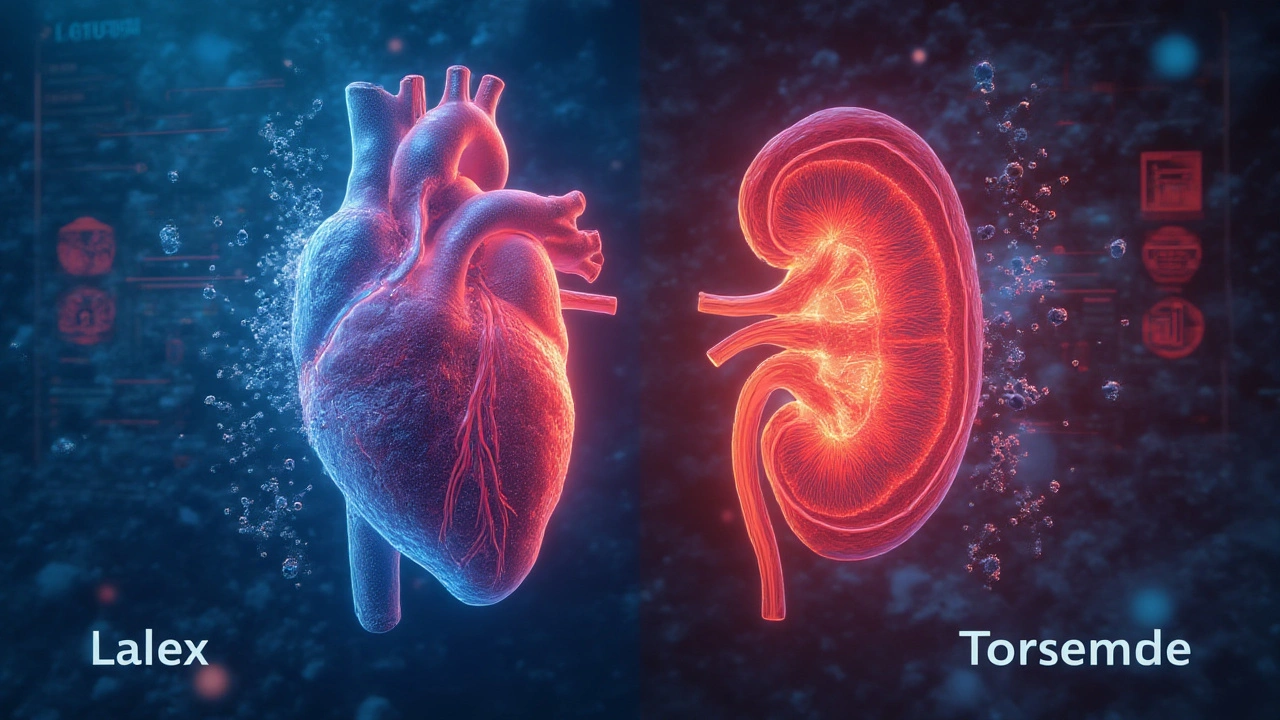
Picture this: one day, your ankles look like overfilled water balloons, or you’re gasping after climbing a single flight of stairs. Congestive heart failure (CHF) or fluid-bloated legs from chronic edema demand answers, and for years, two old rivals—Lasix (furosemide) and Torsemide—have been the first line of defense. People hear doctors toss these names around, but if you’re the patient popping the pills, it helps to know exactly what’s different inside that tablet. Here’s what really separates Lasix and Torsemide when your kidneys and heart need a helping hand.
Duration of Action: Why Timing Matters for Your Pills
Let’s start with how long these meds stick around in your system. Duration of action isn’t just a fancy phrase—it means how steady those pee-demanding effects last in your body. A lot of people get stuck planning their day around sudden bathroom trips because of furosemide (Lasix). This drug kicks in fast—think 30 to 60 minutes after swallowing—but it wears off after about 6 hours. For many, that means two or sometimes three sweaty bathroom dashes per day to flush fluids out. Some even set alarms to take it twice daily so their ankles don’t balloon by evening.
Now, Torsemide is a little sneakier. Same goal, but once it gets working, it sticks around almost twice as long—close to 12 hours, sometimes even to 16. That means one morning dose and you’re usually covered until bedtime, with no awkward mid-day panic for the nearest restroom. That’s a huge deal if you have a job, drive, or just hate scheduling life around a diuretic’s whims. Jules, a retired teacher who switched to Torsemide, told me she could finally run errands again without frantically hunting for a public toilet—talk about freedom most healthy folks take for granted.
