Medication errors are no longer just a quiet concern in hospitals and pharmacies-they’re a national crisis being tackled head-on. In 2025, a wave of new safety data forced major changes across the U.S. and global healthcare systems. These aren’t minor tweaks. They’re full-scale updates to how drugs are prescribed, handled, and tracked-changes that directly affect your doctor’s office, your pharmacy, and ultimately, your safety.
What’s Actually Changing in 2025?
The biggest shifts come from four key sources: the Institute for Safe Medication Practices (ISMP), the Centers for Medicare & Medicaid Services (CMS), the National Institute for Occupational Safety and Health (NIOSH), and the World Health Organization (WHO). Each one targets a different part of the problem.
ISMP’s 2025-2026 Best Practices for Community Pharmacies added six new requirements. The most urgent? Using patient weight to verify dosing for medications like chemotherapy, antibiotics, and pediatric drugs. A single decimal error in weight-based dosing can be fatal. Now, pharmacists must double-check weight entries in electronic records before dispensing. No more guessing. No more skipping steps.
Another big change: independent double checks for high-alert medications. Drugs like insulin, heparin, and opioids now require two trained staff members to verify every step-from order to delivery. This isn’t optional. It’s mandatory for any pharmacy wanting to meet the new safety baseline.
The Hazardous Drugs List Got a Major Update
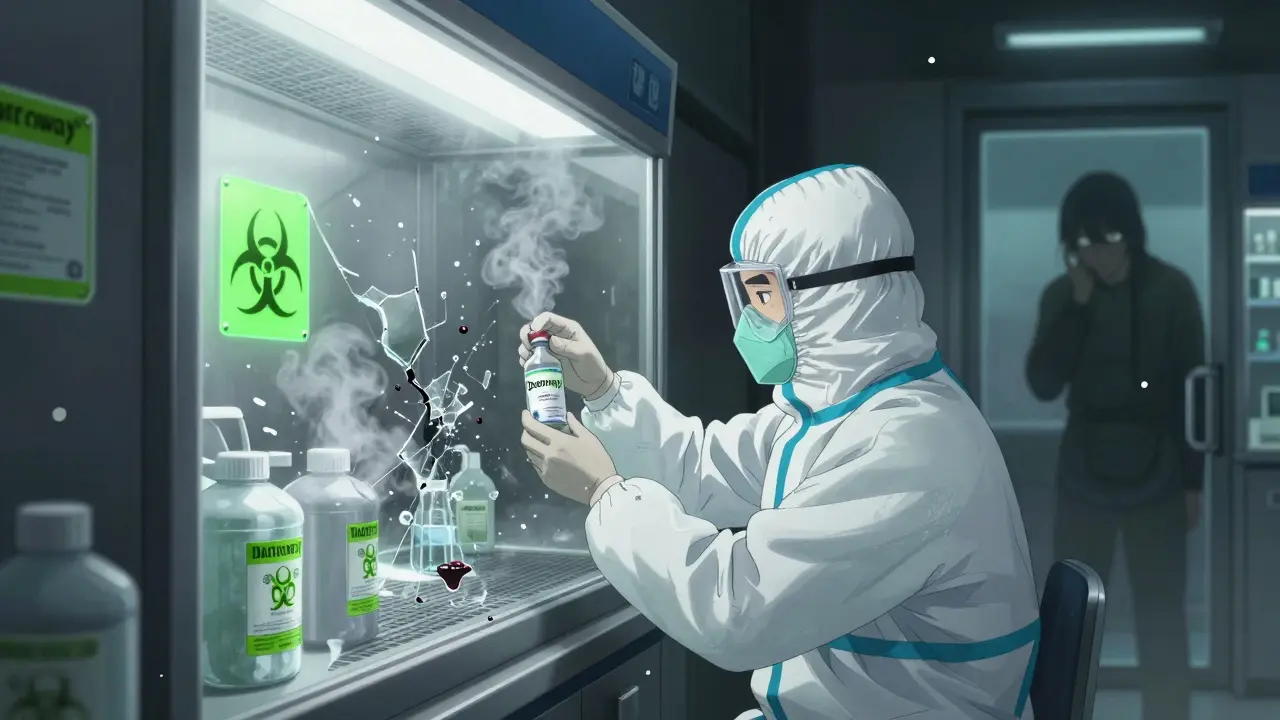
NIOSH didn’t just tweak its Hazardous Drugs List in 2025-it expanded it. Three new cancer drugs were added: datopotamab deruxtecan (Datroway®), treosulfan (Grafapex™), and telisotuzumab vedotin (Emrelis™). These are powerful antibody-drug conjugates, and they’re not just dangerous if swallowed-they’re hazardous if inhaled or absorbed through the skin.
Pharmacies and hospitals now need to upgrade their handling procedures. That means special ventilation cabinets, double-gloving, spill kits, and staff training. One pharmacy in Ohio reported two near-misses in July 2025 after a tech handled a new drug without updated training. After the NIOSH update, they shut down compounding for three days to retrain everyone. It cost time, but it prevented exposure.
