Diabetes Medication Side Effect Risk Estimator
Assess your personalized risk for common diabetes medication side effects based on your health profile and current medications.
Your Personalized Risk Assessment
Consult your doctor about these risks and possible alternatives.
Why Diabetes Medications Often Make Glucose Management Harder
Diabetes isn’t just about high blood sugar. It’s about managing a delicate balance-and the very drugs meant to help can throw that balance off. For millions of people with Type 2 diabetes, taking medication doesn’t mean relief. It often means new problems: nausea so bad you skip meals, dizzy spells from low blood sugar, or yeast infections that keep coming back. And when side effects hit, many people stop taking their pills. Studies show nearly half of patients quit their diabetes meds within the first year-not because the treatment isn’t working, but because it’s too hard to live with.
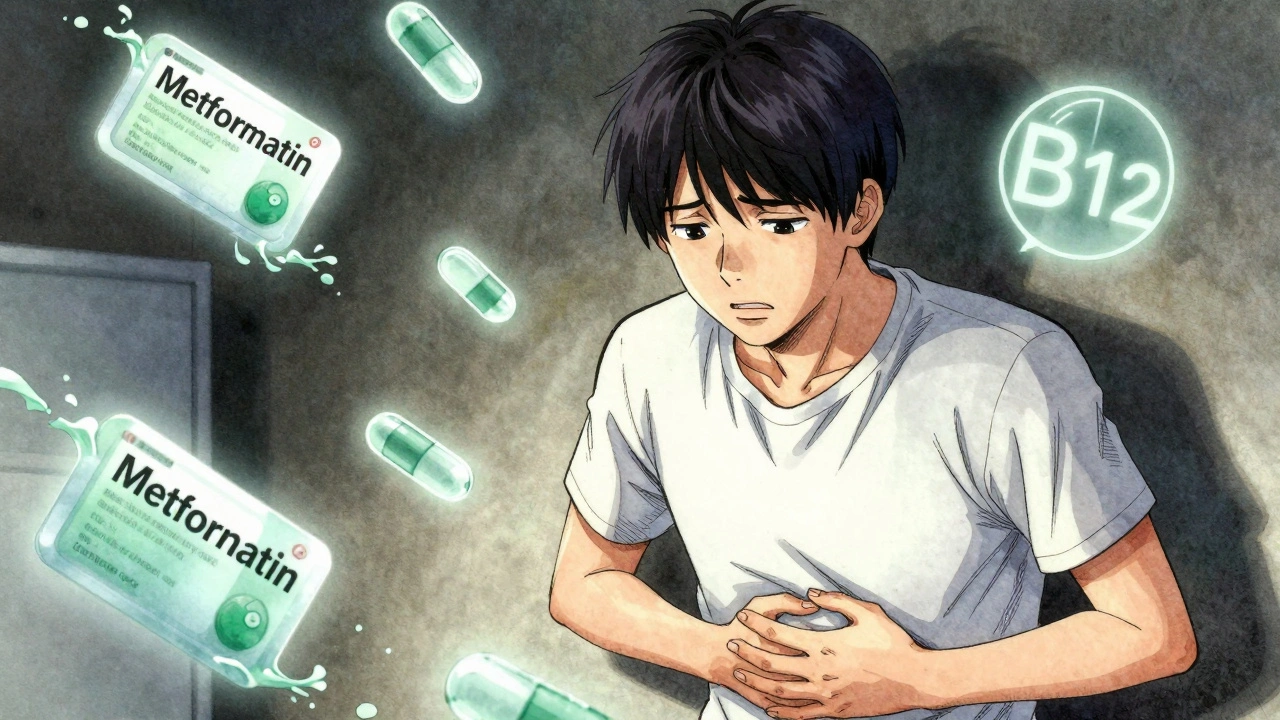
Metformin: The First-Line Drug With Hidden Costs
Metformin is still the go-to starting point for most Type 2 diabetes patients. It’s cheap, effective, and doesn’t cause low blood sugar. But up to 30% of people who take it deal with stomach issues: bloating, cramps, diarrhea, or just feeling sick after eating. These side effects aren’t mild. On review sites like Drugs.com, 42% of users say their gastrointestinal problems were moderate to severe. That’s not just discomfort-it’s life disruption. People skip meals, avoid social dinners, or even stop taking the drug altogether.
