizziness. Option B has less dizziness but a 20 % chance of muscle aches. How does that fit with your daily routine?"
- Summarize the shared understanding. "So you’re comfortable with a small chance of dizziness if it means better blood‑pressure control, and you’d like a plan for managing any muscle aches."
- Document the decision. Record the risk thresholds and patient‑stated preferences in the EHR (American Medical Association, 2022).CPT code 96170 covers documentation of SDM encounters.
- Plan follow‑up. "We’ll check in two weeks to see how you’re feeling and adjust if needed."
Feel free to tweak the wording to match your voice, but keep the structure intact.
Practical examples by specialty
Oncology - chemotherapy selection
Script snippet (Three‑Talk Model):
Option Talk: “Drug X gives a 30 % chance of tumor shrinkage but carries a 5 % risk of severe nausea. Drug Y offers a 20 % chance of shrinkage with a 2 % risk of neuropathy.” Choice Talk: “Which risk feels more manageable for you?” Decision Talk: “Based on what you’ve told me, we’ll start with Drug X and have an anti‑nausea plan in place.”
Cardiology - statin therapy
Script snippet (SHARE):
Help: “Statins lower your heart‑attack risk by about 25 %. Muscle aches happen in roughly 10 % of patients.” Assess: “Are muscle aches something you’d find unacceptable?” Reach: “If we start a low‑dose statin and monitor your muscles, does that sound okay?”
Primary care - anticoagulant choice
Script snippet (combined):
Seek: “You’re on a blood thinner, so let’s talk about how it protects you and the bleeding risk.” Help: “Warfarin requires blood tests; direct oral anticoagulants have a 3‑5 % bleed risk but no routine labs.” Assess: “Do routine blood draws bother you?” Reach: “We’ll choose the oral option and set up a follow‑up in a month.”
Implementation tips that save time
Even the best script can feel like a burden if you’re rushed. Here are proven shortcuts:
- Pre‑visit decision aid. Send a short video or one‑page PDF a few days before the appointment. Studies show a 3.2‑minute reduction in in‑visit conversation time (Scripps Health).
- Role‑play training. Four‑hour workshops at MGH achieve proficiency after 12 supervised cases (2023). Pair junior and senior clinicians for peer coaching.
- EHR templates. Epic’s SDM module (active in 63 % of Epic hospitals) lets you drop a ready‑made script into the note with one click.
- Team delegation. Let nurses or pharmacists run the “Assess” step using a scripted checklist while the physician focuses on “Option Talk.”
Measuring success and getting reimbursed
Analytics turn good intentions into accountability. Track these core metrics:
- Decisional conflict score. Aim for < 25 % post‑visit (scale 0‑100).
- Medication adherence. Look for a 20‑30 % lift in refill rates after SDM implementation.
- Follow‑up visit reduction. Target a 15‑20 % drop in side‑effect‑related calls.
- Reimbursement capture. Use CPT code 96171 for SDM with decision aid documentation and ensure the claim includes the ICD‑10 code for the condition treated.
Report outcomes quarterly to leadership; the data often justifies the extra minutes spent.
Common pitfalls and how to avoid them
Even seasoned clinicians slip into bad habits. Spot them early:
- Over‑scripted, no personalization. Dr. Kaplan warned that rigid check‑boxes can cut satisfaction by 19 %. Insert a patient‑specific question after each scripted line.
- Using relative risk instead of absolute numbers. Patients misinterpret "risk reduced by 50 %" as "only 1 in 10 will get the side effect." Stick to absolute percentages.
- Skipping the treatment‑burden discussion. Forgetting to ask how daily dosing or monitoring fits into life leads to 42 % of regret (MGH, 2022).
- Neglecting documentation. Without a record of the conversation, CMS audits can flag missing SDM compliance.