Seven drugs were removed from the list, too. That’s not because they’re safer-it’s because new data showed they don’t pose the same level of risk as once thought. The list is now more accurate, not just longer.
CMS Star Ratings Are Now Tied to Real Safety Metrics
If you’re on Medicare Part D, your plan’s rating just got harder to improve. CMS updated 16 Patient Safety measures for 2025, and they’re no longer just about paperwork. They’re about real outcomes.
One key measure: Use of Opioids at High Dosage in Persons without Cancer (OHD). Plans are now penalized if they allow patients to stay on high-dose opioids without proper monitoring. That means pharmacists have to flag patients getting more than 90 morphine milligram equivalents per day-and reach out. No more automatic refills.
Another: Medication Adherence for Cholesterol (ADH-Statins). Plans must now prove patients are actually taking their statins. That’s not just sending reminders. It’s using data to identify who’s skipping doses and then calling them, offering home delivery, or even coordinating with their doctor to switch to a cheaper version.
Plans that score low on these measures lose Star Ratings. And lower ratings mean fewer enrollees-and less money. That’s why big insurers are investing in AI tools to predict who’s at risk of non-adherence before they stop taking their meds.
Global Standards Are Now in Place
The WHO didn’t just issue a guideline in September 2025-they created a global blueprint. For the first time, every country now has a framework to ensure people can get essential painkillers and cancer drugs without risking addiction or shortages.
The framework includes eight pillars: digital tracking for drug supply chains, legal protections so patients aren’t arrested for carrying prescribed opioids, training for doctors on pain management, and public education to reduce stigma. It’s ambitious. But in countries like Kenya and Vietnam, where patients used to go without morphine for cancer pain, this could be life-changing.
Still, the challenge is real. Only 12 countries have full national action plans. Most lack the infrastructure. The WHO’s goal? Cut preventable medication harm by 50% in five years. It’s possible-but only if rich countries help fund the systems in low-income regions.
How Are Pharmacies Actually Implementing This?
It’s not easy. A June 2025 survey by the National Community Pharmacists Association found 78% of independent pharmacies think the ISMP guidelines are valuable. But 62% say the cost of technology-like barcode scanners and electronic double-check systems-is too high.
One pharmacy in Texas implemented the weight-based dosing protocol and saw pediatric errors drop by 63% in six months. But it took 40 hours of staff training and a $12,000 software upgrade. They got a grant from a state health fund to cover half.
Big hospital systems are doing better. 89% now use barcode scanning for every medication given to a patient. But small pharmacies? Only 37% have it. That gap is growing. And it’s dangerous.
Some pharmacies are turning to modular, subscription-based tech. For $1,500 a month, they get cloud-based tools that flag dangerous interactions, remind staff to double-check, and auto-generate safety logs. It’s not perfect-but it’s better than nothing.

What’s Next in 2026?
The FDA is getting stricter. In 2025, they issued 23 safety alerts-up from 19 in 2024. One of the most urgent was about Tranexamic Acid, a bleeding control drug that was being confused with another similar-sounding medication. The fix? New packaging standards and clearer labeling rules starting in March 2026.
ISMP is already working on new hospital guidelines for early 2026. This time, they’re focusing on AI-driven alerts. Imagine a system that spots when a doctor orders a high-risk drug for a patient with kidney failure-and automatically suggests a safer alternative. Early tests show this cuts errors by 41%.
And CMS? They’re planning to add even more safety measures in 2026, possibly tying Star Ratings to actual patient harm data, not just process checks. That would be a game-changer.
What This Means for You
If you’re a patient: Ask your pharmacist if they use weight-based dosing for your meds. Ask if they do double checks on high-risk drugs. If they don’t, it’s not necessarily negligence-it might be that they can’t afford the tech. But you have a right to know.
If you’re a caregiver: Watch for changes in how medications are labeled. New packaging might look different. That’s intentional. It’s designed to prevent mix-ups.
If you’re a healthcare worker: The pressure is real. Staff shortages make it harder to follow all the new steps. But don’t skip the double-check. One error can end a life-and ruin a career.
The bottom line? Medication safety isn’t just about rules anymore. It’s about culture. It’s about systems. And it’s about people finally listening to the data-instead of ignoring it until someone gets hurt.
What are the most critical medication safety changes in 2025?
The biggest changes include ISMP’s requirement for weight-based dosing verification and independent double-checks for high-alert drugs, NIOSH’s addition of three new hazardous cancer drugs to its list, CMS tying Medicare Star Ratings to real patient safety outcomes like opioid misuse and statin adherence, and WHO’s first global framework to balance access to controlled medicines with abuse prevention.
Are these updates mandatory for pharmacies?
ISMP’s guidelines are voluntary but widely adopted as the industry standard. NIOSH’s hazardous drugs list is a recommended occupational safety standard, but OSHA can enforce compliance if exposure incidents occur. CMS measures are mandatory for Medicare Part D plans-failure to meet them affects funding and Star Ratings. WHO guidelines are advisory but increasingly used as benchmarks by national health agencies.
