Did you know that the most common cause of an overactive thyroid is actually your own immune system? hyperthyroidism often hides behind a complex web of auto‑immune activity, and unraveling that web can change how you manage symptoms and treatment.
What Is Hyperthyroidism?
Hyperthyroidism is a condition where the thyroid gland produces excessive thyroid hormone, speeding up metabolism and affecting almost every organ. Typical signs include rapid heartbeat, weight loss despite normal eating, heat intolerance, and nervousness. The thyroid’s two main hormones, triiodothyronine (T3) and thyroxine (T4), flood the bloodstream, pushing the body into a constant “high‑gear” mode.
Autoimmune Diseases in a Nutshell
Autoimmune disease refers to a mis‑directed immune response where the body’s own defenses attack healthy tissue. Instead of protecting you from infections, immune cells release antibodies that mistakenly recognize organs as foreign. Over 80 different autoimmune conditions have been identified, ranging from rheumatoid arthritis to multiple sclerosis. The thyroid is a frequent target because it is highly vascular and packed with proteins that can look like an invader to a sensitised immune system.
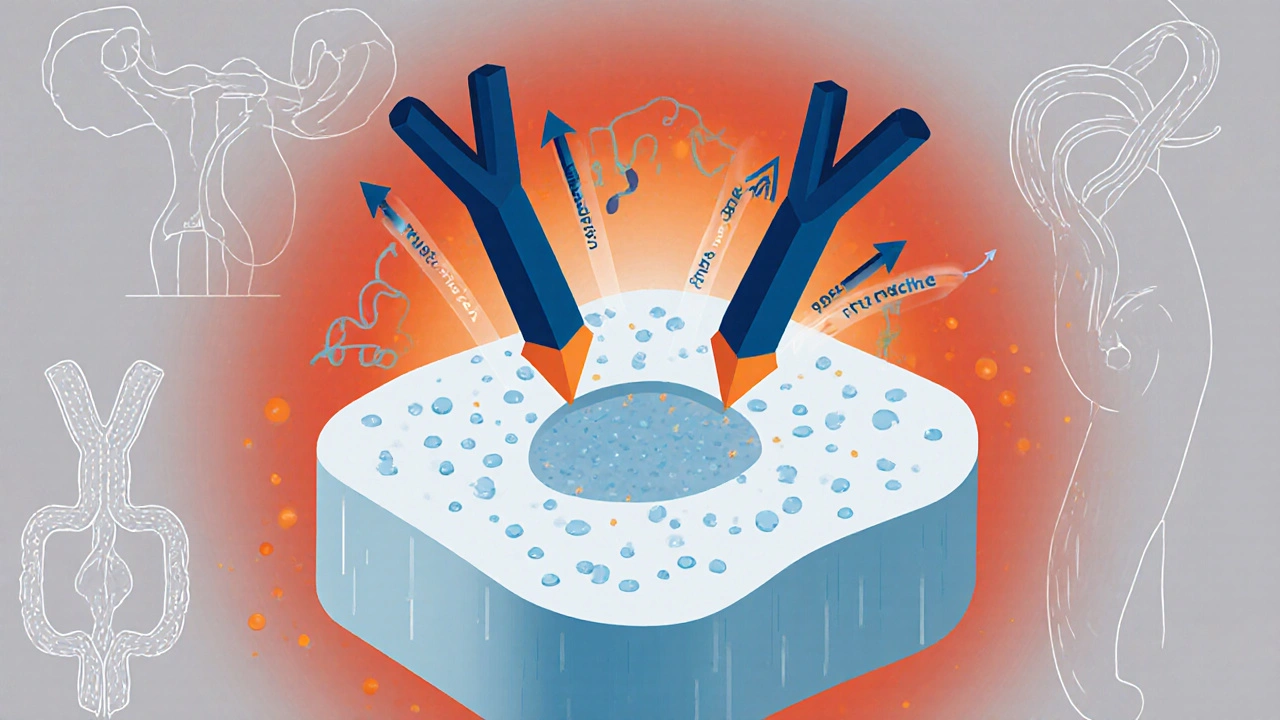
How Autoimmunity Triggers Hyperthyroidism
The link between hyperthyroidism and autoimmunity is strongest in Graves' disease, an autoimmune disorder where the immune system creates stimulating antibodies that bind to the thyroid‑stimulating hormone receptor (TSHR). These thyroid antibodies (specifically thyroid‑stimulating immunoglobulins, TSI) trick the gland into over‑producing T3 and T4, regardless of the body’s actual needs.
Because the antibodies are constantly active, the feedback loop that usually keeps thyroid hormone levels balanced breaks down. Even if the pituitary gland reduces its own hormone-thyroid‑stimulating hormone (TSH)-the thyroid keeps churning out excess hormone under antibody influence.