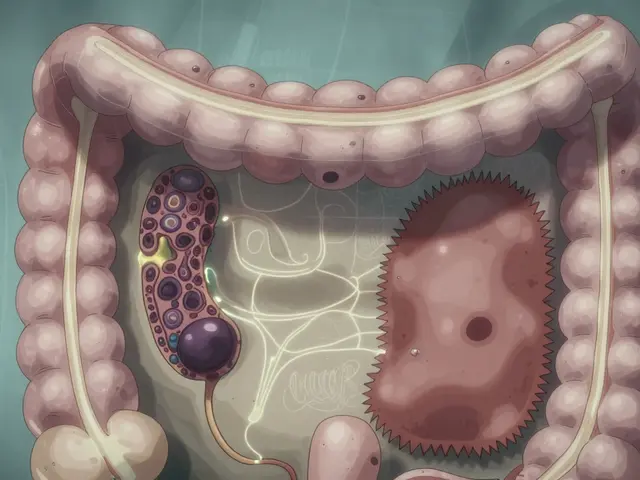
Future directions
AI‑driven conversation analysis is on the horizon. The NIH’s 2023 grant funds tools that flag unspoken worries in real time, letting clinicians pivot instantly. Expect decision‑aid platforms to embed risk calculators that auto‑populate scripts based on patient age, labs, and comorbidities.
Frequently Asked Questions
How long should a side‑effect SDM script take?
On average, clinicians add about 5‑8 minutes. Pre‑visit materials and template use can shave a few minutes off each encounter.
Do I need special training to use these scripts?
A short workshop (2‑4 hours) plus supervised practice on 10‑12 patients is enough to reach proficiency, according to MGH’s program data.
Can I use the scripts for emergency situations?
Full SDM isn’t realistic in acute emergencies. A condensed version that highlights the most critical side effect (e.g., bleeding risk) can still improve consent.
What documentation is required for billing?
Record the patient’s risk thresholds and the decision made. Use CPT 96170 for SDM without a decision aid and CPT 96171 when a validated aid is attached.
How do I choose between SHARE and Three‑Talk?
If your clinic already follows AHRQ’s toolkit, stick with SHARE. For oncology or high‑risk decisions where rapid option comparison is key, the Three‑Talk model often feels lighter.






Monika Pardon October 26, 2025
Oh sure, because the only thing standing between us and perfect health is the big pharma cabal whispering side‑effect scripts into our ears. I guess they’ve finally decided to be transparent, right after they patented the invisible hand. If you trust a script that was drafted by the same people who love to hide adverse events, you might as well hand them your credit card.
Rhea Lesandra October 27, 2025
Hey everyone, love seeing this focus on shared decision‑making! It’s amazing how a clear script can turn confusion into confidence. When you walk a patient through the numbers and ask about their daily priorities, you’re actually giving them the power to shape their own treatment plan. Keep spreading the word – the more clinicians use these tools, the smoother the conversations become.
Kasey Marshall October 28, 2025
Nice summary. The scripts just add a few minutes but save a lot of back‑and‑forth later. It’s a win‑win for patients and providers.
Dave Sykes October 30, 2025
Alright, let’s get into why this matters on the front lines. First, you’ve got the data: a 23% drop in decisional conflict translates into patients feeling less anxious about their choices. Second, those numbers aren’t just abstract – they mean fewer emergency room trips, which saves both time and money. Third, when clinicians take an extra five to eight minutes to run through a script, they often see a 22% reduction in follow‑up visits for side‑effect management. Fourth, Medicare’s recent requirement for documented SDM means that hospitals are already incentivized to adopt these practices. Fifth, using absolute risk numbers like “15% chance of nausea” helps patients grasp the real odds instead of vague “high risk” labels. Sixth, involving nurses or pharmacists in the “Assess” step can offload work from physicians and still keep the conversation patient‑centered. Seventh, pre‑visit decision aids, such as a one‑page PDF, shave off an average of three minutes from the in‑clinic discussion, making the whole process more efficient. Eighth, role‑play workshops have shown that after just a dozen supervised cases, most clinicians feel comfortable with the script flow. Ninth, the Epic SDM module lets you drop a ready‑made script into the note with a single click, eliminating duplication of effort. Tenth, documenting the conversation using CPT 96170 or 96171 ensures you get reimbursed and stay compliant with CMS audits. Eleventh, tracking metrics like decisional conflict scores, medication adherence, and follow‑up call volume gives you concrete feedback on how well the script is performing. Twelfth, sharing those metrics with leadership can secure ongoing support and resources for the program. Thirteenth, avoiding relative risk phrasing and sticking to absolute percentages prevents misinterpretation. Fourteenth, constantly asking patients about their daily routines and treatment‑burden keeps the plan realistic. Fifteenth, the whole approach builds trust, which ultimately improves long‑term health outcomes. Sixteenth, when patients feel heard and involved, they’re more likely to stick with the therapy, reducing the chance of costly discontinuations. So, in short, those extra minutes are an investment that pays dividends across the board.