There’s a workaround: extended-release versions (like Glucophage XR or Fortamet) reduce stomach upset by 25%. Starting low-500 mg once a day with food-and slowly increasing helps too. But there’s another hidden risk: long-term use (over 4 years) can lead to vitamin B12 deficiency. That means fatigue, tingling in hands and feet, and even memory problems. The fix? A daily 1,500 mcg B12 supplement. Most doctors don’t mention this unless you ask.
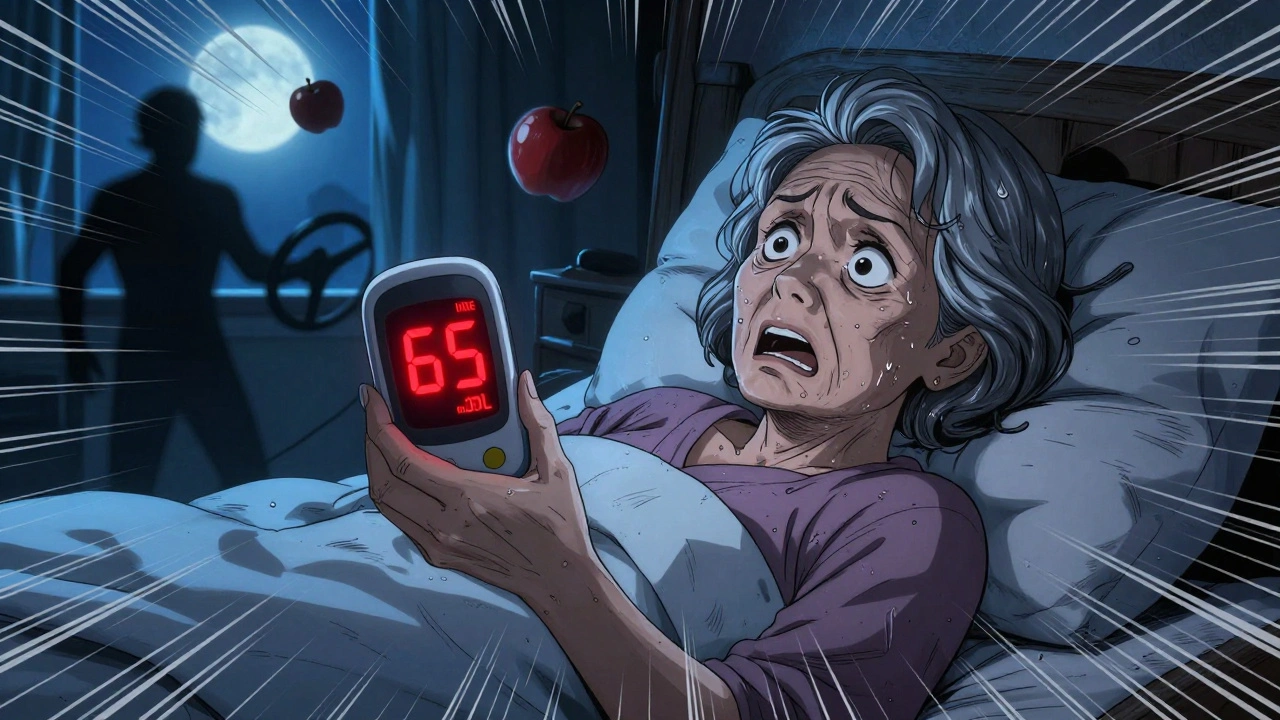
Sulfonylureas: The Hypoglycemia Trap
Drugs like glipizide and glyburide push your pancreas to make more insulin. That lowers blood sugar-but too much can send it crashing. About 15-20% of users get hypoglycemia, defined as blood sugar below 70 mg/dL. Symptoms? Shakiness, sweating, confusion, rapid heartbeat. In older adults, this can lead to falls, confusion, or even hospitalization. One woman in Bristol told her endocrinologist she passed out while driving because her sugar dropped overnight. She didn’t know the risk until it happened.