Other Autoimmune Thyroid Disorders That Can Cause Hyperthyroidism
While Graves' disease accounts for about 80% of autoimmune hyperthyroidism cases, other conditions can also lead to a temporary surge of thyroid hormone.
- Hashimoto's thyroiditis is typically associated with hypothyroidism, but early stages (thyrotoxic phase) can flip into hyperthyroidism as thyroid cells are destroyed and release stored hormone.
- Post‑partum thyroiditis follows childbirth. In the first few months, the inflamed gland may leak excess hormone before settling into a low‑function phase.
- Silent thyroiditis is an painless inflammation that can cause a brief hyperthyroid episode, driven by immune‑mediated gland damage.
All three share a common thread: the immune system’s attack on the thyroid unleashes hormone that the body was not asking for.
Key Hormones and Lab Markers to Watch
Diagnosing autoimmune‑driven hyperthyroidism involves a combination of hormone measurements and antibody tests.
- Thyroid‑stimulating hormone (TSH) - usually low because high thyroid hormone feeds back to suppress pituitary output.
- Free T4 and Free T3 - both elevated in active hyperthyroidism.
- Thyroid‑stimulating immunoglobulin (TSI) - positive in Graves' disease; values above the lab’s reference range support an autoimmune cause.
- Thyroid peroxidase antibodies (TPO‑Ab) - may be present in both Graves' and Hashimoto's, indicating general thyroid autoimmunity.
Imaging, such as a thyroid ultrasound or radioactive iodine uptake scan, can further differentiate Graves' disease (usually high uptake) from thyroiditis (low uptake).
Treatment Options Tailored to Autoimmune Hyperthyroidism
Because the root cause is antibody‑driven, treatment goals focus on lowering hormone production while managing the immune attack.
- Antithyroid medications (methimazole or propylthiouracil) block hormone synthesis. They are first‑line for most patients, especially those who are pregnant or planning pregnancy.
- Radioactive iodine therapy - Radioactive iodine is taken orally and selectively destroys overactive thyroid cells, reducing hormone output. It is a definitive option for many adults, but it may worsen eye disease in Graves' patients, so steroid prophylaxis is sometimes needed.
- Beta‑blockers (propranolol, atenolol) don’t touch hormone levels but calm rapid heartbeats, tremor, and anxiety while other treatments take effect.
- Surgery (partial or total thyroidectomy) is reserved for large goiters, suspicion of cancer, or when radioiodine is contraindicated.
- Immunomodulatory therapy - In severe Graves' ophthalmopathy, corticosteroids or newer agents like teprotumumab can blunt immune inflammation.
Long‑term follow‑up is essential because the immune system may stay active, and some patients develop hypothyroidism after definitive therapy, requiring lifelong levothyroxine replacement.

Lifestyle Strategies to Support Thyroid Health
While medication tackles the hormonal surge, everyday habits can ease symptoms and potentially calm the immune backlash.
- Balanced iodine intake - Both deficiency and excess can provoke thyroid dysfunction. Aim for the recommended 150µg/day, mainly from dairy, seafood, and iodised salt.
- Stress management - Chronic stress raises cortisol, which can aggravate autoimmunity. Mindfulness, yoga, or short daily walks can make a noticeable difference.
- Anti‑inflammatory diet - Foods rich in omega‑3 fatty acids (salmon, flaxseed) and antioxidants (berries, leafy greens) may dampen systemic inflammation.
- Regular sleep - 7‑8hours a night supports immune regulation and helps keep heart rate and metabolism stable.
- Avoid smoking - Smoking is a known risk factor for Graves' eye disease and can worsen overall thyroid outcomes.
These tweaks aren’t a cure, but they complement medical therapy and improve quality of life.
Comparison of Common Causes of Thyroid Hormone Imbalance
| Cause | Type of Imbalance | Autoimmune? | Typical Age Group | First‑Line Treatment |
|---|---|---|---|---|
| Graves' disease | Hyperthyroidism | Yes | 20‑40years | Antithyroid drugs / Radioactive iodine |
| Hashimoto's thyroiditis | Hypothyroidism (often after a brief hyper phase) | Yes | 30‑60years | Levothyroxine |
| Iodine deficiency | Hypothyroidism | No | Regions with low dietary iodine | Iodine supplementation |
| Thyroid nodules / Cancer | Can cause either, depending on hormone‑secreting activity | Rarely autoimmune | Adults >50years | Surgery or targeted therapy |
| Post‑partum thyroiditis | Transient hyperthyroidism → hypothyroidism | Yes | Within 12months after delivery | Beta‑blockers (hyper) / Levothyroxine (hypo as needed) |
Frequently Asked Questions
Can hyperthyroidism become permanent?