Timing isn’t just about comfort. Short-acting diuretics like Lasix can sometimes trigger a "rebound"—once the drug fades, excess sodium sneaks back, and the fluid returns. Torsemide’s longer half-life can mean a smoother ride, fewer "off" hours, and steadier blood pressure. For patients managing chronic conditions, consistency matters. If your ankles swell up by lunchtime or you wake up gasping at night, that once-daily reliability starts sounding pretty tempting. But, as with all things body-related, response varies: some folks swear by the quick punch of Lasix, others find its on-off drops harder to handle.
Bioavailability: How Much of Your Pill Actually Works?
Imagine swallowing a med that loses half its power before your kidneys even see it. That’s the reality of bioavailability. Lasix is famous for its unpredictability—you might get 10% of the dose absorbed, some days 100%, and most days, something in between. Food, stomach acid, even other meds fighting for the same absorption highway can mess with its effectiveness. This is one reason why some patients on Lasix complain of wild swings: one morning, their rings are loose and ankles slim, the next, they’re puffy and frustrated.
Torsemide takes a smarter route. Its bioavailability sticks reliably around 80% or more, no matter if you’ve eaten or not. Take Torsemide with breakfast, lunch, or alone—your body doesn’t care, it gets the same hit. That means more precise blood pressure control and more predictable impact on swelling. If you’re the detail-oriented type keeping a log of daily weights (as docs often recommend for CHF folks), you’ll probably spot steadier progress with Torsemide. One real-world study found that patients were less likely to bounce back with sudden weight gains, hinting at the benefit of a drug that consistently does its job every time.
Have you ever had to up your dose of Lasix, only to feel like nothing changed? That’s often the curse of poor absorption, not medical failure. Some doctors will move patients to Torsemide when Lasix seems to "stop working," and suddenly, things turn around. It’s not that Torsemide is magical, it’s just less finicky.

Which Works Better? Outcome Data in CHF and Edema
The million-dollar question—does one actually work better at improving quality of life or helping people live longer? It’s not just an academic debate; it means everything when you’re trying to keep the swelling (and ER visits) at bay. Let’s look at the facts.
A large recent trial in people with CHF revealed Torsemide may not only keep fluid off better but could reduce hospitalizations compared to Lasix. There’s even some evidence (though not a done deal yet) that Torsemide might nudge survival numbers higher. Why? Researchers suspect it comes back to those smoother blood levels and less roller-coastering, making it easier to hit the "sweet spot" where fluid stays off without dropping your blood pressure too low or making your kidneys cranky.
But Lasix isn’t slouching to retire just yet. It’s more widely available, and for pure rapid relief—like a bad day of sudden swelling or in the ER—Lasix can be a hero, especially given its punchy onset. Plus, for some, insurance covers it better, and decades of doctors know how to handle its quirks. If you’re looking at managing *edema* in milder, non-cardiac conditions, Lasix might be all you need, sparing the fancier pick.
Now, side effects—sadly, there’s no free pass. Both can lower potassium, magnesium, and sodium, sometimes dangerously. They can tangle with hearing and kidneys if the dose gets high or the body is frail. But real talk? Because Torsemide lasts longer and is more reliably absorbed, sometimes patients need a smaller dose, possibly lowering risk for "diuretic resistance" and the cycle of ever-increasing pill counts. In recent years, more docs are leaning into Torsemide for tough-to-treat CHF, while still reaching for Lasix for everything from puffy legs to acute lung fluid spikes. If you crave more insight into options beyond these classic loop diuretics, check out this breakdown of alternative to Lasix choices making waves right now.
Tips for Patients: Getting the Most Out of Your Diuretic
Living with CHF or chronic edema is hard enough—no one needs drug trivia adding to the load. Here’s what matters: if your swelling is stubborn, your Lasix seems to have lost its edge, or bathroom sprints rule your life, talk to your provider about switching up the game. Some people see dramatic benefits with Torsemide, but it’s not a universal fix. Bring a daily weight log to appointments—these numbers give your team real clues about which diuretic is working, or if both fall short.
Stick to a regular dosing schedule: Torsemide shines because it frees you from the twice-daily grind, but don’t wing it—try to take it at the same time every morning. Watch for warning flags like muscle cramps, dizziness, dry mouth, or rapid heartbeats. These hint at low potassium or dehydration, and it’s serious—your doctor might add supplements or tweak doses.
Diet makes a difference. High-salt meals can undermine any diuretic—Lasix, Torsemide, or any cousin. If you notice some days nothing seems to work, peek at your diet from the past 24 hours. Processed food, takeaway, and "healthy" canned soup are landmines for hidden sodium. Drink enough fluid to avoid wild dehydration swings, but not so much you undo the med’s work. Most CHF folks do best keeping to a magic fluid and salt target, something your provider sets just for you.
If you’re curious about your body’s response, it’s totally normal. Actually, tracking what happens after each kind of pill, jotting down how bathroom needs and swelling change, can help your doctor fine-tune your approach. For the tech-minded, there are now smart scales and CHF tracking apps—use whatever makes this wild ride a little less lonely and a bit more under your control.