Erin Leach October 31, 2025
I totally get how overwhelming a new medication can feel, especially when you’re juggling work, family, and everything else. It’s reassuring to know there’s a structured way to talk about the pros and cons without getting lost in medical jargon. When the clinician asks about what side effects would be a deal‑breaker for you, it really shows they care about your life outside the clinic. I’ve seen patients become more confident after a simple “how would you feel about occasional dizziness?” question. Keep the conversation human – that’s what makes the script work.
Erik Redli November 1, 2025
Hold on a sec, why are we putting more paperwork on already burnt‑out doctors? These scripts sound great on paper but in reality they’re just another checkbox that pharma loves because it gives them a paper trail. You think a five‑minute script will magically fix non‑adherence? The real problem is the cost of the drugs and the system that pushes them, not a nice talking point. If you want to see real change, start by questioning why we’re prescribing these high‑risk meds in the first place.
Paul Luxford November 2, 2025
Sounds solid, thanks.
Manoj Kumar November 3, 2025
Ah, the age‑old dance between science and suspicion – we craft scripts to demystify risk, yet some still whisper that the very act of scripting is a control mechanism. Philosophically, it’s fascinating: we try to quantify the unquantifiable, like how much nausea a person can tolerate before life loses its flavor. Still, I appreciate the attempt to bring clarity; it’s better than leaving patients to guess whether a 5% chance is “big” or “tiny.” Just remember: a script is only as good as the honesty behind it, and a little sarcasm never hurts to keep the conversation lively.
Jay Campbell November 4, 2025
I like how the post breaks down both SHARE and Three‑Talk models without preaching one over the other. It gives us flexibility to pick what fits our workflow, whether we’re in primary care or oncology. The step‑by‑step checklist makes it easy to turn the theory into practice. Looking forward to trying these scripts with my patients and seeing how the numbers shape the dialogue.
Jacqui Bryant November 6, 2025
Great info! I’m excited to try the pre‑visit PDF – looks simple enough. The short, upbeat tone makes it easy to explain to patients.
Nic Floyd November 7, 2025
From a health‑informatics perspective, integrating the SDM module into Epic’s workflow is a game‑changer 🚀. The auto‑populate feature pulls patient age, labs, and comorbidities straight into the risk calculator, so you’re not manually entering data every time. Plus, the standardized template satisfies CMS documentation requirements without extra effort. Just make sure the decision‑aid PDFs are HIPAA‑compliant and hosted on a secure server. Overall, this approach bridges clinical rigor with operational efficiency 🤝.
Johnae Council November 8, 2025
This whole thing sounds like a buzzword fest to me. “Shared decision‑making” is just a fancy way of saying “let's talk more” while still pushing the same meds. The stats are nice, but I bet they cherry‑pick the best outcomes and hide the failures. Honestly, if you really wanted to reduce side‑effects, you’d start by cutting the unnecessary prescriptions, not by adding another script.
Hershel Lilly November 9, 2025
I’m curious about how the decision‑aid videos are received by patients with low health literacy. Do they actually understand the absolute risk numbers, or does the format overwhelm them? It would be useful to see some qualitative feedback alongside the hard metrics. Maybe a short focus group could shed light on the patient experience. Thanks for sharing the resources – they’ll be helpful for our upcoming pilot.
Carla Smalls November 10, 2025
Love the enthusiasm, Jacqui! Your excitement about the pre‑visit PDF really captures the spirit we need to keep patients engaged.