How do the new NIOSH hazardous drugs affect pharmacists?
Pharmacists handling drugs like Datroway® or Emrelis™ must now use engineering controls like containment ventilated cabinets, wear double gloves and protective gowns, and follow strict decontamination procedures. Training records must be kept. Failure to comply increases the risk of long-term health effects like infertility or cancer for pharmacy staff.
Why is CMS changing how it measures medication safety?
CMS realized that tracking processes-like how many refill reminders were sent-didn’t actually reduce harm. Now they’re measuring real outcomes: Are patients taking their statins? Are high-dose opioids being monitored? This shifts the focus from paperwork to patient safety, making plans financially accountable for real results.
What should I do if my pharmacy doesn’t follow the new guidelines?
Ask questions. If you’re on a weight-based medication like chemotherapy or insulin, ask if they verify your weight before dispensing. If you’re on a high-risk drug, ask if two staff members check the prescription. If they’re unfamiliar with the 2025 updates, it may mean they haven’t updated their protocols. You can also report concerns anonymously to ISMP or your state pharmacy board.
Will these changes make medications more expensive?
Not directly. But implementation costs-like new software, training, and safety equipment-may lead to higher operational expenses for pharmacies. Some of that could trickle down through higher copays or reduced services, especially in small, independent pharmacies. However, preventing one serious medication error saves an estimated $100,000 in hospital costs, so in the long run, these changes save money.
What to Watch for in 2026
Look for AI tools to become standard in medication safety. By next year, you’ll see more systems that auto-flag dangerous prescriptions before they’re even filled. Expect more FDA alerts on look-alike drug names. And keep an eye on whether low-income countries start receiving funding to adopt WHO’s access policies.
Medication safety isn’t a checklist. It’s a habit. And 2025 was the year the system finally started to change.






Cam Jane January 5, 2026
Just had my pharmacist verify my weight before giving me my chemo dose for the first time. Felt weird at first, but then realized-this should’ve been standard forever. No more guessing. No more ‘oh, she looks about 70kg.’ We’re talking life or death here. Finally, someone’s listening to the data.
My mom’s on insulin now too, and they’re doing double-checks. I didn’t even know that was a thing until this post. Thank you for highlighting this. It’s not glamorous, but it’s saving lives.
Dana Termini January 7, 2026
The NIOSH update on Datroway and Emrelis is long overdue. I’ve seen techs handling these drugs with nitrile gloves and no gown. One near-miss in our hospital last year involved a spill during transfer-no one knew the vapor risk. Now we have the cabinets, the training logs, the whole nine yards. It’s annoying, but it’s necessary.
Susan Arlene January 8, 2026
so like… we’re finally admitting meds are dangerous and not just ‘oops i took the wrong pill’
took me 3 years to get my statin refilled because the pharmacy kept losing my script. now they’re calling me? weird. but also… nice?
Mukesh Pareek January 9, 2026
It's evident that the current pharmacovigilance infrastructure is fundamentally misaligned with the risk profile of modern biologics and ADCs. The ISMP mandates are a necessary but insufficient intervention without concurrent implementation of ISO 13485-compliant traceability systems and real-time pharmacokinetic feedback loops. Absent these, you're merely automating compliance, not mitigating risk.
Matt Beck January 10, 2026
AI is gonna save us 😭🙏
Imagine your med app just pops up: 'Hey, your doc ordered 120mg morphine for someone with stage 3 kidney disease. Here’s a safer alternative. Also, your cousin died from this error in 2021. Just saying.'
That’s not sci-fi. That’s next year. And I’m here for it. The system’s finally waking up. 🌞💊
Kelly Beck January 11, 2026
Y’all, I work at a small pharmacy in rural Ohio, and we just got the grant to install the cloud-based safety system. It’s $1,500/month, but it auto-flags interactions, reminds us to double-check, and even prints out safety logs we can show patients. We cried. Not because it’s expensive-it’s not. But because we finally feel like we’re not just winging it.
To every pharmacist reading this: you’re doing important work. Even if your tech is old, even if you’re understaffed-you’re still the last line of defense. Keep going. We see you.
And yes, we verify weight now. Every. Single. Time.
Beth Templeton January 12, 2026
So let me get this straight-pharmacies are only now required to check a patient’s weight before giving chemo? Like… since when is that not basic? Did we need a national crisis to learn this?
Indra Triawan January 14, 2026
It’s all a distraction. The real issue is that Big Pharma pushed these new drugs knowing the side effects. Now they’re making us pay for the safety upgrades while they rake in billions. They don’t care about your life-they care about liability shields and patent extensions.
I’ve seen the emails. The warnings were there. They buried them.
Melanie Clark January 15, 2026
Did you know that the WHO framework was drafted by a committee that included representatives from 3 pharmaceutical companies? This is not safety. This is control. They’re using ‘patient harm reduction’ as an excuse to centralize drug distribution under corporate surveillance. Your prescription data is being fed into AI models to predict your behavior. Next they’ll ban you from getting pain meds if your credit score drops. I’m not paranoid. I’ve read the documents.