The 15-15 rule helps: eat 15 grams of fast-acting sugar (like juice or glucose tabs), wait 15 minutes, check your level. Repeat if needed. But prevention is better. Continuous glucose monitors (CGMs) cut severe low-blood-sugar events by 40%. If you’re on sulfonylureas, a CGM isn’t optional-it’s lifesaving.
SGLT2 Inhibitors: Weight Loss With a Price
Drugs like Jardiance, Farxiga, and Invokana work differently. They make your kidneys flush out extra sugar through urine. That lowers blood sugar, helps with weight loss (2-3 kg in six months), and protects the heart and kidneys. But the trade-off is serious. Up to 10% of users get urinary tract infections. Women face a 4-6% risk of yeast infections. Men get them too, though less often-around 1-2%. One Reddit user, u/DiabeticDad, wrote: “Jardiance dropped my A1c from 8.2 to 6.8. But I got three UTIs in six months. I switched.”
There’s also a rare but deadly risk: Fournier’s gangrene, a fast-spreading genital infection. The FDA has warned about 55 cases between 2013 and 2018. Another rare danger is diabetic ketoacidosis-even when blood sugar isn’t high. And canagliflozin increases the risk of toe or foot amputations by 0.3-0.5%. These drugs aren’t for everyone. If you have poor kidney function (eGFR under 30), avoid them. If you’re over 75, be extra cautious.
TZDs: The Heart Failure Risk
Actos and Avandia make your body more sensitive to insulin. They help lower blood sugar-but they also cause fluid retention. That means swelling in the legs, sudden weight gain, and worse, heart failure. Rosiglitazone (Avandia) was pulled in Europe in 2021 after studies showed a 43% higher risk of heart failure hospitalizations. Even pioglitazone (Actos), which is safer, isn’t recommended for people with advanced heart disease. If you’re on one of these and notice rapid weight gain or shortness of breath, call your doctor. Don’t wait.
How to Choose the Right Drug for You
There’s no one-size-fits-all. Your best drug depends on your body, your risks, and your life. If you’re overweight and have heart disease, an SGLT2 inhibitor might be ideal. If you’re older with kidney issues, metformin is safer. If you’re prone to low blood sugar, avoid sulfonylureas. If you have a history of yeast infections, SGLT2 inhibitors could backfire.
Doctors are starting to use genetic testing to predict who’s likely to get bad side effects. People with the ADL-1 variant have over three times the risk of metformin nausea. Those with the CYP2C9*3 variant are nearly three times more likely to get dangerous lows on sulfonylureas. This isn’t routine yet-but it’s coming.
What Patients Wish Their Doctors Told Them
A Mayo Clinic survey found 68% of patients felt unprepared for side effects. They knew about high blood sugar. They didn’t know about the yeast infections, the B12 loss, or the sudden dizziness. Most didn’t know to ask about CGMs or B12 supplements. The biggest complaint? “No one warned me.”
Here’s what you should ask your doctor:
- “What side effects should I expect with this drug?”
- “Is there a lower-dose or extended-release version?”
- “Do I need a B12 test or supplement?”
- “Should I get a continuous glucose monitor?”
- “What do I do if I feel dizzy or have frequent infections?”
What’s Changing in 2025
New combinations like Xigduo XR (metformin + dapagliflozin) cut metformin’s stomach issues by 25%. New drugs like INT131, a next-gen TZD, show 60% less swelling in early trials. And glucose-responsive insulin-still in testing-could one day replace daily pills by releasing insulin only when blood sugar rises.
But for now, the reality is this: diabetes meds are powerful tools, but they come with trade-offs. The goal isn’t just to lower A1c. It’s to help you live well. If your medication is making your life harder, talk to your doctor. There’s always another option.
When to Switch Medications
Don’t wait until you’re miserable. If side effects last more than 2-3 weeks, or if they’re affecting your sleep, eating, or daily routine, it’s time to reconsider. Most side effects improve with time-but not all. If you’re having frequent infections, severe nausea, or unexplained fatigue, don’t tough it out. Your doctor can switch you to a different class or adjust your dose. It might take 3-6 months to find the right fit, but it’s worth it. Adherence rates jump 40% when side effects are proactively managed.