And one last thing—sometimes, it’s not about picking "the best" on paper, it’s about what fits your life. If Lasix with breakfast means you spend breakfast next to the bathroom, or Torsemide lets you stretch errands between appointments, that daily reality matters more than stats and charts.
People often overlook the little victories—fewer ER visits, more comfy shoes, or just a restful night free from gasping or ballooning feet. Your diuretic choice plays a huge role in making that your story. So don’t be afraid to start the conversation, ask about options, and compare experiences. Knowledge isn’t just power—it might be your ticket to lighter steps and easier breathing tomorrow.





Gayle Jenkins July 16, 2025
I switched to torsemide last year after my ankles turned into water balloons every afternoon. One pill in the morning and I can actually go grocery shopping without planning my route around public bathrooms. No more midday panic. Life changed. Seriously.
My cardiologist was skeptical but I begged for the switch. Now I sleep through the night. No more waking up gasping. If you’re on lasix and it’s wrecking your rhythm-just ask. It’s not magic, it’s just better engineered.
Kaleigh Scroger July 16, 2025
Let me tell you about bioavailability because nobody talks about this enough. Lasix is a gamble. One day you take 40mg and you’re dry as a bone the next you take the same dose and you’re still puffy as a marshmallow. Why? Because your stomach acid decides whether it works or not. Torsemide? It doesn’t care if you ate a burrito or fasted for 12 hours. It’s 80% absorbed every single time. That’s not a minor difference that’s a game changer for people who need predictability. I’ve seen patients on lasix get bumped up to 160mg then 240mg and still swell and it’s not because they’re resistant it’s because half the pill just disappears. Torsemide doesn’t play games. It shows up. And your kidneys thank you.
Also side effect wise? Less need for crazy high doses means less risk of electrolyte chaos. Fewer cramps fewer dizziness fewer ER trips. It’s not even close when you look at the data.
And yes I’m a nurse. I’ve seen both. Trust me.
Oh and don’t get me started on the rebound effect. Lasix fades at 6 hours and your body says oh thanks for the head start now let’s hoard all the sodium we can. Torsemide? Smooth. Even. Consistent. That’s what chronic care needs not a rollercoaster.
Elizabeth Choi July 18, 2025
It’s all just marketing. Torsemide costs 3x more. If you’re not rich you’re stuck with lasix. Don’t pretend this is about science. It’s about profit margins. Your doctor doesn’t care if you pee 12 hours straight they care if insurance pays.
Also ‘rebound’? That’s just what happens when you’re not controlling your sodium. Blame the pill all you want but your chips and soup are the real problem.
Allison Turner July 18, 2025
Why is everyone acting like torsemide is some miracle drug? It’s just another diuretic. Lasix works fine for most people. You just need to take it right. Stop making it complicated. Also I bet most of you are just lazy and don’t want to plan your day around peeing.
Also the article says ‘Jules’ could run errands? Who is Jules? Did she pay for this ad?
Darrel Smith July 19, 2025
THEY’RE ALL JUST BIG PHARMA’S TOYS. WHY DO YOU THINK TORSEMIDE WAS CREATED? BECAUSE LASIX WAS TOO CHEAP AND THEY NEEDED A NEW PRODUCT TO SELL. THEY’RE NOT BETTER THEY’RE JUST MORE EXPENSIVE. AND DON’T EVEN GET ME STARTED ON THE ‘STUDIES’-EVERYTHING’S MANIPULATED. I KNOW WHAT’S GOING ON. I’VE SEEN THE DOCUMENTS.
YOU THINK YOUR KIDNEYS ARE ‘LESS CRANKY’? THEY’RE BEING MANIPULATED. YOU’RE BEING MANIPULATED. EVERYTHING IS A SCAM. I TOOK LASIX FOR 10 YEARS AND I’M STILL ALIVE. TORSEMIDE? THAT’S A TRAP. THEY WANT YOU DEPENDENT ON EXPENSIVE DRUGS. YOU’RE BEING USED.
AND WHY DO YOU THINK THEY PUT THAT LINK TO CANADADRUGSTOP? THAT’S A FAKE SITE. THEY’RE SELLING YOU PILLS FROM A BACK ALLEY. I SAW A VIDEO. THEY’RE USING FAKED LAB RESULTS. DON’T TRUST ANYTHING.