If left untreated, an over‑active thyroid can lead to permanent heart problems, bone loss, and in rare cases, thyrotoxic crisis. Most people achieve long‑term control with medication, radioactive iodine, or surgery, but regular monitoring is crucial.
Is Graves' disease the only autoimmune cause of hyperthyroidism?
Graves' disease accounts for the majority, but conditions like post‑partum thyroiditis or silent thyroiditis can also produce an autoimmune‑driven surge of hormone.
Can diet cure hyperthyroidism?
No single diet cures the disease, but a balanced intake of iodine, reduced caffeine, and anti‑inflammatory foods can lessen symptoms and support treatment effectiveness.
Will I need lifelong medication after radioactive iodine?
Most patients become hypothyroid after radioactive iodine and will need levothyroxine for the rest of their lives. This is easier to manage than fluctuating hyperthyroid levels.
Are there any warning signs of a thyroid storm?
Sudden high fever, rapid heart rate (>130bpm), severe agitation, vomiting, or diarrhea may signal a thyroid storm-a medical emergency that requires immediate hospital care.
Understanding that hyperthyroidism often stems from an over‑active immune system empowers you to ask the right questions, choose targeted treatments, and adopt lifestyle tweaks that keep the hormone roller‑coaster in check.




Hayden Kuhtze October 12, 2025
Oh, because we all needed another masterclass on thyroid autoimmunity, right? Your post simply re‑hashes the textbook definition with the enthusiasm of a bored lecture.
Craig Hoffman October 15, 2025
Here’s the quick takeaway: Graves’ disease drives most autoimmune hyperthyroidism, TSI antibodies boost hormone output, and treatment hinges on antithyroid meds or radioiodine.
Terry Duke October 18, 2025
Wow, the immune system can really throw a wild party in the thyroid, releasing hormones left and right, and it’s amazing how lifestyle tweaks like stress reduction and omega‑3s can actually help calm that storm, giving patients a better quality of life, and that’s genuinely encouraging!
Chester Bennett October 21, 2025
Hyperthyroidism often masquerades as anxiety.
The underlying immunologic mechanisms are key.
Graves’ disease accounts for the lion's share of cases.
The pathogenic TSI antibodies bind to the TSH receptor and mimic its action.
This results in unchecked synthesis of T3 and T4.
Laboratory evaluation typically shows suppressed TSH alongside elevated free T3/T4.
Positive TSI or TPO‑Ab further confirms an autoimmune etiology.
Imaging modalities, such as radioactive iodine uptake, differentiate Graves’ from thyroiditis.
Management should be individualized, balancing symptom control with disease modification.
Antithyroid drugs like methimazole are first‑line for most patients.
Radioactive iodine offers a definitive solution but may exacerbate ophthalmopathy without steroid prophylaxis.
Surgical thyroidectomy remains an option for large goiters or refractory cases.
Regardless of the chosen therapy, regular monitoring of thyroid function tests is essential to avoid overtreatment.
Many patients transition to hypothyroidism after definitive therapy, necessitating levothyroxine replacement.
Lifestyle interventions-including adequate iodine, stress management, and anti‑inflammatory diet-support medical treatment and improve outcomes.
In summary, recognizing the autoimmune root of hyperthyroidism guides both diagnostic work‑up and therapeutic strategy, ultimately leading to better patient care.
Emma French October 24, 2025
The immune system’s misdirection is a serious issue, and patients deserve clear guidance on how to navigate treatments without being swept into hype.
Debra Cine October 27, 2025
Absolutely, you’re spot on! 😊 It’s all about cutting through the noise and giving folks solid, empathetic advice they can actually use.
Rajinder Singh October 30, 2025
Behold! The thyroid, that fickle maestro of metabolism, is once again commandeered by a rogue legion of antibodies, thrusting the body into a relentless frenzy of heat and haste.
Samantha Leong November 2, 2025
I hear the frustration behind those dramatic words; many feel powerless when their bodies accelerate beyond their control, and compassionate support can make a real difference.
Taylor Van Wie November 5, 2025
Our healthcare system should prioritize American research on thyroid autoimmunity-no foreign protocols can match our standards.
carlee Lee November 8, 2025
Great info, thanks.
chuck thomas November 11, 2025
The interplay between endocrine signaling and immune regulation reminds us that the body is a symphony, each instrument needing harmony; when one section rebels, the entire performance suffers, urging us to seek balance through both medicine and mindful living.
Gareth Pugh November 14, 2025
Indeed, a harmonious chord between thyroid health and immune calm can turn chaos into melody.
Michael Daun November 17, 2025
yall should remember to keep regular checkups, cuz early detection saves a lotta trouble.