Bottom Line: Your Health, Your Choice
Diabetes medication isn’t a one-time decision. It’s an ongoing conversation. What works today might not work next year. Side effects aren’t failures-they’re signals. Listen to your body. Track your symptoms. Ask questions. And remember: you’re not alone. Millions are navigating the same challenges. The best treatment isn’t the one with the lowest A1c. It’s the one you can stick with-and live well with.



Ethan McIvor December 4, 2025
This hit me right in the soul. I’ve been on metformin for 5 years and just found out last month my brain fog and tingling hands were from B12 deficiency. My doctor never mentioned it. I started taking 1500 mcg daily and it’s like I got my life back. 🙏
Mindy Bilotta December 5, 2025
i was on jardiance for 6 months and got 3 yeast infections. no one warned me. i felt so gross and embarrassed. switched to glimepiride and no more issues. also, the weight loss was nice but not worth it.
Erik van Hees December 6, 2025
Let me tell you something, folks. The real problem isn’t the meds-it’s the lazy doctors who treat diabetes like a checkbox. You want to know why people quit? Because no one tells you about the 15-15 rule until you’re shaking in a parking lot at 3 a.m. CGMs aren’t luxury items-they’re survival gear. And if your doc doesn’t push one for you on sulfonylureas, find a new doc. Period.
Storz Vonderheide December 7, 2025
I’m a nurse in Chicago and I see this every day. Patients are scared to speak up because they think they’re being ‘difficult.’ But here’s the truth: side effects aren’t weakness-they’re data. I always tell my patients: ‘If your meds are making you miss work, skip family dinners, or avoid the shower because you’re embarrassed-you’re not failing. Your treatment is.’ And we adjust. Always. You deserve to live, not just survive.
dan koz December 8, 2025
In Nigeria we don’t even have access to most of these drugs. Most people are on metformin or glibenclamide and just pray. No CGMs. No B12 tests. No extended release. We just try not to die. The fact that people in the West complain about side effects while we’re begging for any pill at all... it’s wild.
Kevin Estrada December 9, 2025
Okay but let’s be real-this whole system is a scam. Big Pharma knows metformin causes B12 loss and SGLT2 inhibitors cause gangrene but they still push them because they make billions. And your doctor? They get paid per script. They don’t care if you’re crying in the bathroom from yeast infections. They just want your A1c to look pretty on their dashboard. Wake up.
Katey Korzenietz December 11, 2025
I got Fournier's gangrene scare last year. 3 days in the ER. 2 surgeries. All because I didn't know to check for genital pain with SGLT2. My doc said 'it's rare.' Rare doesn't mean 'won't happen to you.' I'm now on metformin XR and I'm alive. Don't be a statistic.
Michael Bene December 12, 2025
Honestly? The only reason I didn’t quit meds is because I read about the ketoacidosis risk with SGLT2s and thought, ‘nah, I’d rather have a UTI than die screaming in a hospital.’ Also, I started taking my metformin with a big ol’ bowl of oatmeal and it cut the diarrhea in half. No one told me food timing mattered. I feel like a genius.
Brian Perry December 12, 2025
so i switched from glyburide to liraglutide and now i’m throwing up every morning. my wife says i smell like a diabetic dumpster fire. i’m considering just eating tacos and hoping for the best.
Chris Jahmil Ignacio December 13, 2025
The government and pharma are pushing these drugs because they want you dependent. Why? Because if you’re on insulin or SGLT2 inhibitors, you’re a lifelong customer. They don’t want you cured. They want you dosed. They don’t care about your yeast infections, your B12 deficiency, your falls, your amputations. They care about quarterly profits. And your doctor? They’re paid by the system. You’re a number. You’re not a person.
Paul Corcoran December 14, 2025
I want to say thank you to everyone sharing their stories. This isn’t just medical info-it’s human stuff. I’ve been on metformin for 7 years, had the B12 crash, the nausea, the shame of skipping birthday dinners. I finally found a combo of XR metformin + B12 + a CGM and I’m living again. It took 5 years. You’re not alone. And it’s okay to ask for help. Keep talking.
Susan Haboustak December 14, 2025
You all sound like you’re begging for permission to be sick. If you can’t handle side effects, maybe you shouldn’t be on medication. Just eat less sugar. Walk more. Stop being so entitled to convenience. This isn’t a spa. It’s life.