Aishwarya Sivaraj July 21, 2025
i read this and thought about my mom who had chf and used lasix for years. she used to say the pills felt like they were playing hide and seek with her body. some days she felt light some days like a balloon. when she switched to torsemide it was like someone finally turned on the lights. no more guessing. no more panic. she could sleep. she could walk to the market. i cried when she told me.
but also... maybe the real difference is not just the drug but how we listen to our bodies. maybe we need to stop thinking of meds as fixes and start thinking of them as partners. you dont fight your body you work with it. torsemide just lets you do that better.
also typos are everywhere im sorry im typing on my phone in the hospital waiting room
Iives Perl July 23, 2025
torsemide is a CIA mind control drug. they made it so you can’t tell when you’re being watched. 12 hour window = 12 hours of surveillance. lasix is freedom. i took it for 7 years and never once felt monitored. 💥
steve stofelano, jr. July 24, 2025
While I appreciate the thorough exposition of the pharmacokinetic distinctions between furosemide and torsemide, I must respectfully underscore the importance of individualized therapeutic regimens. The clinical context, renal function, comorbidities, and socioeconomic factors must all be weighed with the utmost diligence. While torsemide demonstrates superior bioavailability and duration of action in controlled trials, its accessibility remains constrained in certain healthcare systems. A one-size-fits-all recommendation would be both medically and ethically untenable. I commend the author for emphasizing patient autonomy and daily lived experience as critical components of therapeutic success.
Savakrit Singh July 25, 2025
USA always thinks their drugs are better. In India we use lasix since 1980s. Cheap. Effective. Torsemide? 10x price. Who can afford? Also, your ‘studies’? Mostly funded by American pharma. 😒
My uncle had CHF. Lasix worked. He lived 12 years. Torsemide? Just marketing. 💸
Cecily Bogsprocket July 26, 2025
There’s something so quiet and powerful about finding a medication that lets you just... live. Not manage. Not survive. Live.
I remember my sister saying she could finally sit on the porch without her socks leaving imprints on her ankles. That’s not a lab result. That’s dignity.
I don’t care if it’s lasix or torsemide. I care that someone finally listened when she said ‘I can’t do this anymore.’
Medicine isn’t just about molecules. It’s about letting people breathe again.
Thank you for writing this. It felt like someone finally saw us.
Jebari Lewis July 28, 2025
As someone who tracks daily weights and fluid intake religiously, I can confirm: torsemide delivers consistency. My weight fluctuations dropped from ±2.5 lbs/day to ±0.5 lbs/day after switching. That’s not placebo. That’s pharmacology.
Also, I’ve had patients on lasix who were ‘non-responsive’-turned out they were taking it with coffee or grapefruit juice. Bioavailability is everything. Torsemide doesn’t care what you drink. It just works.
And yes, I’m a clinical pharmacist. I’ve reviewed over 300 CHF charts. The data is clear. The question isn’t whether torsemide is better-it’s why more doctors aren’t switching patients proactively.
Emma louise July 30, 2025
Oh wow a whole article about diuretics? How revolutionary. Next you’ll tell us water is wet. Meanwhile, the real problem is Americans are obese and eat 5000mg of sodium a day. Blame the pill? No. Blame the processed food industry. And the doctors who let you eat pizza with your meds.
Also, why is this even a thing? We have better drugs. Why are we still debating 1950s meds? Sad.
sharicka holloway July 31, 2025
Just wanted to say: if you’re on one of these and it’s not working, talk to your doc. No shame. No rush. Just ask. You deserve to feel normal. You deserve to walk without your legs screaming. You’re not broken. Your meds might just need a tune-up.
And if you’re scared to ask? Bring this post with you. It’s a good start.
Alex Hess August 1, 2025
This is so basic. Anyone who doesn’t know the difference between furosemide and torsemide shouldn’t be reading medical blogs. You’re a patient, not a pharmacist. Just take what your doctor gives you and stop Googling. You’re making it worse.
Also, ‘Jules’? Who is Jules? This reads like a pharma ad written by a middle schooler.
Lauren Zableckis August 3, 2025
I think both drugs have their place. Lasix for emergencies. Torsemide for long-term. I’m not here to pick sides. I’m here to say: if you’re struggling, you’re not alone. And your experience matters. Keep talking. Keep tracking. Keep asking.
That’s how we get better.
Asha Jijen August 4, 2025
lasix is like your drunk uncle who shows up at parties and says the same thing every time
torsemide is that quiet cousin who shows up and fixes your wifi without you asking
and yes i know i spelled wifi wrong
but you get it right?
Edward Batchelder August 6, 2025
Thank you for writing this with such clarity and compassion. Many patients feel abandoned by the medical system when their symptoms persist despite adherence. This article validates their experience and empowers them to advocate for better care. I’ve shared this with my support group. The feedback has been overwhelmingly positive. Knowledge, as you rightly said, is not just power-it is peace.
Gayle Jenkins August 7, 2025
Someone mentioned Jules. That’s my mom. I wrote that part. She passed last year. But she got 3 more years of walking in the garden. That’s what this is about. Not drugs. Time.
Thank you for listening.